Review Article Open Access
Achalasia Cardia Recent Advances in Diagnosis and Endoscopic Management
Zaheer Nabi* and Duvvur Nageshwar ReddyAsian Institute of Gastroenterology, Hyderabad, Telangana, India
- *Corresponding Author:
- Zaheer Nabi
Consultant, Asian Institute of Gastroenterology
Gastroenterology, 6-3-661, Somajiguda
Hyderabad, Telangana 500082, India
Tel: 919573058810
E-mail: zaheernabi1978@gmail.com
Received date: October 21, 2015; Accepted date: January 11, 2016; Published date: January 20, 2016
Citation: Nabi Z, Reddy DN (2016) Achalasia Cardia – Recent Advances in Diagnosis and Endoscopic Management. J Gastrointest Dig Syst 6:393. doi:10.4172/2161-069X.1000393
Copyright: © 2016 Nabi Z, et al. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.
Visit for more related articles at Journal of Gastrointestinal & Digestive System
Abstract
Achalasia Cardia is a rare neurodegenerative disorder of esophagus resulting in defective peristalsis and impaired relaxation of lower esophageal sphincter. The exact etiopathogenesis of achalasia is not known. Achalasia is associated with significant morbidity and impaired quality of life. The standard of care in patients with achalasia has been pneumatic balloon dilatation and laparoscopic heller's myotomy. Recent advancements in the diagnosis and endoscopic management have greatly improved the outcomes of this disorder. Subtyping of esophageal motility disorders with high resolution manometry has served to predict treatment outcomes and plan appropriate treatment. Per oral endoscopic myotomy (POEM) is an novel minimally invasive treatment option for all types of achalasia cardia. Short and mid term efficacy are excellent. Randomized trials are required to confirm its superiority over the currently established treatment modalities.
Keywords
Achalasia cardia; Per oral endoscopic myotomy; High resolution manometry; Timed barium esophagogram
Introduction
Achalasia Cardia (AC) is a primary motility disorder of the esophagus characterized by aperistalsis and defective lower esophageal sphincter relaxation. The pathogenesis of AC is poorly understood. However recent evidences indicate that it is an autoimmune process trigerred by some virus (e.g herpes virus) in a genetically predisposed individual resulting in degeneration of myenteric neurons [1].
Achalasia is a rare disease and therefore the epidemiological data on its incidence and prevalence is limited. The incidence and prevalence of AC in population studies is 0.31-1.63 and 6.29-10.82 per 105 population respectively [2-6]. The standard of endoscopic management has been graded pneumatic balloon dilatation and botox injection in selected high risk cases. Recent advances in the diagnosis as well as endoscopic management of AC have improved the outcomes significantly.
Diagnosis and Prediction of Outcomes
The diagnosis of AC relies on high resolution esophageal topography and endoscopy. Barium swallow supplements the diagnosis and is an objective parameter for documenting esophageal emptying after any therapeutic intervention. The main role of gastroscopy is to rule out other causes of dysphagia, especially pseudoachalasia due to gastroesophageal junction neoplasms.
High Resolution Manometry and High Resolution Impedance Manometry
High resolution manometry (HRM) has largely replaced conventional manometry for the diagnosis of AC and other motility disorders of esophagus. In HRM the pressure sensors are closely spaced (1 cm intervals) so that the esophageal pressure is depicted as a continuum in real time. HRM is the diagnostic modality of choice for AC and other non-achalasia motility disorders of esophagus. Chicago Classification (CC) of esophageal motility disorders is widely accepted for the subtyping of AC and defining other esophageal motility disorders of esophagus [7].
With HRM, three subtypes of AC have been identified (Type I, II, III) [8,9]. Subtyping of AC into three types has prognostic significance as well. Type II AC (panesophageal pressurisation) responds best to any form of treatment (botox injection, pneumatic dilatation, heller’smyotomy), whereas type I AC does not respond as well and type III is the most resistant to treatment [8,9]. The response rate to pneumatic balloon dilatation (PBD) in one study was 90.0% for type II AC as compared to 63.3% for type I and only 33.3% for type III AC [8]. There is some evidence that Type III AC responds better to myotomy than pneumatic dilatation (86% vs. 40%) [10]. Therefore, HRM may also help in deciding the optimum modality of treatment.
HRM can also predict the probability of recurrence after treatment (like PBD). A post dilatation lower esophageal sphincter (LES) pressure of <10 mmHg or >50% reduction in LES pressure from baseline is a predictor of good outcome and less chances of recurrence [11,12]. Esophageal HRM has been found to be equivalent to timed barium esophagogram (TBE) in assessing the efficacy of PBD in treatment of achalasia [13]. The normalization of integrated relaxation pressure (IRP) correlates well with TBE and has been found to be a valid objective point in treatment of AC [14].
Moreover, high-resolution impedance manometry (HRIM) can be used as a single test to determine bolus retention (like in TBE) and motility function in the management of achalasia [15]. The measurement of bolus flow time (BFT) by HRIM is an useful adjunct to integrated relaxation pressure (IRP) in the diagnosis of AC [16].
Therefore, HRM is an indispensable tool in the diagnosis and management of patients with AC and other esophageal motility disorders.
Timed Barium Esophagogram
Timed barium esophagogram (TBE) is an objective way to determine esophageal emptying. In TBE a fixed quantity (about 200-250 ml) of low density barium (45%) is ingested and films are taken at predefined intervals (1, 2 and 5 minutes) [17]. TBE has an important role in predicting treatment failure and symptom relapse in patients treated for achalasia (Figures 1 and 2). In a randomized trial, Andersson et al (2009) showed that in patients with less than 50% improvement in height of barium column at 1 min, the chance of failure was high (40%) during follow-up [18].
