Research Article Open Access
Acceptance and Positive Attitude Increased Utilization of Long Acting and Permanent Family Planning Methods Among Reproductive Age Group Women from Debre Berhan District, Ethiopia: Quantitative and Qualitative Analysis
Asegidew W1*,Tariku B1, Kaba M2, Getachew S2 and Ketsela K31Department of Public Health, Health Sciences College, Debre Berhan University, Ethiopia
2Department of Public Health, College of Medicine and Health Sciences, Addis Ababa University, Ethiopia
3Department of Nursing, Health Sciences College, Debre Berhan University, Ethiopia
- Corresponding Author:
- Wondesen Asegidew
Department of Public Health
Health Sciences College
Debre Berhan University, Ethiopia
Tel: 251911071777
E-mail: wondeasgw@gmail.com
Received Date: July 10, 2017; Accepted Date: July 27, 2017; Published Date: July 31, 2017
Citation: Asegidew W,Tariku B, Kaba M, Getachew S, Ketsela K (2017) Acceptance and Positive Attitude Increased Utilization of Long Acting and Permanent Family Planning Methods Among Reproductive Age Group Women from Debre Berhan District, Ethiopia: Quantitative and Qualitative Analysis. J Community Med Health Educ 7:541. doi:10.4172/2161-0711.1000541
Copyright: © 2017 Asegidew W, et al. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution and reproduction in any medium, provided the original author and source are credited.
Visit for more related articles at Journal of Community Medicine & Health Education
Abstract
Background: Wider access and use of long-acting and permanent methods of contraception are the most effective contraceptives available to contribute to reduction of the high levels of maternal mortality and morbidity. Yet, utilization of long acting and permanent contraception methods in Ethiopian is recorded to be low.
Objective: The purpose of this study was to describe utilization of long acting reversible and permanent family planning methods and identify associated factors among women of 15-49 years age group in Debre Berhan district, Ethiopia.
Methods: A community based cross-sectional study was conducted in four selected kebeles of Debre Berhan. Cluster sampling was used to select study subjects for survey while purposive sampling was used to select study subjects for qualitative study. A pre-tested structured questionnaire was used to collect quantitative data and interviewer topic guide was used for qualitative. The survey data was entered into Epi-Info version 3.5.4 and exported, cleaned and analyzed using SPSS version 21. Open code version 3.6.2 was used to categorize and code qualitative data. Factors associated with utilization of long acting and permanent contraceptive methods were identified using logistic regression model and content analysis of qualitative data.
Results: Current utilization of long acting and permanent family planning methods among women of reproductive age was estimated to be 27.3% (95% CI: 23.4-31.2). Women of 24-35 age group were 2.23 (AOR=2.23; 95% CI: 1.18-4.18) times more likely to utilize long acting and permanent contraceptive methods as compared to those women whose age was 35 and above. Women who had positive attitude towards the method were 1.87 times more likely to use long acting and permanent contraceptive methods as compared to those women who had negative attitude (AOR=1.87; 95% CI: 1.13-3.07). Clients who were satisfied with treatment and advice given were 1.81 times more likely to use long acting and permanent contraceptive methods as compared to those clients who were not satisfied (AOR=1.81; 95% CI: 1.1-2.99). Myths and misconceptions about intrauterine device and implants were major barriers for the use of long acting and permanent contraceptive methods.
Conclusion: Acceptance, positive attitude, client satisfaction and age were factors affecting utilization, whereas myth and misconception in the community hindered use of long acting and permanent contraceptive methods. Therefore, sustained and appropriate information on long acting and permanent contraceptive methods should be provided to raise awareness and build the attitude of women and the community. District health office should design educational programs that promote long acting family planning and reduce barriers at community level in the town. Moreover, health professionals should improve the quality of long acting and permanent contraceptive methods service, which enhances satisfaction.
Keywords
Contraceptive methods; Debre Berhan; LAPM; Utilization
Introduction
As of June 2013 UN reported, world population to hit 7.2 billion. The report further projected world population increase by almost one billion people during the next twelve years. With that the world population is projected to reach 8.1 billion in 2025 and 9.6 billion in 2050 [1]. Over the past four decades, the organized international family planning effort has made great progress in expanding the availability and use of reproductive health and family planning services [2]. Family planning has widespread positive impacts for population health and well-being; contraceptive use not only decreases unintended pregnancies, reduces infant, maternal mortality and morbidity, but it is critical to the achievement of Sustained- Development Goals [3].
