Research Article Open Access
Abolishment of Alkaline Tide by a Proton Pump Inhibitor (PPI) - An Indication for Successful Therapy in Barrett's Esophagus Patients – A Prospective Study
Maria Raskin and Yaron Niv*Department of Gastroenterology, Rabin Medical Center, Tel Aviv University, Israel
- *Corresponding Author:
- Prof. Yaron Niv
Department of Gastroenterology, Rabin Medical Center
49 Jabotinski Street, Petach Tikva 49100, Israel
Tel: 972-3-9377237
Fax: 972-3-9210313
E-mail: yniv@clalit.org.il
Received date: March 05, 2015; Accepted date: March 23, 2015; Published date: March 28, 2015
Citation: Raskin M, Niv Y (2015) Abolishment of Alkaline Tide by a Proton Pump Inhibitor (PPI) - An Indication for Successful Therapy in Barrett's Esophagus Patients – A Prospective Study. J Gastrointest Dig Syst 5:267. doi:10.4172/2161-069X.1000267
Copyright: © 2015 Raskin M, et al. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution and reproduction in any medium, provided the original author and source are credited.
Visit for more related articles at Journal of Gastrointestinal & Digestive System
Abstract
Introduction: Gastro-esophageal-reflux disease (GERD) and its complication, Barrett's esophagus, are highly prevalent and request medical attention all over the world. Proton pump inhibitors (PPI) are the treatment of choice, acting as gastric acid secretion inhibitors. The transient increase in blood pH following gastric secretion has been termed alkaline tide (AT) phenomenon, and its measurement provides a non-invasive and inexpensive test for evaluation of hypo- and hyper secretory states. Till today it has never been shown that PPI is able to prevent AT, and to optimize treatment for GERD.
Aim: To investigate PPI effect on the AT phenomenon and to ascertain the power of 80 mg pantoprazole to abolish gastric acid secretion.
Methods: The study group comprised of 7 consecutive patients with endoscopically and histologically diagnosed Barrett's Esophagus. Alkaline tide was measured after a test meal, and then the test repeated after a bolus intravenous injection of 80 mg pantoprazole. Base Excess was measured, and AT calculated according to body weight and bicarbonate circulation distribution factor.
Results: Six patients had AT ≥5 mEQ/45min, and included in the study. In all the participants AT was abolished after pantoprazole injection, and a test meal of 400 kcal became ineffective as a stimulus for gastric acid secretion.
Conclusion: In this paper we demonstrate the efficiency of PPI in lowering acid secretion, established the association between gastric acid secretion and AT, and described a way to measure PPI successes in preventing secretion in Barrett's esophagus patients.
Abstract
Introduction: Gastro-esophageal-reflux disease (GERD) and its complication, Barrett's esophagus, are highly prevalent and request medical attention all over the world. Proton pump inhibitors (PPI) are the treatment of choice, acting as gastric acid secretion inhibitors. The transient increase in blood pH following gastric secretion has been termed alkaline tide (AT) phenomenon, and its measurement provides a non-invasive and inexpensive test for evaluation of hypo- and hyper secretory states. Till today it has never been shown that PPI is able to prevent AT, and to optimize treatment for GERD.
Aim: To investigate PPI effect on the AT phenomenon and to ascertain the power of 80 mg pantoprazole to abolish gastric acid secretion.
Methods: The study group comprised of 7 consecutive patients with endoscopically and histologically diagnosed Barrett's Esophagus. Alkaline tide was measured after a test meal, and then the test repeated after a bolus intravenous injection of 80 mg pantoprazole. Base Excess was measured, and AT calculated according to body weight and bicarbonate circulation distribution factor.
Results: Six patients had AT ≥5 mEQ/45min, and included in the study. In all the participants AT was abolished after pantoprazole injection, and a test meal of 400 kcal became ineffective as a stimulus for gastric acid secretion.
Conclusion: In this paper we demonstrate the efficiency of PPI in lowering acid secretion, established the association between gastric acid secretion and AT, and described a way to measure PPI successes in preventing secretion in Barrett's esophagus patients.
Keywords
Alkaline tide; Acid secretion; PPI; Barrett’s esophagus
Introduction
Gastro esophageal reflux disease attacks 10-20% of the Western population [1]. In 5-15% of the patients a premalignant state is developed in the lower esophagus: intestinal metaplasia or Barrett's esophagus. These patients need surveillance of endoscopy and biopsy every 3 years, and when dysplasia developed (in 5%-10% of the cases) – ablation by endoscopic or surgical procedure is performed. American guidelines recommend PPI therapy for these patients [2].