After a procedure, TBE is better than symptom relief or LES pressure in predicting future relapse [19-21]. In one study, Vaezi et al. (2002) found that about 30% of AC patients treated with PBD reported good immediate symptom relief despite poor esophageal emptying (<50%) on TBE. However, 90% of these patients relapsed within 1 year of follow up [19,20]. Therefore TBE identifies an important subgroup of patients who need close follow up or early re-treatment despite symptom control.
Endoluminal Functional Lumen Imaging Probe (EndoFLIP)
EndoFLIP works on the principle of impedence planimetry and allows the measurement of gastroesophageal junction (GEJ) distensibility in real time. GEJ diameter, cross sectional area and distensibility (calculated by dividing minimum cross-sectional area at the GEJ by pressure) can be measured with this novel technique. As expected, GEJ distensibility and cross sectional area increase substantially after successful treatment in patients with AC. The proposed advantage of this technique is that the adequacy or completeness of myotomy (endoscopic or heller) can be determined during the procedure. Establishing the adequacy of myotomy may be challenging during per-oral endoscopic myotomy (POEM). EndoFLIP may be useful in this regard as myotomy can be extended, if GEJ distensibility is inadequate [22].
The evidence for utility of endoFLIP in identifying the effect of myotomy on GEJ physiology is gradually building up [23-25]. The measurement of GEJ distensibillity by endoFLIP may be a better parameter than LES pressure to evaluate the efficacy of treatment in AC [24].
Teitelbaum et al. (2015) studied the effect of extent of myotomy on EndoFlip and concluded that extension of myotomy for 2 cm across GEJ normalizes GEJ distensibility during POEM. However, further extension of myotomy onto the gastric side (upto 3 cm) did not result in incremental compliance [25]. Therefore, EndoFLIP appears a promising novel innovation in assessing the success of endoscopic or surgical myotomy. However, more studies with long term follow up are required to assess the impact of this technique on the management of AC.
Management of Achalasia Cardia
AC can be managed but not cured. Since the initial description of AC in 1674 by Sir Thomas Willis, various endoscopic and surgical treatment modalities have been developed and modified from time to time. However, all of them aim to reduce the GEJ or LES pressure and none of these modalities can bring back the normal motility of esophageal body. This is because the degeneration of myenteric neurons, due to yet poorly understood reasons, underlies the pathogenesis of AC and cannot be reverted back with the currently available treatment options.
Botulinum Toxin Injection
Botolinum toxin injection (BI) has been in use for years now for AC. The proposed advantages being safety and good short term outcomes (>75%). However, the disadvantage being poor long term efficacy (35-41% at 1 year) [26].
Currently BI is used in specific patient groups (e.g high surgical risk, vigorous achalasia) who are not fit for pneumatic balloon dilatation (PBD) or myotomy. There is a renewed interest in the use of BI for non-achalasia esophageal motility disorders like diffuse esophageal spasm (DES) and nutcracker esophagus (NE). Vanuytsel et al. (2013) demonstrated the utility of BI in DES and NE in a prospective, doubleblind, randomized, controlled study. The authors used BI at two levels of esophagus (2 and 7 cm above GEJ) in this study. The response rate (improvement in dysphagia) at 1 month and 1 year was 50% and 30% respectively [27]. Therefore, BI may be especially useful in these patients who are otherwise difficult to treat.
Pneumatic Balloon Dilatation
Pneumatic Balloon Dilatation (PBD) is the standard of non surgical management of AC. Non compliant polyethylene balloons (Rigiflex, Boston Scientific) are used under fluoroscopic guidance to stretch LES. Graded dilatation is recommended to get the best results with PBD [26]. Dilatation is started with a 30 mm balloon with subsequent dilatations done with 35 and 40 mm balloons in case of symptom relapse or esophageal stasis on TBE. Older age (>40 years) and type II AC are predictive factors for good response [8-10]. The efficacy of PBD is comparable to heller’smyotomy at 2 years follow up (86% vs. 90%) [28]. The most feared complication of PBD is perforation which occurs in about 2-4% of cases. Risk factors for PBD related perforations include – age >65 years and initial dilatation with a larger balloon. However, most of these perforations can be managed conservatively [29,30].
Laparoscopic Heller Myotomy (LHM)
Heller myotomy has evolved and developed over time since its introuction more than a hundred years ago. To begin with, both an anterior and posterior myotomies were performed via abdominal approach [31]. Subsequently, myotomy via transthoracic route gained transient acceptance [32]. Difficulty in reaching on to the anterior wall of gastric cardia leading to insufficient myotomy is one of the major drawbacks with thoracoscopic approach.
With the advent of laparoscopic approach, the morbidity minimized significantly and LHM was accepted as the standard of surgical management for AC. However, worrisome gastroesophageal reflux remained a trouble. A limited myotomy (especially on the gastric side) would minimize reflux, but the chances of recurrent dysphagia would be high. In its current form, LHM is combined with partial posterior (Toupet) or anterior (Dor) fundoplication to limit GER and myotomy is extended to 6 cm on esophageal side and 3 cm on gastric side to limit occurrence of recurrent dysphagia [33]. Long term (≥5 years) success rates reported with LHM are 80-84% [34]. LHM has been found to be comparable to PBD (at 5 years) in the European achalasia trial. However a quarter of PBD patients required redilations on follow up [35].
Per Oral Endoscopic Myotomy (POEM)
Endoscopic myotomy was first described by Ortega and colleagues in 1980 [36]. Although the authors described the procedure as fast, safe and effective, it did not gain widespread acceptance because of the fear of complications like mediastinitis and perforation.
