Research Article Open Access
Achieving Consistent, Homogeneous, Dark Fat Suppression on Bilateral Breast MRI at 3.0 Tesla in the Clinical Setting
Heather I Greenwood1*, Vignesh A Arasu1, Vibhas S Deshphande2, Dorota J Wisner3, Gerhard A Laub2, Nola M Hylton1 and Bonnie N Joe11Department of Radiology and Biomedical Imaging University of California, San Francisco School of Medicine, University of California, USA
2Siemens Medical Solutions USA, San Francisco, USA
3Kaiser San Rafael Medical Center, San Rafael, USA
- *Corresponding Author:
- Heather I Greenwood
Department of Radiology and Biomedical Imaging
San Francisco School of Medicine
University of California
1600 Divisadero St, Rm C-250
San Francisco, CA 94115, USA
Tel: 415-885-7464
Fax: 415-885-7876
E-mail: heather.greenwood@ucsf.edu
Received date: June 23, 2016; Accepted date: July 20, 2016; Published date: July 25, 2016
Citation: Greenwood HI, Arasu VA, Deshphande VS, Wisner DJ, Laub GA, et al. (2016) Achieving Consistent, Homogenous, Dark Fat Suppression on Bilateral Breast MRI at 3.0 Tesla in the Clinical Setting. OMICS J Radiol 5:230. doi: 10.4172/2167-7964.1000230
Copyright: © 2016 Greenwood HI, et al. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.
Visit for more related articles at Journal of Radiology
Abstract
Purpose: Effective fat suppression is a fundamental aspect of diagnostic quality breast MR for cancer screening but is challenging at 3T due to higher B0 and B1 magnetic field inhomogeneities compared with 1.5T. The purpose of this study is to describe a technique to achieve consistent homogeneous, dark fat suppression for T1 breast MR imaging at 3T for clinical breast cancer screening and evaluation. Methods: This was an IRB approved, HIPAA compliant study. Over 100 clinical breast MRI patients were scanned from May 2010 through October 2010, as part of routine clinical care, on a wide-bore 3T Magnetom Verio (Siemens Medical Solutions), One pre-contrast and two post-contrast axial VIBE scans were acquired for dynamic T1 imaging of the bilateral breasts. A longer TE of 4.9 ms was chosen empirically for optimal fat saturation. Two MQSA-certified breast radiologists, independently reviewed 20 consecutive MR studies. MR images were assessed for homogeneity of fat suppression and degree of fat suppression, both on a 5-point scale. A kappa coefficient was calculated for inter-reader agreement for both homogeneity of fat suppression and degree of fat suppression. Results: Overall, we found minimal unsuppressed fat and overall dark gray fat, indicating a high degree of fat suppression on 3T MR. Readers rated 3T fat suppression homogeneity as having minimal to no inhomogeneity in 80-90% of the examinations, with moderate agreement, (K=0.62, p<0.003), and fat suppression degree was rated having dark to very dark fat for all examinations with perfect agreement (K=1.0, p<0.001). Conclusion: Homogeneous, dark fat suppression on bilateral axial breast MRI can be obtained at 3.0T consistently in the clinical setting with minimal unsuppressed fat.
Keywords
Breast MRI; Fat Suppression; Breast cancer, Breast Imaging
Introduction
Homogeneous, dark fat suppression is a fundamental component of diagnostic- quality magnetic resonance imaging (MRI) for breast cancer screening and evaluation. The mainstay of clinical breast MRI protocols designed for cancer detection is the pre- and dynamic postcontrast T1 sequence. Because fat typically appears hyperintense on T1-weighted sequences, as does gadolinium, fat-suppression to make fat appear dark is essential to improve conspicuity of enhancing breast lesions. In addition to dynamic contrast-enhanced sequences, other breast MRI sequences such as T2 and diffusion-weighted sequences, require or benefit from effective fat suppression [1].