In 2012, an estimated 645 million women in the developing world were using modern methods- 42 million more than in 2008. About half of this increase was due to population growth in developing world. The proportion of married women using modern contraceptives barely changed from 56% in 2008 to 57% in 2012. Serving all women in developing countries that currently have an unmet need for modern methods would prevent an additional 54 million unintended pregnancies, including 21 million unplanned births, 26 million abortions (of which 16 million would be unsafe) and 7 million miscarriages; this would also prevent 79,000 maternal deaths and 1.1 million infant deaths. Special attention is needed to ensure that the contraceptive needs of vulnerable groups such as unmarried young women, poor women and rural women are met and that inequities in knowledge and access are reduced [4]. Research done in America and Europe showed that the most common contraceptive methods currently used by respondents in all countries were the contraceptive pill and male condom [5]. Recent scientific findings and new understanding about long-acting and permanent methods of contraception underscore their safety and effectiveness [6,7]. The methods considered “long-acting” in this context are intrauterine devices (IUDs) and implants; vasectomy and female sterilization are considered “permanent.” Wider access and use of family planning, especially of long-acting and permanent methods of contraception which are the most effective contraceptives available, can substantially reduce the high levels of maternal mortality and morbidity in developing countries, as well as unwanted pregnancies and abortion [2].
In Ethiopia, fertility declined from 5.4, to 4.8 children per woman between 2005-2011 which had decreased by about one child and the decrement also very slow and time taking. Among currently married women, 29% used any method of contraceptive. The most common modern method used was injectable, which was 21% of currently married women, and 32% of unmarried sexually active women. But only 3% of them had used long acting and permanent methods, IUD, female sterilization and implant were used by 0.2%, 1.3% and 2.4% of women, respectively [8]. Another finding in Ethiopia reported that the most common family planning method used was injections (83.1%) followed by oral contraceptives (17.7%) but none of them used longterm methods [9-11]. Thus, this study examined the association of factors affecting utilization of long acting reversible contraception and permanent method among women of reproductive age, adjusting for several factors known to be associated with contraceptive use. Besides, it was designed to test hypotheses; Do positive attitude and acceptance of LAPMs increases the uptake of LAPMs?
Methodology
Community-based cross-sectional study supported with qualitative data was conducted among reproductive age group women in Debre Berhan town, Ethiopia from February to June 2014. Debre Berhan town is found in Amhara Region State, North Shoa administrative Zone. It is located 130 kms Northeast of Addis Ababa, Ethiopia. Based on the last census of 2007, the population of the town was estimated to be 97,908. The town is divided into 9 urban kebeles and 5 rural kebeles. There are one governmental referral hospital, one private general hospital, one higher clinic, two medium clinics, three health centers, four lower clinics and two drug venders in the town [8]. Among source populations, study subjects were included by inclusion criteria.
Sample size for quantitative data
The sample size was calculated using the following assumptions; proportion (p) of utilization of long acting and permanent contraceptive methods of Ethiopia is 12.3% [12]. Confidence level of 95%, which means α (alpha) at 0.05 and Zα/2=1.96 and acceptable difference of 3% (0.03). Finally, the calculated sample size was 461. Adding 10% for non-response rate, we recruited 507 reproductive age group women.
Two stage cluster sampling procedures were employed to identify study subjects. In the first stage four kebeles were randomly selected among nine kebeles (clusters) of the town. Secondly, all study subjects were identified until the required sample size was reached.
Data collection tools and Procedure
A structured face to face questionnaire with both open and closed ended questions were used to collect the data. The questionnaire encompasses socio-economic and demographic, past contraception history, knowledge on LAPMs, attitude toward LAPMs, counseling status and information specific to the use of LAPMs. The questionnaire was adapted from reviewing different literatures and scientific facts. Questionnaire was first prepared in English and translated to Amharic (local language) by principal investigator and reviewed by peer public health professional to make it understandable by the study subjects and to check whether the translation was consistent with the English version or not. The questionnaire was back translated to English by another person. Before the actual data collection, the questionnaire was pre-tested in 5% (26 women) at similar setting near in the study setting one week before the scheduled data collection day. Based on the pretest, necessary modification was made. Four public health officer students, as data collectors and two health officers as supervisors were recruited and trained on objectives of the study, data collection tools and interview techniques for two days by the principal investigator.
Qualitative data
Five in-depth interviews were done with the women to explore myth, misconception, perception and the reasons of why they use or not use LAPMs. The study participants were selected through purposive sampling method. The probes for the in-depth interviews were developed with the help of available literature. One person was assigned for field note taking and tape recording while the principal investigator facilitated the interview. Interviewer guide was used for facilitate the in-depth interview. This process ended when information saturation was reached.
Operational definitions
LAPMs: Three contraceptive methods are categorized as long acting or permanent these are intrauterine devices (IUDs), implants and female sterilization.
Very good knowledge: Women who scored 80% and above distinct features of LAPMs knowledge assessing questions.