The development of NOTES reopened the doors of minimally invasive treatment for AC. Sumiyama and colleagues (2008) described a technique to safely access the peritoneal and mediastinal cavity. The principle of POEM is based on this technique called as submucosal endoscopy with mucosal flap safety valve technique [37].
Pasricha et al. (2007) first described the feasibility of submucosal endoscopic esophageal myotomy in a porcine model [38]. Subsequently Inoue et al. (2009), performed the first human submucosal endoscopic myotomy and coined the term POEM for this technique [39]. Since then a large number of studies have been published demonstrating the safety and efficacy of POEM in AC [40-52].
POEM – Technique
POEM is performed under general anaesthesia with the patient in supine position. The standard equipment or accessories used for POEM include – a high definition endoscope with water jet facility, transparent cap (Olympus), CO2 insufflator (UCR; Olympus), triangletip knife (Olympus) or hybrid knife T type (ERBE, Tübingen, Germany), coagulating forceps (Coagrasper, Olympus) and hemostatic clips.
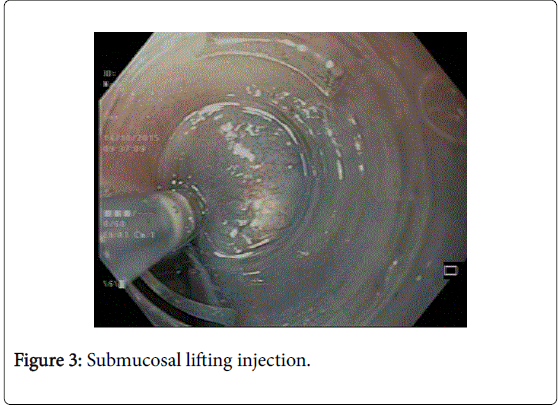
The first and most important step is lifting the mucosa away from submucosa by injecting solution made of saline mixed with indigocarmine dye (Figure 3). This area is usually chosen about 10-15 cm proximal to GEJ. A good lift makes the next step of entry into submucosal tunnel easier.
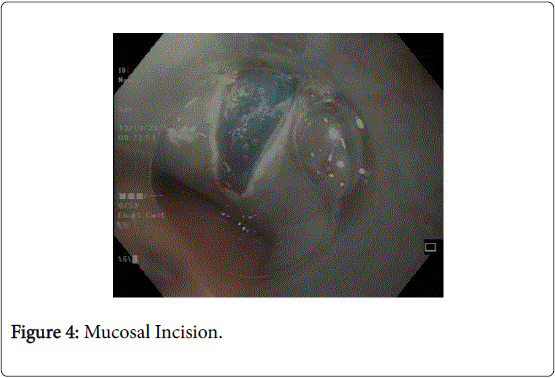
The next step involves making a mucosal incision and clearance of submucosal fibres to make way for the entry of gastroscope (Figure 4). Initially a small (3-4 mm) mucosal incision is made using a needle knife and subsequently the incision is enlarged by an insulated tip knife (Olympus) up to 2 cm in length [40].
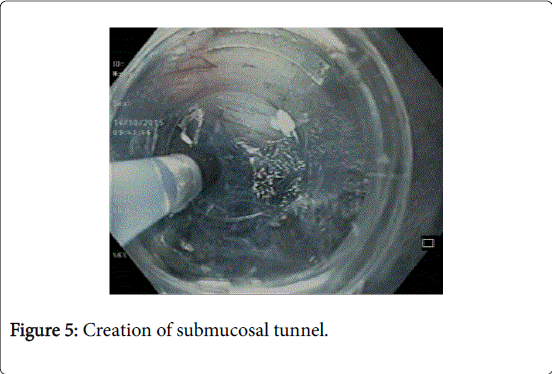
In the third step, submucosal tunnel is created by using triangular tip or hybrid knife (Figure 5). Any intervening vessels are coagulated using the coagulation forceps (Figures 6a and 6b). The submucosal tunnel should extend to at least 2 to 3 cm beyond GEJ onto the gastric side for good relief. Adequate extension of tunnel can be confirmed by retroflex viewing of the gastric cardia and identifying the bluish discoloured area.
Myotomy is then performed, starting from 2 to 3 cm distal to the mucosal incision site (safety mucosal flap) (Figure 7).
Either circular only myotomy or full thickness myotomy (both circular and longitudinal muscles) can be performed.
The authors perform circular only myotomy in the proximal part and full thickness myotomy in the lower part of esophagus (from 2-3 cm proximal to GEJ till the end of submucosal tunnel).
In the final step mucosal incision is closed using standard hemostatic clips (Figure 8). It is important to carefully inspect the esophageal mucosa for any inadvertent injury or perforation before closing the mucosal incision. After the procedure, patients are kept nil per oral for about 24 hours. A timed barium esophagogram is performed about 24 hours later and oral liquids are started subsequently.
POEM – Variation in Techniques
POEM can be performed by an anterior (2’oclock) or posterior (5’ oclock) approach. Lower esophageal sphincter is asymmetric and consists of semicircular clasp like fibres on the right (centred at 2 O’clock) and oblique sling fibres on the left (5 to 11 O’clock) side of the esophagus. Therefore, in anterior myotomy only the clasp fibres are divided, whereas in posterior approach both the clasp and sling fibres are cut. A limited myotomy of the clasp fibres may not completely abolish the competency of GE junction due to persistent action of sling fibres [41]. Therefore, theoretically speaking a posterior approach should give better results in terms of symptom response. However, randomized control trials are required to demonstrate any clinically relevant differences in anterior vs. posterior myotomy. The authors prefer a posterior approach in patients with history of prior laparoscopic heller’smyotomy (LHM) or in case a diverticulum is present along the anterior esophageal wall.