Several techniques are available for fat suppression on breast MRI, including frequency-selective fat suppression, Dixon techniques, and water suppression. Frequency-selective fat suppression, also known as chemical fat suppression, uses the difference in the precessional frequencies between protons in fat molecules versus those in water molecules, to selectively suppress frequencies associated with fat. This difference is 220 Hz at 1.5T and 440 Hz at 3T [2-4]. Although the fat water separation is wider at higher field strengths, uniform fat suppression is harder to obtain at higher magnetic strengths due to magnetic field inhomogeneities. Inhomogeneous fat suppression is readily identified as hyperintense areas of fat on fat-suppressed images.
The American College of Radiology (ACR) accreditation for breast MRI has several technical requirements, including the importance of using fat suppression. The ACR states that to detect and characterize small abnormalities on MRI, both high spatial and temporal resolutions are required. The ACR also states that chemical fat suppression is helpful when high-resolution images are obtained, to reduce fat signal while preserving the signal-to-noise ratio, thereby increasing the ability to detect cancer. Some protocols use fat suppression and a subtraction technique on sequences that are used to assess for contrast enhancement. Using only subtraction imaging to assess tumor enhancement may lead to misregistration if the patient moves during the MRI, which is very common given the long exam time. Thus, using fat suppression is recommended on sequences used to assess for contrast enhancement [5].
Inhomogeneous fat suppression can make breast MR interpretation challenging for the radiologist. If fat suppression is not homogeneous, both fat and tumors may appear bright, and tumors may be less conspicuous [3,6,7]. In addition, whenever there is inhomogeneous fat suppression there can also be associated water suppression, which causes black fibroglandular tissue. Water suppression can mask cancers because gadolinium enhancement cannot be detected in the areas affected by water suppression [4,7]. Therefore, homogeneous fat suppression is essential to detecting cancers on breast MRI. Finally, failure of fat suppression may lead to spurious results when using quantitative MR image analysis for lesion and stromal characterization [8,9].
Obtaining homogeneous, dark fat suppression on breast MRI is technically challenging for several reasons. First, the breast contains large amounts of fat with variable fat to fibroglandular tissue ratio and there must be a highly effective fat suppression technique to completely remove fat signal [1]. There are also relatively large fields of view required for bilateral breast coverage and individual right and left breasts are always located off of magnet iso-center. The breasts are surrounded by air, which causes local magnetic field (B0) inhomogeneity [1]. These technical challenges are greater at 3T because inherent B0 and B1 inhomogeneities are higher at 3.0T than at 1.5T. However, breast MRI at 3T is desirable, as it has several advantages over 1.5T. These advantages include improved spatial and temporal resolution, which leads to increased lesion conspicuity [1]. The real and perceived challenges of obtaining consistent, homogeneous fat-suppression comprise a practical barrier in the use of routine clinical breast MR at 3T, often overshadowing the potential advantages of the increased signal to noise at 3T. Thus, the purpose of this study was to describe a technique to achieve consistent homogeneous, dark fat suppression for T1 breast MR imaging at 3T during our early experience with 3T breast MRI in a clinical outpatient setting.
Methods
This HIPPA-compliant, retrospective study was approved by our institutional review board with waiver of requirement for informed consent for the retrospective review of images. Over 100 clinical patients were scanned from May to October 2010, as part of routine clinical care. We randomly chose 20 consecutive studies from the 100 total patients, performed from July 28, 2010 to October 29, 2010, to include in our reader study. Consecutive studies were chosen to avoid selection bias of choosing our “best work”.