Good knowledge: Women who scored 60 up to 79% distinct features of LAPMs from knowledge assess questions.
Poor knowledge: Women who scored less than 60% features of any of the LAPMs from knowledge assessing questions
Positive attitude: Women who scored above mean to the correct answers from attitude measuring LAPMs questions.
Negative attitude: Women who scored less than or equal to mean score from attitude measuring LAPMs questions
Data processing and analysis
Quantitative data were entered into Epi-Info version 3.5.4, then cleaned, coded and exported to statistical package for service solution (SPSS V.20) for analysis. Descriptive statistics, such as proportion, mean, standard deviation, frequency distribution tables and graphs were used to describe study findings. To determine the potential influence of explanatory variables on utilization of LAPMs, binary logistic regression was used to calculate crude and adjusted odds ratio with adjustments for covariates. Those factor variables with p-value ≤ 0.25 in bivariable logistic regression were entered into multivariable logistic regression analysis. Statistical significance was declared if the p-value is less than 0.05. Besides, data from the in-depth interview were translated and transcribed to English and categorized and coded accordingly to main thematic areas using Open code software version 3.6.2.
Ethical consideration
Data collection was carried out after getting approval of project from IRB (Ethical Review Board of the medical faculty of Addis Ababa University. Official permission and letter were obtained from North Shoa Zonal Health Department. Verbal consent was gained from individual participants. All the participants of this study were told about their participation could be on a voluntary basis and their information was kept confidential.
Results
Out of 507 households from 4 clusters, 499 participated with a response rate of 98.42%.
Socio-demographic characteristics of respondents
The mean age of the respondents was 31.69 ± 8 years. Regarding family size, 312 of the respondent have family size of four and above and the majority of the respondents 464 (93%) were Orthodox Christian and 462 (92.6%) were Amhara in ethnicity. One hundred sixty nine (33.9%) of them attended secondary education while 77 (15.4%) of them had no formal education. In addition 150(36.9%) of the respondents’ husband attended college and above but only 32(7.9%) of them had no formal education. Two hundred thirty eight (47.7%) of respondents were house wife and 186 (45.7%) of the respondent’s husband were government employees. Four hundred seven (81.6%) of respondent were currently married and 253 (50.7%) of the respondents had monthly income above the median. From the qualitative finding participants’ characteristic shows that all key informant women were orthodox by religion, Amhara by ethnicity and married (Table 1).
| Variable | Frequency | Percentage |
|---|---|---|
| Age Mean + SD 15-24 25-34 35+ |
31.69 + 8 108 188 203 |
21.6 37.7 40.7 |
| Family size | ||
| 1-3 >4 |
187 312 |
37.5 62.5 |
| Religion | ||
| Orthodox Others |
464 35 |
93 7 |
| Ethnicity | ||
| Amhara Others |
462 27 |
92.6 7.4 |
| Educational status | ||
| No education Primary Secondary College and above |
77 137 169 116 |
15.4 27.5 33.9 23.2 |
| Husband education husband | ||
| No education Primary Secondary College and above |
32 90 135 150 |
7.9 22.1 32.2 36.9 |
| Occupation of respondent | ||
| Gov. employee Merchant House wife student Daily laborer Others |
110 44 238 35 45 27 |
22 8.8 47.7 7 9 5.4 |
| Main occupation of husband | ||
| Gov. employee Merchant Daily laborer Others |
197 55 101 54 |
48.4 13.5 24.9 13.3 |
| Marital status | ||
| Married Single Divorced Widowed |
407 42 30 20 |
81.6 8.4 6 4 |
| Monthly income | ||
| < 1200 ≤ 1200 |
246 253 |
49.3 50.7 |
Table 1: Socio demographic characteristics of the respondents, Debre Berhan Town, Amhara, Ethiopia May, 2014.
Obstetric characteristics of the respondents
Majority of the respondents 374(74.9%) had married below the age of twenty five with the mean age of 20 ± 3.65 years. At their first birth more than half of the respondents were twenty four or below years old with the mean age of 22.55 ± 3.98 years. One hundred seventy (34.1%) of the respondents had three and more pregnancy. Thirty six (7.2%) of them encountered abortions which were more than half 20(55.6%) of the abortion took place in health institution and 31(86.1%) of them had unsafe abortion. Three hundred ninety nine (80%) of the respondents had at least one live child and 104(20.8%) of the respondents had only one pregnancy. Two hundred forty nine (49.9%) of the respondents planned to have child in the future (Table 2).
| Variable | Frequency | Percentage (%) |
|---|---|---|
| Age at time of first marriage(n=457) | ||
| Mean+SD 15-24 25-34 Not married yet |
20+3.65 374 82 43 |
74.9 16.5 8.6 |
| Age at time of First birth(n=404) | ||
| Mean+SD 15-24 25-34 Not gave birth yet |
22.55+3.98 282 118 99 |
56.6 23.6 19.8 |
| Number pregnancies | ||
| One Two Three and above None |
104 135 170 90 |
20.8 27.1 34.1 18 |
| Having live children | ||
| Yes No |
399 100 |
80 20 |
| Want more children for future | ||
| Yes No |
249 250 |
49.9 50.1 |
| Passed away child | ||
| Yes No |
39 460 |
7.8 92.2 |
Table 2: Obstetric characteristic of respondents, Debre Berhan Town, Amhara, Ethiopia, May 2014.