The only role of PPI is to inhibit secretion of gastric acid, and this activity differs between different individual according to several factors such as body weight, parietal cell mass, and in some p450 protein polymorphism [3]. Optimizing PPI dosage seems to be essential for prevention of reflux in Barrett's esophagus patients, thus prevention of dysplasia may be achieved.
The usual dose of pantoprazole used for Barrett's esophagus patients is 40 to 80 mg/d, but nobody has ever demonstrated efficiency in lowering acid secretion or reflux in these patients.
The transient increase in blood pH following gastric secretion [4-7] has been termed the alkaline tide (AT) phenomenon [8]. Carbonic acid, formed in the presence of the enzyme carbonic anhydrase, neutralizes intracellular hydroxyl ions produced as a result of luminal acid secretion.
The bicarbonate generated is removed from the cell via the basolateral chloride bicarbonate exchanger [9]. The significance of the effect of bicarbonate produced during acid secretion on changes in plasma pH is still controversial [10]. There are conflicting data concerning the relationship between gastric acid secretion and the postprandial decrease in urine acidity [6,11].
In addition, it has been argued that pancreatic bicarbonate secretion occurs in parallel to acid secretion and should neutralize the effects of gastric acid secretion [10]. However, we have shown in several studies that this phenomenon parallels acid secretion [7,12].
Thus, stimulation of acid secretion with a test meal increased base excess maximally after 45 minutes and these changes parallel peak acid output measured in the gastric aspirate. Procedures and treatments that reduce acid output also decrease the alkaline tide.
Examples include vagotomy [7,13], H2-receptor antagonists [14], calcium channel blockers [15], and acetazolamide, a carbonic anhydrase inhibitor [16]. The last study supported the direct correlation between gastric acid secretion and alkaline tide.
The measurement of alkaline tide is a convenient, non-invasive and inexpensive test for gastric acid hypo- and hypersecretory states. Arterialized venous blood has been shown to accurately reflect pH in arterial blood, and serial samples are easily obtained with this technique [16].
Studies using this method have confirmed that the alkaline tide is measurable in both blood and urine [7]. Since the production of bicarbonate is dependent on the activity of carbonic anhydrase, inhibition of this enzyme prevented the alkaline tide phenomenon.
Till today the effect of PPIs on the AT phenomenon has never been studied. It is speculated that PPI will abolish completely the AT phenomenon, since it can stop completely gastric acid secretion.
Aim
The primary aim of this study was to investigate PPI effect on the AT phenomenon. Our working hypothesis was that AT disappears after PPI therapy. This effect confirms the adequacy of PPI dosage in Barrett's esophagus patients.
The secondary aim of the study was to ascertain the power of 80 mg pantoprazole, to abolish gastric acid secretion. Failure to achieve this goal dictates increasing the PPI dose. This is a significant decision, since long term high dose PPI may cause osteoporosis and trend for infectious diseases.
Patients and Methods
The study group comprised of 7 consecutive patients with endoscopically and histologically diagnosed Barrett's Esophagus. Pregnant and lactating women, patients less than 18 years of age and patients with renal or pulmonary disease were excluded. Informed consent obtained before enrollment. The study has been reviewed and approved by the Institutional Review Board of the Rabin Medical Center.
Design
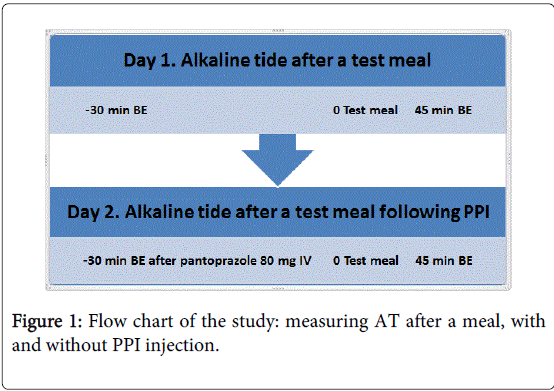
All subjects were asked to stop medication that affects acid secretion or gastric acidity, for at least 7 days prior to the study. After a fast of 9 hours, blood base excess (BE) was determined before and after a test meal (standard sandwich of 400 calories). Subjects who demonstrated an alkaline tide of >5 mEq/h at 45 minutes continued to day 2 (Figure 1).