MR technique
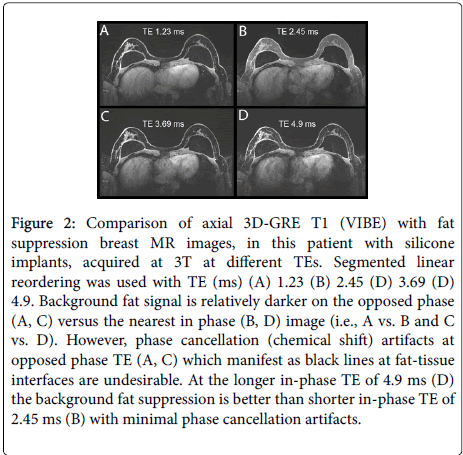
Breast MRI was performed on a wide-bore (70 cm) 3T Magnetom Verio (Siemens Medical Solutions, Erlangen, Germany) with a Sentinelle 8-channel breast coil (Hologic, Bedford, MA). One precontrast and two post-contrast 3 minute high resolution axial volumetric interpolated breath-hold examination (VIBE) scans were acquired for T1 imaging of bilateral breasts in the axial plane with patient in prone position. VIBE is a standard 3D T1-weighted gradient echo sequence. Contrast agent (Magnevist, Berlex) was injected using a power injector at 1.2 ml/sec with the start of the first post-contrast scan followed by a 20 cc saline flush at the same rate. Segmented linear reordering was used in the VIBE sequence in the partitions direction and linear reordering in the lines direction. The imaging parameters were as follows: Imaging time=3 min., resolution=0.73 × 0.73 × 1.6 (interpolated to 0.8) mm3, TR/TE=7.29 ms/4.9 ms, readout bandwidth=540 Hz/pixel, flip angle=12 deg., flip angle of fat suppression pulse=100 deg., lines per fat suppression pulse=24, interval between two fat suppression blocks=198.32 ms (24 excitation pulses: 23*7.29+15.69 ms), delay between saturation pulse and the first excitation pulse=10.46 ms, interval between successive excitation pulses=7.29 ms (TR), FOV 28-40 cm. A TE of 4.9 ms was chosen for water-fat in-phase behavior at 3T to minimize chemical shift artifact at fibroglandular tissue-fat interfaces. Moreover, we empirically chose a relatively long TE of 4.9 ms (the second “in-phase” TE at 3T) in this case for consistent and superior background fat suppression. During initial protocol optimization, we systematically tried the first and second in and out phase TEs at 3.0T. We found that the background fat signal exhibited lower signal at longer TE’s. A shorter T2* of the background, perhaps due to voxel contents with different resonant frequencies, is a likely reason for this signal suppression. An in-phase TE is not necessary, but preferable to minimize phase cancellation artifacts. Hence, we chose the second in-phase TE to maximize background signal suppression and minimize phase cancellation artifacts.
MR image assessment
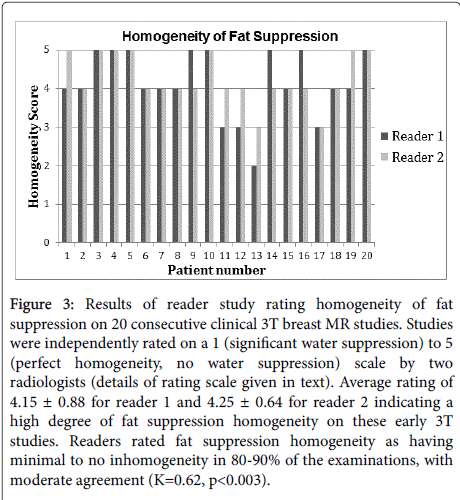
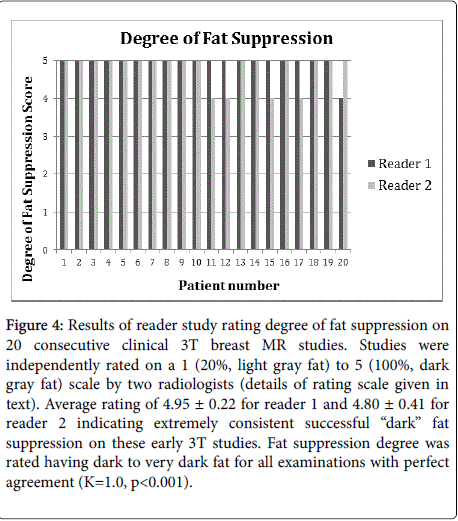
Two MQSA-certified breast imaging radiologists experienced in MRI independently reviewed 20 consecutive pre- and post-contrast clinical breast MR exams obtained during a three-month period early in our 3T breast MR experience (July 28, 2010 to October 29, 2010). All studies were performed and interpreted prospectively for routine clinical purposes. Patient age ranged from 38 to 68 years with mean of 53 years. Readers were blinded to all patient identity and MR exam and technical parameters. Each reviewed the cases in a different randomized order as presented by a researcher. Homogeneity of fat suppression was rated on a 5-point scale defined by the radiologists as follows: 1=Significant water suppression; 2=Some water suppression and/or significant amount of unsuppressed fat; 3=Moderate amount of unsuppressed fat, no water suppression; 4=Minimal unsuppressed fat, no water suppression; 5=Perfect homogeneity, no water suppression. Degree of fat suppression was also rated on a 5 point scale defined by the radiologists based on how light or dark gray the fat appeared relative to breast fibroglandular tissue where 1=20% (very light gray fat), 2=40% (light gray fat), 3=60% (gray fat), 4=80% (dark gray fat), 5=100% (very dark gray fat). For statistical analysis, a kappa coefficient was calculated for inter-reader agreement for both homogeneity of fat suppression and degree of fat suppression.