Other variations in endoscopic myotomy include – full thickness vs. circular myotomy and short vs. long myotomy. Limited data suggests that there is no difference in the clinical outcomes and complications between full thickness vs. circular only myotomy. However, the procedure time may be shorter for full thickness myotomy [42,43].
Tang et al (2015), compared short myotomy (<7 cm) to long myotomy (>7 cm). Short term clinical efficacy were similar in the two groups and the procedure time shorter in the former group [44]. However, randomized trials are required before applying the results of this study into clinical practice. A shorter myotomy may be sufficient for type II AC, whereas a long myotomy is necessary for vigorous achalasia (type III) and other non-achalasia spastic disorders like DES and nutcracker esophagus.
At this point, the available evidence is limited to advocate any one technique over the other and future studies are required to demonstrate clinically relevant differences between various tecniques.
POEM – Efficacy and Complications
The efficacy and safety of POEM has been established in numerous retrospective and prospective studies (Table 1) [45-52]. In a study by Ramchandani et al (2015), including over 200 patients with AC, the technical success rate of POEM was 96%. At 1 year, clinical success rate was 92%. There was significant improvement of esophageal emptying on TBE (38.4 ± 14.0% vs. 71.5 ± 16.1% (P=0.001) and mean lower esophageal sphincter pressure (37.5 ± 14.5 mmHg vs. 15.2 ± 6.3 mmHg, P=0.001). There were no major adverse events [45].
| n | Efficacy (%) | Follow up | |
| Ren et al. [39] | 119 | 92 | 10.4 |
| Inoue et al. [40] | 500 | 89 | 36 |
| Zhou et al. [41] | 205 | 97 | 8.5 |
| Ramchandani et al. [38] | 220 | 92 | 12 |
| Werner YB et al. [42] | 80 | 80 | 29 |
| Sharata et al. [43] | 100 | 97 | 16 |
Table 1: POEM – efficacy in selected studies.
POEM is a safe procedure and till date no death has been reported related to this procedure. Intraprocedural events include – gas related (pneumothorax, capnoperitoneum, subcutaneous emphysema), mucosal injury, premature muscle injury and bleeding (Table 2). However, these events rarely proceed to clinically significant adverse events and no mortality has been observed due to any of these events [45-47,50-52].
| N | Perforation | Mucosal Inj | Bleed | Gas Related | |
| Ren et al. [39] | 119 | 0.80% Tunnel entry dehiscence | NA | 0.80% | Pneumothorax -25 % |
| Emphysema-55 % | |||||
| Pneumoperitoneum -39 % | |||||
| Von Renteln et al. [44] | 70 | 1% | 4% | 1 %, 1 % delayed bleed | Emphysema 37 % |
| Pneumoperitoneum 50 % | |||||
| Sharata et al. [43] | 100 | 3% | NA | 1% | 1% |
| Inoue et al. [40] | 500 | 0.40% | 1.20% | 0.2 % - intra-operative | 0.20% |
| 0.6 %- post-operative | |||||
| Ramchandani et al. [38] | 225 | NA | 6.30% | NA | Pneumothorax -1.3 % |
| Emphysema- 14.2 % | |||||
| Pneumoperitoneum - 25 % | |||||
| Stavropoulos et al. [45] (Ipoems ) | 841 | 6.70% | NA | 1% | 8.30% |
Table 2: Adverse events related to POEM.
POEM - Comparison with Other Treatment options
POEM is an evolving technique with impressive short term results. Good outcomes with POEM demand its comparison with already established techniques like PBD and LHM. Unfortunately, there is no randomized trial till date comparing POEM with other treatment modalities for AC. Limited data suggests that the efficacy of POEM is comparable to laparoscopic heller’smyotomy (LHM) in patients with AC [53,54]. The post-procure pain, intra-operative blood loss, and procedure time are less and return to normal activities faster with POEM as compared to LHM [55,56].
Another advantage of POEM over LHM is that longer myotomies can be performed easily as may be required in some patients with DES, jackhammer esophagus and type III AC [57]. A multicenter study compared POEM to LHM in patients with type III AC. Clinical response was significantly better, length of myotomy longer and adverse events significantly lower in the POEM group. The authors attributed better response rates with POEM to the ability to perform longer myotomies than LHM [57].
POEM in Special Population (Failed cases, Sigmoid Achalasia, Pediatric achalasia)
POEM has been successfully performed in previously failed cases (PBD, Botox inj. Or LHM). Studies show that there is no difference in the efficacy between treatment naïve or prior failure cases [58-61]. Moreover, re-POEM can be performed in patients who fail to respond with initial POEM [62].
Sigmoid esophagus is regarded as an advanced stage of AC and treatment outcomes with the standard modalities are not as good. POEM is feasible and safe with good short term results in sigmoid type AC [63].
The other population group which is difficult to treat is pediatric AC. LHM is the current gold standard for children with AC. There is growing evidence that POEM is safe and effective in this group also [64,65].
Self Expanding Metal Stents (SEMS)
SEMS are commonly used for benign or malignant esophageal strictures. Covered SEMS are removable and have steady radial expanding force. This lead some authors to study the utility of covered SEMS in AC [66-68]. In a recent study, fully covered SEMS (diameter of 2.0-2.5 cm and length of 5-7 cm) was used in fifty nine patients with AC. The stents were subsequently removed at 1 month. Clinical remission was 82% at 1 year and 49% at 3 years. There were no major adverse events [66].
SEMS have been shown to be superior to botulinum toxin injection and PBD [67,68].
However, the time is not yet ripe for the use of SEMS and more data is required before they can be recommended for AC.
Management of Achalasia – The Individualized Approach
The management of achalasia needs to be tailored according to the subtype of AC on HRM as well as the phenotype of patients. Young patients (<35-40 years) do not respond as well to PBD as their older counterparts [69].