Alkaline tide lower than 5 mEq/h is not reliable for estimation of gastric acid output, and may be misleading. On day 2, the participants were tested following the administration of intravenous 80 mg pantoprazole (controloc®, Perigo, Petach Tikva, Israel) 30 min before the test meal.
Blood samples
The determination of the alkaline tide was performed as previously described [12]. Briefly, a 21 gauge ''butterfly'' needle was introduced into a vein on the dorsum of the hand. Before each sample taken the hand was immersed in a water bath at 43°C to "arterialize" the venous blood.
At each sampling, 5 ml of blood was drawn and discarded. Two blood samples were then drawn anaerobically in heparinized syringes and analyzed for pO2 and BE, within 5 min, in an automatic blood gas analyzer (AVL OMNI, Graz, Austria). Only samples with pO2>70 mm Hg (arterialized blood) were evaluated. Otherwise, the hand was reimmersed and the procedure repeated. Base excess recorded for each sample was the mean of two determinations.
Data analysis
Alkaline tide (mEq) was calculated as Λ BE (mEq) x 0.3 x body weight (kg). 0.3 is the coefficient of bicarbonate circulation distribution. Results were expressed as the mean ± standard deviation. Observations were compared by paired Student's t-test and P<0.05 was considered significant.
Results
Clinical data are demonstrated in Table 1. Seven patients were enrolled in the study, 2 women and 5 men, with average age of 57.4 years (range 32-75). All had endoscopically and histologically diagnosed Barrett's esophagus, 6 were treated with high dose PPI, and one with low dose. Three patients had short segment, and 4 patients had long segments Barrett's esophagus. Five patients had background diseases, 3 of them had metabolic syndrome.
| Patient | Sex | Age (Y) | Weight (Kg) | Background diseases | PPI therapy | Biopsy results | Prague classification |
| SM | M | 63 | 85 | Obesity | Omeprasole 20mg x 2 | IM | C8M10 |
| Diabetes Mellitus | LGD | ||||||
| Dyslipidemia | |||||||
| PR | M | 75 | 83.5 | Asthma | Omeprasole 20mg x 2 | IM | C2M2 |
| Benign Prostatic Hypertrophy | LGD | ||||||
| GM | F | 67 | 55 | Arterial Hypertension | Omeprasole 20mg x 1 | IM | C0M1 |
| Dyslipidemia | |||||||
| Diverticulosis Coli | |||||||
| DD | M | 45 | 80 | None | Omeprasole 40md x 2 | IM | C5M5 |
| BL | F | 55 | 67.2 | Asthma | Omeprasole 20mg x 2 | IM | C5M5 |
| Dyslipidemia | LGD | ||||||
| AS | M | 32 | 92 | None | Omeprasole 20mg x 2 | IM | C1M2 |
| LGD | |||||||
| BD | M | 65 | 79 | Obesity | Omeprazole 20mg x 2 | IM | C1M3 |
| Arterial Hypertension | LGD | ||||||
| Diabetes Mellitus |
Table 1: Clinical data, N=7. IM: Intestinal Metaplasia, LGD: Low Grade Dysplasia, Prague classification – C: Circumference, M: Maximum Extent.
Six patients had AT ≥5 mEQ/45min, and included in the study. In one patient AT measurement was a negative number and he was excluded from the study.
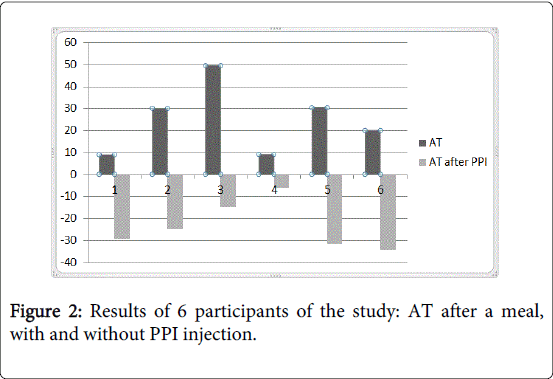
Results of the measurements of BE on Day 1 (after a meal) and on Day 2 (with prior injection of PPI) are demonstrated in Table 2. Calculated AT became a negative number on day 2, after PPI injection, in all the participants.