Results
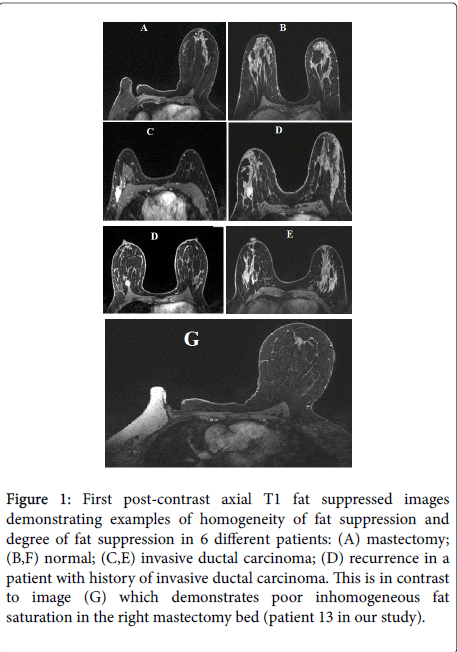
Overall, in the 20 consecutive clinical 3T breast MR studies, we found minimal unsuppressed fat and overall dark gray fat, indicating a high degree of fat suppression on 3T MR (Figure 1). When TE was varied and all other parameters were kept constant, a long TE of 4.9 provided better background suppression (likelyT2* relaxation) and minimal phase cancellation artifacts. With a TE of 1.23 ms (opposed phase) vs. a TE 2 of 0.45 ms (in phase) we saw the desirable darker background fat signal, but phase cancellation artifacts were problematic (Figure 2). For the 20 consecutive clinical 3T breast MR studies there was high homogeneity of fat, indicating overall minimal unsuppressed fat (Figure 3), as well as a high degree of fat suppression indicating extremely consistent successful “dark” fat suppression on these early 3T studies (Figure 4), as shown by both reader ratings. We found excellent inter-reader agreement and the majority of examinations were rated highly. Readers rated 3T fat suppression homogeneity as having minimal to no inhomogeneity in 80-90% of the examinations, with moderate agreement (K=0.62, p<0.003), and fat suppression degree was rated having dark to very dark fat for all examinations with perfect agreement (K=1.0, p<0.001).
Figure 1: First post-contrast axial T1 fat suppressed images demonstrating examples of homogeneity of fat suppression and degree of fat suppression in 6 different patients: (A) mastectomy; (B,F) normal; (C,E) invasive ductal carcinoma; (D) recurrence in a patient with history of invasive ductal carcinoma. This is in contrast to image (G) which demonstrates poor inhomogeneous fat saturation in the right mastectomy bed (patient 13 in our study).
Figure 2: Comparison of axial 3D-GRE T1 (VIBE) with fat suppression breast MR images, in this patient with silicone implants, acquired at 3T at different TEs. Segmented linear reordering was used with TE (ms) (A) 1.23 (B) 2.45 (D) 3.69 (D) 4.9. Background fat signal is relatively darker on the opposed phase (A, C) versus the nearest in phase (B, D) image (i.e., A vs. B and C vs. D). However, phase cancellation (chemical shift) artifacts at opposed phase TE (A, C) which manifest as black lines at fat-tissue interfaces are undesirable. At the longer in-phase TE of 4.9 ms (D) the background fat suppression is better than shorter in-phase TE of 2.45 ms (B) with minimal phase cancellation artifacts.