Therefore, they should be preferably managed with LHM or POEM. Similarly in patients with type III achalasia or other spastic esophageal disorders, POEM or LHM should be preferred to PBD for similar reasons. POEM may be especially useful in this subgroup of patients as longer myotomies can be easily performed as compared to LHM [70]. More studies are required to assess and compare the efficacy of myotomy and pneumatic dilatation in each subtype of AC (Table 3).
| PBD | LHM | POEM | |
| Type I AC | 63.3-85%8,10 | 81%10 | 91.4%* |
| Type II AC | 90-93%8,9,10 | 93-100%9,10 | 93.6%* |
| Type III AC | 33.3-40%8,10 | 80-86%10,57 | 98%57 |
| Overall Efficacy | 44-84%35 | 57-89.3%35,71,74 | 80-97%45-50 |
| Follow up (yrs) | ≥5 years | ≥5 years | 1-3 years |
| GER | 4%74 | 9-33%71 | 15-30%47,50,52,54 |
Table 3: Comparison of efficacy according to AC subtype. AC =achalasia cardia, PBD: Pneumatic Balloon Dilatation, POEM: Per Oral Endoscopic Myotomy, GER: Gastroesophageal reflux. *Study in Abstract form (Tang X et al. Volume 81, No. 5S: 2015 GASTROINTESTINAL ENDOSCOPY AB493).
Success rates of myotomy (endoscopic or surgical) may increase with the use of EndoFlip which will help in deciding the optimal length of myotomy intra-operatively. Timed barium esophagogram should be performed postprocedure, irrespective of the treatment modality used (LHM, PBD or POEM). It is an excellent predictor of future relapse, even if clinical symptoms are apparently absent [19].
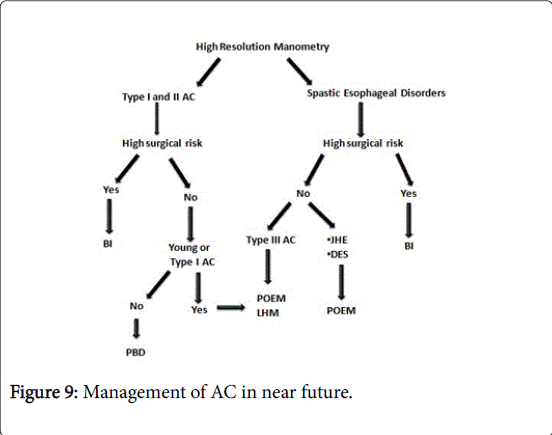
Unfortunately, POEM has still not made its place in the management algorithms and guidelines on AC [26]. Excellent safety and efficacy of POEM in recent studies can not be ignored and it should find a definite place in the management of AC in near future (Figure 9).
Long Term Follow up and Surveillance - Why and How
Achalasia cardia is not curable because the currently available treatments do not restore the myenteric neurons which disappear over time. Moreover relapses are well known with the present treatment options (especially PBD and BI). Untreated relapses may lead to end stage achalasia for wchich esophagectomy may be required which carries significant morbidity. Therefore, regular follow up is required for these patients after treatment. Both, HRM and TBE have been utilized to follow these patients. TBE is non invasive and probably better than HRM for predicting future relapses. However, the frequency of performing the same is not known. Whether TBE should be performed at regular intervals (e.g. 6-12 monthly) after the procedure is a matter of debate. Arguments in favour include significant stasis and risk of disease progression in the absence of symptoms in some patients after the procedure. Early management will prevent the development of end stage achalasia. However, the strategy of treating patients solely on the basis of barium stasis on TBE in the absence of symptoms has not been formally tested. Nevertheless, this is a small subgroup of patients and routine TBE may not be justified in all. TBE at regular intervals may not be required in patients who have undergone LHM or POEM especially if intra-operative EndoFlip shows good relaxation and post procedure TBE shows good esophageal emptying. However, young patients and those with type I/III AC opting for PBD, require close surveillance and TBE at regular intervals may have some role.
In addition to disease relapse, additional reasons to follow the patients with AC include post treatment gastroesophageal reflux and risk of esophageal carcinoma [71-73].
Gastroesophageal reflux (GER) is a common occurrence after LHM and POEM. The incidence of GER ranges from 9-33% with LHM and 20-30% with POEM [71,72]. However, the reflux is usually mild and easily controlled with lifestyle modifications and proton pump inhibitors.
Achalasia cardia predisposes to esophageal malignancy due to chronic stasis and mucosal irritation. The long term risk of esophageal malignancy in primary AC was 3.3% (~70% males) in one study. Unfortunately only 1/3rd of them could undergo potential curative treatment [74].
It is not easy to differentiate between dysplastic lesions from the changes of stasis esophagitis that are commonly present in patients with AC. Therefore, the utility of surveillance endoscopy in AC is not well known and there is no consensus over the same. Whether the screening of selected high risk cases (e.g older men, >10 years of disease) and use of narrow band imaging or lugol’s iodine will improve the outcomes of screening remains to be seen.
Summary
Achalasia cardia is a rare neurodegenerative disease with significant morbidity. Recent advances in the diagnosis and management of AC have significantly improved the outcomes. High resolution manometry allows for the subtyping of AC and helps in guiding treatment plan. New diagnostic modalities like EndoFLIP allow intra-operative assessment of adequacy of myotomy. POEM is an novel endoscopic treatment option for AC. Short and midterm results with this technique are promising. However randomized trials are required to establish its superiority over other established modalities of treatment like LHM and PBD.
References
- Gockel I, Becker J, Wouters MM, Niebisch S, Gockel HR, et al. (2014) Common variants in the HLA-DQ region confer susceptibility to idiopathic achalasia. Nat Genet 46: 901-904.