Utilization of long acting and permanent contraceptive methods
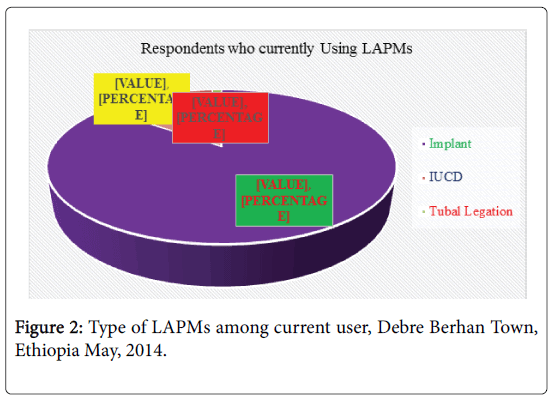
One hundred seventy five (35.1%) of the women were ever used LAPMs. Most of them used implant 149(85.1%) and the rest of them 25(13.7%) used IUD and 2(1.2%) used female sterilization method (Figure 1). One hundred thirty six (27.3%, 95% CI; 23.4-31.2) of the respondents were currently using LAPMs, of which most of them were using implant (86.0%) (Figure 2). Reasons for discontinuing use of LAPMs from ever used women were shifting to other methods and want to have a child. Regarding place for family planning service, more than half of the users 71(52.2%) had got the service from health center followed by hospital 38(27.9%) and 120(88.2%) had got the service free of charge.
Knowledge of respondents on LAPMs
Four hundred fifty nine (92%) of the respondents were able to mention at least one method of modern family planning method. Injection was the most known method and vasectomy was the least known method among modern family planning techniques which accounts 437(92.5%) and 170(37%), respectively. Four hundred forty (88.2%) of the respondents know at least one method of long acting and permanent family planning methods among them the most known was implant 430(97.7%) and the least known was vasectomy 173(39.3%). As shown in chart 3, the reasons behind use of long acting and permanent family planning methods were for limiting family size 397(90.2%), followed by child spacing 383(87%) (Figure 3).
Three hundred eighty five (87.5%) of the women were aware of that IUD can prevent pregnancy for 10 years and 273(62%) of them said IUD is not good for female at risk of getting sexual transmitted infection. In this study 145(23%), 112(25.5%) and 116(26.4%) of the women said that IUD had effect on sexual intercourse and desire, IUD does not results in immediate pregnancy after removal and IUD can causes cancer respectively. This finding was supported by qualitative data; “IUD causes uterine cancer; it is bad if stayed in uterus for long period of time, and affects sexual intercourse and desire,” a 25 years old married respondent.
Moreover, 405(92%) of women had an awareness that implant can prevent pregnancy for 3-5 years and 339(77%) of the respondents knew that implants required minor surgery during insertion and removal, while 343(78%) of them believed that implants was immediately reversible. Generally, 153(30.7%) of the respondents had very good knowledge, 221(44.3%) of the respondents had good knowledge, and the remaining 125 (25.1%) of them had poor knowledge towards LAPMs
Attitude of the respondents towards utilization of LAPMs
Three hundred ninety nine (80%) of the women accepted utilization of LAPMs. Majority 318 (78.1%) of the respondents were supported by their husbands, while the rest 89 (21.9%) of their husband was against utilization. The most common reason for non-acceptors was fear of side effect and religious opposition. Two hundred twenty six (45.3%) of the respondents agreed on the insertion and removal of implant was not highly painful while 184(36.9%) and 140(28.1%) of the respondents agreed that Insertion of IUD affected their privacy. In addition to these, they believe that IUD and implants could prevent them doing heavy work. This finding was supported by qualitative data;
“Our people are daily laborer, work overloaded, so that it is protecting us from moving and working freely”.
“Different women in the community talk something frustrating about utilizations of IUD. Some of them say IUD may cause uterine cancer; it is bad if stayed in our uterus for long period of time, it may affect sexual intercourse and desire. Besides, those women who used this method may not give birth in the future”.