Figure 3: Results of reader study rating homogeneity of fat suppression on 20 consecutive clinical 3T breast MR studies. Studies were independently rated on a 1 (significant water suppression) to 5 (perfect homogeneity, no water suppression) scale by two radiologists (details of rating scale given in text). Average rating of 4.15 ± 0.88 for reader 1 and 4.25 ± 0.64 for reader 2 indicating a high degree of fat suppression homogeneity on these early 3T studies. Readers rated fat suppression homogeneity as having minimal to no inhomogeneity in 80-90% of the examinations, with moderate agreement (K=0.62, p < 0.003).
Figure 4: Results of reader study rating degree of fat suppression on 20 consecutive clinical 3T breast MR studies. Studies were independently rated on a 1 (20%, light gray fat) to 5 (100%, dark gray fat) scale by two radiologists (details of rating scale given in text). Average rating of 4.95 ± 0.22 for reader 1 and 4.80 ± 0.41 for reader 2 indicating extremely consistent successful ��?dark� fat suppression on these early 3T studies. Fat suppression degree was rated having dark to very dark fat for all examinations with perfect agreement (K=1.0, p < 0.001).
Discussion
In this study, we investigated whether we could achieve consistent, homogenous, fat suppression on 3T breast MRI. The results of this reader study show that under clinical conditions the technique for the T1 dynamic breast MR imaging at 3T that we describe offers excellent fat suppression with consistent homogeneity and minimal unsuppressed fat with consistent dark gray appearance of fat relative to fibroglandular tissue. Suppressing the fat signal adequately improves the sensitivity of breast MRI by increasing conspicuity of breast lesions, importantly breast cancers. Improving homogeneity is important to reduce areas of poor fat suppression, which can distract from cancer detection. Since the time of this study we have successfully performed over 2000 breast MRI exams using this technique at 3T which has become our standard clinical T1 pre- and post-contrast sequence.
There are a variety of other fat suppression techniques available including fat saturation, water suppression and Dixon techniques. Fat saturation and water excitation are both very sensitive to B0 and B1. There is substantial B0 variation across the FOV in breast MR, especially when imaging axially. In addition, there are also substantial local field inhomogeneities due to air-tissue interfaces that may lead to the loss of fat suppression locally. At 3T, there could also be B1 variations that may lead to inconsistent fat suppression. Finally, in vivo fat shows multiple frequencies in the spectrum, which may not all be suppressed with a fat suppression pulse, or eliminated by water excitation.
One issue with Dixon methods is that the early in and out-of-phase echoes need to be sampled for a robust separation, use of later echoes makes the fat-water separation more challenging. Sampling both early echoes in the same TR limits the spatial resolution, due to maximum gradient amplitude limitations. Dixon methods are less prone to B0 problems compared to the fat suppression and water suppression methods, but may not be completely immune to the same. With large local variations, there is potential for fat-water swaps, but this is a topic of research and as the Dixon algorithms improve, it is likely that this may not be an issue.
Ultimately, our approach was chosen mainly because of its robustness to patient and scanner variations. The method relies on using a fat suppression pulse to reduce the fat signal, but also uses the T2* related signal loss with a longer TE to achieve uniform and robust background suppression. This is a simple method that can be implemented on any clinical scanner and works robustly.
We used an increased TE in this study to achieve consistent, homogenous fat suppression on 3T breast imaging. One effect of using this is signal loss around metal/clips. In general, the T2* weighting will act to reduce the enhanced-unenhanced tissue contrast that the T1 tries to increase. This is because the T2* of Gadolinium enhanced tissue will be higher than that of unenhanced tissue, and hence reduce the signal of the enhanced tissue at a faster rate. However, based on the results, the T1 enhancement is still the dominant factor in tissue contrast, and this compromise of slightly increased T2* loss seems to be a good one, in order to achieve robust background suppression.