- Sadowski DC, Ackah F, Jiang B et al. Achalasia: incidence, prevalence and survival. A population-based study.NeurogastroenterolMotil. 2010 Sep;22(9):e256-61.
- Kim E, Lee H, Jung HK, Lee KJ (2014) Achalasia in Korea: an epidemiologic study using a national healthcare database. J Korean Med Sci 29: 576-580.
- Mayberry JF, Atkinson M (1985) Studies of incidence and prevalence of achalasia in the Nottingham area. Q J Med 56: 451-456.
- Birgisson S, Richter JE (2007) Achalasia in Iceland, 1952-2002: an epidemiologic study. Dig Dis Sci 52: 1855-1860.
- Farrukh A, DeCaestecker J, Mayberry JF. An epidemiological study of achalasia among the South Asian population of Leicester, 1986-2005.Dysphagia. 2008 Jun;23(2):161-4.
- Kahrilas PJ, Bredenoord AJ, Fox M, Gyawali CP, Roman S, et al. (2015) The Chicago Classification of esophageal motility disorders, v3.0. Neurogastroenterol Motil 27: 160-174.
- Pratap N, Kalapala R, Darisetty S, Joshi N, Ramchandani M, et al. (2011) Achalasia cardia subtyping by high-resolution manometry predicts the therapeutic outcome of pneumatic balloon dilatation. J Neurogastroenterol Motil 17: 48-53.
- Pandolfino JE, Kwiatek MA, Nealis T (2008) Achalasia: a new clinically relevant classification by high-resolution manometry. Gastroenterology 135:1526-1533.
- Rohof WO1, Salvador R, Annese V, Bruley des Varannes S, Chaussade S, et al. (2013) Outcomes of treatment for achalasia depend on manometric subtype. Gastroenterology 144: 718-725.
- Ghoshal UC, Rangan M, Misra A (2012) Pneumatic dilation for achalasia cardia: reduction in lower esophageal sphincter pressure in assessing response and factors associated with recurrence during long-term follow up.Dig Endosc 24:7-15.
- Ghoshal UC1, Kumar S, Saraswat VA, Aggarwal R, Misra A, et al. (2004) Long-term follow-up after pneumatic dilation for achalasia cardia: factors associated with treatment failure and recurrence. Am J Gastroenterol 99: 2304-2310.
- Ghoshal UC, Gupta M, Verma A et al.High-resolution manometry is comparable to timed barium esophagogram for assessing response to pneumaticdilation in patients with achalasia.Indian J Gastroenterol 34:144-151.
- Nicodème F, de Ruigh A, Xiao Y, Rajeswaran S, Teitelbaum EN, et al. (2013) A comparison of symptom severity and bolus retention with Chicago classification esophageal pressure topography metrics in patients with achalasia. Clin Gastroenterol Hepatol 11: 131-137.
- Cho YK, Lipowska AM, Nicodème F (2014) Assessing bolus retention in achalasia using high-resolution manometry with impedance: a comparator study with timed barium esophagram. Am J Gastroenterol 109:829-835.
- Lin Z, Carlson DA, Dykstra K et al. High-resolution impedance manometry measurement of bolus flow time in achalasia and its correlation with dysphagia. Neurogastroenterol Motil 27:1232-1238.
- Neyaz Z, Gupta M, Ghoshal UC (2013) How to perform and interpret timed barium esophagogram. J Neurogastroenterol Motil 19: 251-256.
- Andersson M, Lundell L, Kostic S (2009) Evaluation of the response to treatment in patients with idiopathic achalasia by the timed barium esophagogram: results from a randomized clinical trial. Dis Esophagus 22:264-273.
- Vaezi MF, Baker ME, Achkar E (2002) Timed barium oesophagram: better predictor of long term success after pneumatic dilation in achalasia than symptom assessment. Gut 50:765-70.
- Vaezi MF, Baker ME, Richter JE (199) Assessment of esophageal emptying post-pneumatic dilation: use of the timed barium esophagram. Am J Gastroenterol 94:1802-1807.
- Rohof WO, Lei A, Boeckxstaens GE (2013) Esophageal stasis on a timed barium esophagogram predicts recurrent symptoms in patients with long-standing achalasia. Am J Gastroenterol 108: 49-55.
- Rieder E, Swanström LL, Perretta S (2013) Intraoperative assessment of esophagogastric junction distensibility during per oral endoscopic myotomy (POEM) for esophageal motility disorders.Surg Endosc 27:400-405.
- Verlaan T1, Rohof WO, Bredenoord AJ, Eberl S, Rösch T, et al. (2013) Effect of peroral endoscopic myotomy on esophagogastric junction physiology in patients with achalasia. Gastrointest Endosc 78: 39-44.
- Rohof WO, Hirsch DP, Kessing BF (2012) Efficacy of treatment for patients with achalasia depends on the distensibility of the esophagogastric junction.Gastroenterology 143:328-335.
- Teitelbaum EN, Sternbach JM, El Khoury R, Soper NJ, Pandolfino JE, et al. (2016) The effect of incremental distal gastric myotomy lengths on EGJ distensibility during POEM for achalasia. Surg Endosc 30: 745-750.
- Vaezi MF, Pandolfino JE, Vela MF (2013) ACG clinical guideline: diagnosis and management of achalasia. Am J Gastroenterol 108: 1238-1249.
- Vanuytsel T, Bisschops R, Farré R (2013) Botulinum toxin reduces dysphagia in patients with nonachalasia primary esophageal motility disorders. ClinGastroenterolHepatol 11:1115–1121.