Based on utilization the third participants shared her ideas as follows:
“IUD may further enter into surrounding tissue and causes damage the uterus of mother which may lead to infertility”
Pertaining to the attitude of the responders, more than half 262(52.5%) of the women had negative attitude towards practicing LAPMs and 262(47.2%) of them had positive attitude towards LAPMs.
Level of service satisfaction of the women
According to our study, 91(66.9%) and 34(25%) of the respondents have got family planning service without waiting time and with reasonable waiting time, respectively. Out of current users of LAPM, 46(33.8%) of the women had developed side effects with the method they are using, the rest 90(66.2%) do not have such side effects. Eighty (58.8%) of the users were given advice on what to do if there is side effect. Generally, 92(67.6%) of current users of LAPMs were satisfied with the advice or treatment that was given to them to manage side effects. This is supported by qualitative findings.
“If there is a problem after starting utilization of contraceptive method, service providers will give us a treatment based on the type of side effect occurred and even they give an appointment for further investigation and solutions.” Said married 30 years old women, Orthodox in religion.
Out of five, four of the participants explained their perception:
“Health workers provide us necessary information about the benefit and side effect of each contraceptive method. If there is a problem after starting utilization of a contraceptive method, they give us a treatment based on the type of problem and even give an appointment for further investigation and solution. Such treatment increased our service satisfaction and thereby increasing service utilization” Said married 26 years old women, Orthodox in religion.
Multivariable analysis of logistic regression
Logistic regression analysis revealed that women in 25-34 age groups, women’s acceptance of utilization of LAPMs, attitude of women toward utilization of LAPMs and satisfaction of the women by the treatment and advice were independent predictors of utilization of LAPMs.
Women of 24-35 age group were 2.23(AOR=2.23; 95% CI: 1.18-4.18) times more likely to utilize LAPMs as compared to those women whose age was 35 and above. Women who have positive attitude towards LAPMs were 1.87 times more likely to use LAPMs as compared to those women who had negative attitude towards LAPMs (AOR=1.87; 95% CI: 1.13-3.07). Clients who are satisfied with treatment and advice given were 1.81 times more likely to use LAPMs as compared to those clients who were not satisfied with treatment and advice given (AOR=1.81; 95% CI: 1.1-2.99). Myth and misconception in the community were other barriers for utilization of LAPMs (Table 3).
| Variables | Utilization of LAPMs | COR (95% CI) | AOR (95% CI) | P value | |
|---|---|---|---|---|---|
| Yes | No | ||||
| Age | |||||
| 15-24 | 26 | 82 | 1.08(.62-1.87) | 2.33(0.89-6.05) | 0.08 |
| 25-34 | 64 | 124 | 1.76(1.23-2.75)* | 2.23(1.18-4.18)** | 0.014 |
| ≥ 35 | 46 | 157 | 1 | 1 | |
| Family size | |||||
| ≥ 4 | 95 | 217 | 1.56(1.02-2.38)* | 1.24(0.49-1.76) | 0.82 |
| 01-Mar | 41 | 146 | 1 | 1 | |
| Monthly income | |||||
| >1200 | 78 | 168 | 1.56(1.05-2.32)* | 0.95(0.69-2.23) | 0.47 |
| ≤ 1200 | 58 | 195 | 1 | 1 | |
| Age at time of first marriage | |||||
| 15-24 | 110 | 264 | 5.57(1.68-18.33)* | 2.68(0.59-12.13) | 0.2 |
| 25-34 | 23 | 59 | 5.20(1.47-18.48)* | 3.84(0.68-12.57 | 0.13 |
| Yet not married | 3 | 40 | 1 | 1 | |
| Age at time of First birth | |||||
| 15-34 | 85 | 197 | 2.62(1.41-4.87)* | 0.99(0.18-5.34) | 0.99 |
| 25-35 | 37 | 81 | 2.77(1.40-5.51)* | 0.83(0.15-4.69) | 0.83 |
| Not gave birth yet | 14 | 85 | 1 | 1 | |
| Number pregnancies | |||||
| One | 25 | 79 | 1.87(0.89-3.93) | 0.41(0.03-4.94) | 0.48 |
| Two | 48 | 87 | 3.27(1.65-6.48)* | 0.55(0.04-7.78) | 0.66 |
| Three and above | 50 | 120 | 2.47(1.26-4.84)* | 0.78(0.04-14.56) | 0.86 |
| None | 23 | 77 | 1 | 1 | |
| Live children | |||||
| 01-Feb | 76 | 172 | 2.71(1.45-5.08)* | 2.74(0.22-34.62) | 0.44 |
| 3 and above | 46 | 105 | 2.69(1.39-5.22)* | 2.41(0.14-41.43) | 0.55 |
| Have no child | 14 | 86 | 1 | 1 | |
| Knowledge of respondents | |||||
| Highly knowledge | 48 | 105 | 2.40(1.33-4.32)* | 1.21(0.60-2.46) | 0.57 |
| Moderate knowledge | 68 | 153 | 2.33(1.34-4.02)* | 1.30(0.67-2.52) | 0.43 |
| Low knowledge | 20 | 105 | 1 | 1 | |
| Accept utilization of LAPMs | |||||
| Yes | 131 | 271 | 8.89(3.53-22.41) | 4.21(1.53-11.55)** | 0.005 |
| No | 5 | 92 | 1 | 1 | |
| Attitude of respondents | |||||
| Positive attitude | 85 | 152 | 2.13(1.54-3.47)* | 1.81(1.12-2..94)** | 0.016 |
| Negative attitude | 51 | 211 | 1 | 1 | |
| Satisfied with the advice & treatment given | |||||
| Yes | 92 | 107 | 1.56(1.05-2.32)* | 1.86(1.14-3.04)** | 0.013 |
| No | 44 | 92 | 1 | 1 | |
Table 3: Determinants for current use of LAPMs among women from Debre Berhan Town, Ethiopia, May 2014.