A limitation of using linear k-space reordering is sensitivity to motion artifact. At the time of this study, we were using a 3-minute sequence in order to achieve higher spatial resolution with the tradeoff that a longer sequence would be more susceptible to any motion artifact within the three-minute period. Currently, we employ a shorter, 100 second sequence which is less sensitive to motion artifact and we are able to maintain the same spatial resolution with use of parallel imaging techniques and a 16-channel breast coil (not available at time of this study).
A limitation of retrospective studies is potential selection bias. We tried to avoid selection bias by choosing 20 consecutive cases shortly after our radiologists agreed upon a clinical protocol. Another limitation of this study is that we could not simultaneously look at lesion conspicuity or contrast enhancement of lesions given the low frequency of these findings. However, we expect that homogeneous fat suppression in breast MRI leads to increased lesion conspicuity, and that homogeneous fat suppression is more challenging at 3T than at 1.5T.
Conclusion
In conclusion, we have been able to achieve homogeneous, dark fat suppression on bilateral breast MRI at 3T consistently in the clinical setting using the described sequence. Overall we found minimal unsuppressed fat and overall dark gray fat indicating a high degree of fat suppression on 20 consecutive cases soon after launching our 3.0T breast MRI program. Homogeneous, dark fat suppression on bilateral axial breast MRI at 3.0T is achievable using a long TE VIBE sequence.
Acknowledgements
• Grant #IRG-97-150-10 from the American Cancer Society.
• Grant from the University of California Cancer Research Coordinating Committee.
References
- Chen L, Rogers CD, Majidi S (2016) Fat Suppression techniques in breast magnetic resonance imaging: a critical comparison and state of the art.Dovepress 8: 37-49.
- Hendrick ER (2008) Breast MRI fundamentals and technical aspects (1stedn.) NY: Springer, New York.
- Ojeda-Fournier H, Choe KA, Mahoney MC (2007) Recognizing and interpreting artifacts and pitfalls in MR imaging of the breast. Radiographics 27:147-164.
- Yitta S, Joe BN, Wisner DJ, Price ER, Hylton NM (2013) Recognizing artifacts and optimizing breast MRI at 1.5 and 3 T. AM J Roentgenol200:673-682.
- Mahoney MC, Newell, MS Bailey L (2013) ACR Practice Parameter for the Performance of Contrast Enhanced Magnetic Resonance Imaging (MRI) of the Breast.
- Harvey JA, Hendrick RE, Coll JM, Nicholson BT, Burkholder BT, et al. (2007) Breast MR imaging artifacts: how to recognize and fix them. Radiographics27:131-145.
- Rausch DR, Hendrick RE (2006) How to optimize clinical breast MR imaging practices and techniques on your 1.5T system. Radiographics 26:1469-1484.
- Aliu SO, Jones EF, Azziz A, Kornak J, Wilmes LJ, et al. (2014)Repeatability of quantitative MRI measurements in normal breast tissue. TranslOncol7:130-137.
- McLaughlin RL, Newitt DC, Wilmes LJ, Jones EF, Wisner DJ, et al. (2014)High resolution in vivo characterization of apparent diffusion coefficient at the tumor-stromal boundary of breast carcinomas: a pilot study to assess treatment response using proximity-dependent diffusion-weighted imaging. J MagnReson Imaging 39:1308-1313.
Relevant Topics
- Abdominal Radiology
- AI in Radiology
- Breast Imaging
- Cardiovascular Radiology
- Chest Radiology
- Clinical Radiology
- CT Imaging
- Diagnostic Radiology
- Emergency Radiology
- Fluoroscopy Radiology
- General Radiology
- Genitourinary Radiology
- Interventional Radiology Techniques
- Mammography
- Minimal Invasive surgery
- Musculoskeletal Radiology
- Neuroradiology
- Neuroradiology Advances
- Oral and Maxillofacial Radiology
- Radiography
- Radiology Imaging
- Surgical Radiology
- Tele Radiology
- Therapeutic Radiology
Recommended Journals
Article Tools
Article Usage
- Total views: 12930
- [From(publication date):
August-2016 - Mar 29, 2025] - Breakdown by view type
- HTML page views : 12035
- PDF downloads : 895