- Boeckxstaens GE, Annese V, des Varannes SB, Chaussade S, Costantini M, et al. (2011) Pneumatic dilation versus laparoscopic Heller's myotomy for idiopathic achalasia. N Engl J Med 364: 1807-1816.
- Molina EG, Stollman N, Grauer L, Reiner DK, Barkin JS (1996) Conservative management of esophageal nontransmural tears after pneumatic dilation for achalasia. Am J Gastroenterol 91: 15-18.
- Vanuytsel T, Lerut T, Coosemans W(2012) Conservative management of esophageal perforations during pneumatic dilation for idiopathic esophageal achalasia. Clin Gastroenterol Hepatol 10:142–149.
- Heller E (1914) Extramukose Kardiaplastik beim chronischen kardiospasmus mit dilatation des oesophagus. Mitt Grenzgeb Med Chir 27:141–149.
- Gaissert HA, Lin N, Wain JC, Fankhauser G, Wright CD, et al. (2006) Transthoracic Heller myotomy for esophageal achalasia: analysis of long-term results. Ann Thorac Surg 81: 2044-2049.
- Rawlings A, Soper NJ, Oelschlager B (2012) Laparoscopic Dor versus Toupet fundoplication following Heller myotomy for achalasia: results of a multi-center, prospective, randomized-controlled trial. Surg Endosc 26:18–26.
- Kilic A, Schuchert MJ, Pennathur A, Gilbert S, Landreneau RJ, et al. (2009) Long-term outcomes of laparoscopic Heller myotomy for achalasia. Surgery 146: 826-831.
- Moonen A, Annese V, Belmans A (2015) Long-term results of the European achalasia trial: a multicentre randomised controlled trial comparing pneumatic dilation versus laparoscopic Heller myotomy. Gut.
- Ortega JA, Madureri V, Perez L (1980) Endoscopic myotomy in the treatment of achalasia. Gastrointest Endosc 26: 8-10.
- Sumiyama K, Tajiri H, Gostout CJ (2008) Submucosal endoscopy with mucosal flap safety valve (SEMF) technique: a safe access method into the peritoneal cavity and mediastinum.Minim Invasive Ther Allied Technol 17: 365-369
- Pasricha PJ, Hawari R, Ahmed I, Chen J, Cotton PB, et al. (2007) Submucosal endoscopic esophageal myotomy: a novel experimental approach for the treatment of achalasia. Endoscopy 39: 761-764.
- Inoue H, Minami H, Satodate H, Kudo SE (2009) First Clinical Experience of Submucosal Endoscopic esophagealmyotomy for esophageal achalasia with no skin incision. GastrointestEndosc 69: AB122.
- Ramchandani M, Nageshwar Reddy D1 (2014) Peroral endoscopic myotomy: technique of mucosal incision. Clin Gastroenterol Hepatol 12: 900-901.
- Friedel D, Modayil R, Stavropoulos SN1 (2014) Per-oral endoscopic myotomy: major advance in achalasia treatment and in endoscopic surgery. World J Gastroenterol 20: 17746-17755.
- Li QL, Chen WF, Zhou PH, Yao LQ, Xu MD, et al. (2013) Peroral endoscopic myotomy for the treatment of achalasia: a clinical comparative study of endoscopic full-thickness and circular muscle myotomy. J Am Coll Surg 217: 442-451.
- Duan T, Zhou J, Tan Y (2015) PerOral Endoscopic Myotomy for Severe Achalasia: the Comparison of Full-Thickness Myotomy and Circular Myotomy.GastrointestEndosc 81: AB118.
- Tang X, Deng Z, Gong W (2015) PerOral Endoscopic Short Versus Long Myotomy for the Treatment of Achalasia: a Case-Control Study. GastrointestEndosc 81: AB117 .
- Ramchandani M, Reddy DN, Darisetty S (2015) Peroral endoscopic myotomy for achalasia cardia: Treatment analysis and follow up of over 200 consecutive patients at a single center.Dig Endosc.
- Ren Z, Zhong Y, Zhou P (2012) Perioperative management and treatment for complications during and after peroral endoscopicmyotomy (POEM) for esophagealachalasia (EA) (data from 119 cases). Surg Endosc 26: 3267-3272.
- Inoue H, Sato H, Ikeda H, Onimaru M, Sato C2, et al. (2015) Per-Oral Endoscopic Myotomy: A Series of 500 Patients. J Am Coll Surg 221: 256-264.
- Zhou P, Yao L, Zhang YQ (2012) Peroral endoscopic myotomy (POEM) for esophageal achalasia: 205 cases report. GastrointestEndosc 75: AB132-AB133.
- Werner YB, Costamagna G, Swanström LL3 von Renteln D, Familiari P, et al. (2015) Clinical response to peroral endoscopic myotomy in patients with idiopathic achalasia at a minimum follow-up of 2 years. Gut .
- Sharata AM, Dunst CM, Pescarus R (2015) Peroral endoscopic myotomy (POEM) for esophageal primary motility disorders: analysis of 100 consecutive patients.J Gastrointest Surg 19: 161-170.
- Stavropoulos SN, Modayil RJ, Friedel D, Savides T (2013) The International Per Oral Endoscopic Myotomy Survey (IPOEMS): a snapshot of the global POEM experience. Surg Endosc 27: 3322-3338.
- Von Renteln D, Fuchs KH, Fockens P () Peroral endoscopic myotomy for the treatment of achalasia: an international prospective multicenter study. Gastroenterology 145:309-311.
- Hungness ES, Teitelbaum EN, Santos BF, Arafat FO, Pandolfino JE, et al. (2013) Comparison of perioperative outcomes between peroral esophageal myotomy (POEM) and laparoscopic Heller myotomy. J Gastrointest Surg 17: 228-235.