Discussion
The overall current prevalence of long acting and permanent family planning methods was 27.3%. This result was high compared to research done in Bale and Mekelle which were 8.72% and 12.3%, respectively. This difference could be as a result of study setting, time of the study, the deployments of urban health extension worker which may supported to bring positive attitude towards LAPMs at community level, currently different Medias were promoting utilization of LAPMs and the government attention towards these methods increased utilization rate. Moreover, this result was consistent with research done in Iran which was 27.7% [12,13]. The majority of the women used implant 117(86.03%) followed by IUD 16(11.76) and only 3(2.21%) of the women were using female sterilization. This finding was consistent with EDHS 2011 findings which were utilization of LAPMs in urban areas found to be 0.9% for IUD 3.8% for implants and 0.5% female sterilization [8]. In contrary, it is inconsistent with research done in Guatemala, majority of women were used female sterilization and IUD than implant which was female sterilization, IUD and implants 16%, 8% and 6%, respectively [7]. The possible reasons could be study setting, study design and study time.
The main reasons for using LAPMs in the present study were child spacing 61.0% and limiting the number of children 39.0%. These results were similar with research done in Bale and Mekelle which showed that child spacing was 54% and limiting child was 40.6% in Bale. In addition, in Mekelle town it was reported that child spacing (65%) and limiting the number of children (17%) [12,13]. Current utilization of LAPMs found to be higher for implant 117(86.03%). This is in line with study done in Mekelle and Debre Markos; majority of women were used implants among current user of LAPMs which 87% and 81.2% [12,14]. The major source of LAPMs for the women was a public health facility (80.1%). This finding is consistent with EDHS report of 2011(80%), Butajira (80.8%) and Mekelle 83% and majority of women had got services from public health facility [8,12,15]. IUD were the most extensively used LAPMs around the world but in this study it was the reverse and very low. Even if, IUD can provide effective protection for up to 10 years and might be used as alternative to sterilization for women who may regret after tubal ligation, it was low with this study [16-18]. The reasons for not to use IUD in the town were fear of side effect, loss of privacy during insertion and thought that IUD reduces daily activities which was supported from qualitative finding. It was expressed that some of the key informants were not using IUD due to the fear of difficulties mothers might face during heavy daily activities, interfere sexual intercourse and desired and it may causes uterine cancer and infertility. These were also in line with qualitative studies done India and Nigeria [19,20].
This study indicated that the main reasons for not using LAMPs were due to use of other methods which was 56.47%; most of them used injection and pills, 21.21% of them were fear of side effect, 17.35% of them criticized by their husband and 8.26% of them faced religious opposition. This findings was consistent with research done in Mojo and Mekelle in Ethiopia [14,21].
Four hundred fifty nine (92%) of women in Debre Berhan town mentioned at least one modern method of contraception. Regarding injectable 95.2%, followed by implants and IUD which were 91.5% and 88.7%, respectively. This result was consistent with finding from 2011 EDHS and research done in Butajira and Debre Markos which were 97% and 99%, respectively [8,14,16]. This study also showed that 88.2% of women had had awareness about LAPMs and 97.7%, 94.3% and 46.6% had awareness about implants, IUD, and female sterilization, respectively. This was higher compared to research done in Mekelle (63.9%) of women had heard about LAPMs and EDHS 2011 findings [8]. This might be due the recently employed urban health extension worker performance improved the awareness, the attention of government to LAPMs and also the promotion of different Medias about LAPMs that might have increased the awareness of LAPMs.
Multivariable logistic regression analyses showed that women of 25-34 age group were 2.16 times more likely to practice LAPM as compared to those women who were in age group of 35 and above (AOR=2.16, 95% CI: 1.16-4.03). This is consistent with study done in rural Ethiopia, which stated majority of implanon users were in age group of 25-34 [22-24]. Nevertheless, this was inconsistent with studies done in Mekelle, Adgirat and Debre Markos, where most users were in age group of 35 years and above [12,14,23]. This difference could be due to difference in study setting, categorization of age and time gap of the study. Those women who accept the utilization of LAPMs were 4.21 times more likely to practice long acting and permanent family planning methods as compared with those women who didn’t accept utilization (AOR=4.21, 95% CI: 1.53-11.55). This was in line with research done in Ethiopia and Pakistan. The women who were willing to use long-term family planning methods were 2.5 times more likely to use the methods than not willing to use [9]. A woman’s perception that her relatives support family planning use is important for the formation of her intention to use a contraceptive method [14]. Those women who had positive attitude towards long acting and permanent family planning methods were 1.81 times more likely to utilize LAPMs as compared with those women who had negative attitude towards long acting and permanent family planning methods (AOR=1.81, 95% CI: 1.12-2.94). This was consistent with researches done in Pakistan and Democratic Republic of Congo. Majority were self-motivated and played an important role in decision making to use contraceptive methods and most women who had a good perception about family planning had good desire to use family planning [25,26].
Moreover, satisfaction is a part and parcel of quality, the association between quality of family planning service and uptake and continuation of contraception has been demonstrated in numerous settings like study conducted in Philippines [27]. Likewise, in our study, women who were satisfied with the advice or treatment that was given to them to manage side effects were 1.71 times more likely to utilize LAPM as compared to those women who were dissatisfied (AOR=1.71, 95% CI:1.06-2.78). Similarly, studies in Butajira and Pakistan showed that service provider incompetence were one of the factors as barriers to use family planning methods utilization [28,29].
Concerning myth and misconception, as stated in qualitative data, study subjects believe that IUD and implants prevent users from doing heavy work and cause infertility. Furthermore, they stated IUD could cause uterine cancer; these situations were hindering the utilization of long acting and permanent family planning methods. This is in line with qualitative research done in Pakistan and Nigeria [18,20].
Conclusion and recommendation
In conclusion, utilization of LAPMs (27.3%) in Debre Berhan was higher as compared to study done in Mekelle (12.3%) and Debre Markos (8.72%). Factors encouraging utilization of LAPMs were acceptance of the method by the women, positive attitude of women towards LAPMs, family planning service satisfaction and women’s age. Common myths and misconception that are barriers to utilization of LAPMs in the community were: IUD and implants can affect daily activities by preventing free movement during up and downs for earning, interfere with sexual intercourse and desire and particularly IUD causes cancer and infertility. Therefore, district health workers should strength behavioral change communication strategies to increase the awareness, to bring positive attitude that may help in correcting misconceptions about IUD and implant. Furthermore, health workers who deliver family planning service should offer adequate counseling and treatment for clients who had problem with methods they use.
Strength and Limitation
Strength
Use of quantitative and qualitative data together with high response rate makes our study strong.
Limitation
Since our investigation was cross-sectional, it was impossible to establish temporal relationship. Besides, the finding did not represent the great majority of the rural community around Debre Berhan town.
Acknowledgement
We authors of this article are glad to express our gratitude to Addis Ababa and Debre Berhan Universities, study participants, data collectors and our families for their full collaboration and encouragement.
Author’s Contribution
WA, MK and SG design the study, conducted analyses and interpretation. BT and KK prepared the manuscript. Furthermore, all authors had read and approved the final manuscript.
References
- UNDESA (2013) World population projected to reach 9.6 billion by 2050. New York
- Jacobstein R (2007) Long-acting and permanent contraception: An international development, service delivery perspective. J Midwifery Women’s Heal 52: 361-367.
- Speizer IS, Nanda P, Achyut P, Pillai G, Guilkey DK (2012) Family planning use among urban poor women from six cities of Uttar Pradesh, India. J Urban Heal 89: 639-658.
- Singh S, Darroch JE (2012) Adding it up: Costs and benefits of contraceptive servicesestimates for 2012. GuttmacherInst United Nations Popul Fund (UNFPA) 201: 1-28.
- Johnson S, Pion C, Jennings V (2013) Current methods and attitudes of women towards contraception in Europe and America. Reprod Health 10: 7.
- Republic FD (2011) National guideline for family planning services in Ethiopic. Federal Democratic Republic of Ethiopia 1-69.
- Stover C, Jansen WI, Khan SA, Chowdhury W (2007) Long-term and permanent methods of family planning in Bangladesh.
- Central Statistical Agency (2011) Ethiopia demographic and health survey 2011. Addis Ababa, Ethiopia and Calverton, Maryland, USA.