- Teitelbaum EN, Rajeswaran S, Zhang R (2013) Per oral esophageal myotomy (POEM) and laparoscopic Heller myotomy produce a similar short-term anatomic and functional effect.Surgery 154:885-891.
- Ujiki MB, Yetasook AK, Zapf M, Linn JG, Carbray JM, et al. (2013) Peroral endoscopic myotomy: A short-term comparison with the standard laparoscopic approach. Surgery 154: 893-897.
- Chan SM, Wu JC, Teoh AY (2015) Comparison of early outcomes and quality of life after laparoscopic Heller's cardiomyotomy to peroral endoscopic myotomy for treatment of achalasia.Dig Endosc.
- Kumbhari V, Tieu AH, Onimaru M, El Zein MH, Teitelbaum EN, et al. (2015) Peroral endoscopic myotomy (POEM) vs laparoscopic Heller myotomy (LHM) for the treatment of Type III achalasia in 75 patients: a multicenter comparative study. Endosc Int Open 3: E195-201.
- Zhou PH, Li QL, Yao LQ, Xu MD, Chen WF, et al. (2013) Peroral endoscopic remyotomy for failed Heller myotomy: a prospective single-center study. Endoscopy 45: 161-166.
- Onimaru M, Inoue H, Ikeda H (2015) Peroral endoscopic myotomy is a viable option for failed surgical esophagocardiomyotomy instead of redo surgical Heller myotomy: a single center prospective study.J Am Coll Surg 217:598-605.
- Vigneswaran Y, Yetasook AK, Zhao JC, Denham W, Linn JG, et al. (2014) Peroral endoscopic myotomy (POEM): feasible as reoperation following Heller myotomy. J Gastrointest Surg 18: 1071-1076.
- Ling T, Guo H, Zou X (2014) Effect of peroral endoscopic myotomy in achalasia patients with failure of prior pneumatic dilation: a prospectivecase-control study. J GastroenterolHepatol 29:1609-1613.
- Li QL, Yao LQ, Xu XY (2015) Repeat peroral endoscopic myotomy: a salvage option for persistent/recurrent symptoms.Endoscopy.
- Hu JW, Li QL, Zhou PH (2015) Peroral endoscopic myotomy for advanced achalasia with sigmoid-shaped esophagus: long-term outcomes from a prospective, single-center study.SurgEndosc 29:2841-2850.
- Chen WF, Li QL, Zhou PH (2015) Long-term outcomes of peroral endoscopic myotomy for achalasia in pediatric patients: a prospective, single-center study. Gastrointest Endosc 81:91-100.
- Tang X, Gong W, Deng Z, Zhou J, Ren Y, et al. (2015) Usefulness of peroral endoscopic myotomy for treating achalasia in children: experience from a single center. Pediatr Surg Int 31: 633-638.
- Zeng Y, Dai YM, Wan XJ (2014) Clinical remission following endoscopic placement of retrievable, fully covered metal stents in patients withesophageal achalasia. Dis Esophagus 27:103-108.
- Cai XB, Dai YM, Wan XJ, Zeng Y, Liu F, et al. (2013) Comparison between botulinum injection and removable covered self-expanding metal stents for the treatment of achalasia. Dig Dis Sci 58: 1960-1966.
- Zhu YQ, Cheng YS, Tang GY (2010) Comparison of temporary stent insertion with pneumatic dilation of the same diameter in the treatment ofachalasia patients: a retrospective study. J Gastroenterol Hepatol 25:499-505.
- Ghoshal UC, Rangan M (2011) A review of factors predicting outcome of pneumatic dilation in patients with achalasia cardia. J Neurogastroenterol Motil 17: 9-13.
- Khashab MA, Messallam AA, Onimaru M (2015) International multi-center experience with peroral endoscopic myotomy for the treatment of spastic esophageal disorders refractory to medical therapy (with video) Gastrointest Endosc81:1170–1177.
- Campos GM, Vittinghoff E, Rabl C (2009) Endoscopic and surgical treatments for achalasia: a systematic review and meta-analysis. Ann Surg 249:45–57.
- Youn YH1, Minami H2, Chiu PW3, Park H1 (2016) Peroral Endoscopic Myotomy for Treating Achalasia and Esophageal Motility Disorders. J Neurogastroenterol Motil 22: 14-24.
- Leeuwenburgh I, Scholten P, Alderliesten J, Tilanus HW, Looman CW, et al. (2010) Long-term esophageal cancer risk in patients with primary achalasia: a prospective study. Am J Gastroenterol 105: 2144-2149.
- Vela MF, Richter JE, Khandwala F, Blackstone EH, Wachsberger D, et al. (2006) The long-term efficacy of pneumatic dilatation and Heller myotomy for the treatment of achalasia. Clin Gastroenterol Hepatol 4: 580-587.
Relevant Topics
- Constipation
- Digestive Enzymes
- Endoscopy
- Epigastric Pain
- Gall Bladder
- Gastric Cancer
- Gastrointestinal Bleeding
- Gastrointestinal Hormones
- Gastrointestinal Infections
- Gastrointestinal Inflammation
- Gastrointestinal Pathology
- Gastrointestinal Pharmacology
- Gastrointestinal Radiology
- Gastrointestinal Surgery
- Gastrointestinal Tuberculosis
- GIST Sarcoma
- Intestinal Blockage
- Pancreas
- Salivary Glands
- Stomach Bloating
- Stomach Cramps
- Stomach Disorders
- Stomach Ulcer
Recommended Journals
Article Tools
Article Usage
- Total views: 29133
- [From(publication date):
February-2016 - Jul 17, 2024] - Breakdown by view type
- HTML page views : 27773
- PDF downloads : 1360