- Ko IS, You MA, Kim ES, Lee TW, Kim S, et al. (2010) Family planning practice and related factors of married women in Ethiopia. IntNurs Rev 57: 377-382.
- Emmart P (2010) Policy Barriers to long-acting and permanent method use in Ghana. USAID
- Cleland JG, Ndugwa RP, Zulu EM (2011) Family planning in sub-Saharan Africa: Progress or stagnation? Bull World Health Organ 89: 137-143.
- Alemayehu M, Belachew T, Tilahun T (2012) Factors associated with utilization of long acting and permanent contraceptive methods among married women of reproductive age in Mekelle town, Tigray region, north Ethiopia. BMC Pregnancy Childbirth 12: 6.
- Takele A, Degu G, Yitayal M (2012) Demand for long acting and permanent methods of contraceptives and factors for non-use among married women of Goba Town, Bale Zone, South East Ethiopia. Reprod Health 9: 26.
- Bulto GA, Zewdie TA, Beyen TK (2014) Demand for long acting and permanent contraceptive methods and associated factors among married women of reproductive age group in DebreMarkos Town, North West Ethiopia. BMC Womens Health 14: 46.
- Mekonnen W, Worku A (2011) Determinants of low family planning use and high unmet need in Butajira District, South Central Ethiopia. Reprod Health 8: 37.
- Tilahun T, Coene G, Luchters S, Kassahun W, Leye E, et al. (2013) Family planning knowledge, attitude and practice among married couples in Jimma Zone, Ethiopia. PLoS One 8: e61335.
- Ong J, Temple-Smith M, Wong WC, McNamee K, Fairley C (2012) Contraception matters: Indicators of poor usage of contraception in sexually active women attending family planning clinics in Victoria, Australia. BMC Public Health 12: 1108.
- Khan A, Shaikh BT (2013) An all-time low utilization of intrauterine contraceptive device as a birth spacing method: A qualitative descriptive study in district Rawalpindi, Pakistan. Reprod Health 10: 10.
- Hall MA, Stephenson RB, Juvekar S (2008) Social and logistical barriers to the use of reversible contraception among women in a rural Indian village. J Heal PopulNutr 26: 241-250.
- Babalola S, John N (2012) Factors underlying the use of long-acting and permanent family planning methods in Nigeria: A qualitative study. RESPOND Proj Study SerContrib to Glob Knowledge-Report 5: 3-84.
- Gizaw A, Regassa N (2011) Family planning service utilization in Mojo town , Ethiopia: A population based study. JGRP 4: 355-363.
- Regions T (2004) ETHIOPIA?: Knowledge, attitudes and practices in family planning: Results from September 2004 survey in Amhara, Oromia, SNNPR and Tigray Regions of Ethiopia. USAID
- Gebremariam A, Addissie A (2014) Intention to use long acting and permanent contraceptive methods and factors affecting it among married women in Adigrat town, Tigray, Northern Ethiopia. Reprod Health 11: 24.
- Mavranezouli I, LARC Guideline Development Group (2008) The cost-effectiveness of long-acting reversible contraceptive methods in the UK: Analysis based on a decision-analytic model developed for a national institute for health andclinical excellence (NICE) clinical practice guideline. Hum Reprod 23: 1338-1345.
- Qureshi AM (2010) Case study: Does training of private networks of family planning clinicians in urban Pakistan affect service utilization? BMC Int Health Hum Rights 10: 26.
- Mathe JK, Kasonia KK, Maliro AK (2011) Barriers to adoption of family planning among women in Eastern Democratic Republic of Congo. Afr J Reprod Health 15: 69-77.
- RamaRao S, Lacuesta M, Costello M, Pangolibay B, Jones H (2003) The link between quality of care and contraceptive use. IntFam Plan Perspect 29: 76-83.
- Mekonnen W, Worku A (2011) Determinants of low family planning use and high unmet need in Butajira District , South Central Ethiopia. Reprod Health 8: 37.
- Agha S (2010) Intentions to use contraceptives in Pakistan: Implications for behavior change campaigns. BMC Public Health 10: 450.
Relevant Topics
- Addiction
- Adolescence
- Children Care
- Communicable Diseases
- Community Occupational Medicine
- Disorders and Treatments
- Education
- Infections
- Mental Health Education
- Mortality Rate
- Nutrition Education
- Occupational Therapy Education
- Population Health
- Prevalence
- Sexual Violence
- Social & Preventive Medicine
- Women's Healthcare
Recommended Journals
Article Tools
Article Usage
- Total views: 4508
- [From(publication date):
August-2017 - Jul 11, 2025] - Breakdown by view type
- HTML page views : 3534
- PDF downloads : 974