| Patient | Day I (without PPI injection) | Day II (with PPI injection) | ||||||||
| BE 0 | BE 45 | ΔBE | AT | AT/BW | BE 0 | BE 45 | ΔBE | AT | AT/BE | |
| SM | 0.4 | 0.75 | 0.35 | 8.92 | 0.1 | -0.3 | -1.45 | -1.15 | -29.3 | -0.34 |
| PR | 3.3 | 4.45 | 1.2 | 30 | 0.3 | 3.15 | 2.15 | -1 | -25 | -0.29 |
| GM | -2.8 | 0.2 | 3 | 49.5 | 0.9 | -1.7 | -2.6 | -0.9 | -14.8 | -0.26 |
| DD | -3.5 | -7.5 | -4 | -96 | -1.2 | ND | ND | ND | ND | ND |
| BL | -1.35 | -0.9 | 0.45 | 9.07 | 0.13 | -2.25 | -2.55 | -0.3 | -6 | -0.08 |
| AS | -2.5 | -1.4 | 1.1 | 30.3 | 0.3 | -1.85 | -3 | -1.15 | -31.7 | -0.34 |
| BD | -0.55 | 0.3 | 0.85 | 20 | 0.25 | -0.3 | -1.75 | -1.45 | -34.3 | -0.43 |
| Mean ± SD | -0.6 ± 0.9 | 0.57 ± 0.84 | 1.16 ± 0.39 | 24.63 ± 15.43 | 0.33 ± 0.29 | -0.5 ± 0.8 | -1.53 ± 0.77 | -0.99 ± 0.16 | -23.52 ± 10.97 | -0.28 ± 0.12 |
| Median | -0.95 | 0.25 | 0.98 | 25 | 0.25 | -1 | -2.15 | -1.07 | -27.15 | -0.29 |
Table 2: Results of BE and calculated AT for the participants on Day 1 and Day 2, after a standard meal, with and without PPI injection.
In Table 2 we grouped together the BE and AT results of Day 1 and day 2, with and without PPI injection, and demonstrate the disappearance of AT after PPI injection. Figure 2 demonstrates AT for each patient in both days of the study. After injection of 80 mg pantoprazole a test meal of 400 kcal became ineffective, no acid was secreted into the gastric lumen, and no bicarbonate into the circulation. A negative number for AT calculation has no physiological meaning but zero acid secretion.
Discussion
Optimizing the PPI treatment in patients with GERD and Barrett's esophagus may be important since in addition to endoscopy and biopsy surveillance every 3 years, prevention of acid secretion may be found beneficial. The development of dysplasia on the background of Barrett's mucosa may be prevented if gastro-esophageal acid reflux is prevented. Treatment with high dose of PPI is efficient in this regard, and was successful in all our patients. Alkaline tide, a validated test for gastric acid output rate [12], completely disappeared with 80 mg of pantoprazole, intravenously injected before a standard meal of 400 Kcal. In addition to achievement of our primary goal, we also could demonstrate, in the first time, that PPI can abolish gastric acid secretion completely, prove our secondary goal, and further support the physiological association between gastric acid output and alkaline tide phenomenon [4,5].
Even though PPI therapy is prescribed for a long period for patients with Barrett's esophagus, there is no evidence that this treatment prevents dysplasia or esophageal adenocarcinoma. Thus, we cannot recommend according to our results to continue this strategy, or using specific dose, route of giving the drug or a specific brand. In this paper we demonstrate the efficiency of PPI in lowering acid secretion, and described a way to measure its success in preventing secretion.
References
- Katz PO, Gerson LB, Vela MF (2013) Guidelines for the diagnosis and management of gastroesophageal reflux disease.Am J Gastroenterol 108: 308-328.
- Spechler SJ, Sharma P, Souza RF, Inadomi JM, Shaheen NJ, et al. (2011) American Gastroenterological Association medical position statement on the management of Barrett’s esophagus. Gastroenterology 140: 1084-1091.
- Vela MF (2014) Medical treatments of GERD: the old and new.Gastroenterol Clin North Am 43: 121-133.
- Rune SJ (1965) The metabolic alkalosis following aspiration of gastric acid secretion.Scand J Clin Lab Invest 17: 305-310.
- Rune SJ (1966) Comparison of the rates of gastric acid secretion in man after ingestion of food and after maximal stimulation with histamine.Gut 7: 344-350.
- Johnson CD, Rai AS (1990) Urine acid output as a test of completeness of vagotomy.Br J Surg 77: 417-420.
- Niv Y (1992) Pentagastrin-induced urinary alkaline tide--a repeatable phenomenon that is abolished after vagotomy.Isr J Med Sci 28: 97-98.
- Moore EW (1967) The alkaline tide.Gastroenterology 52: 1052-1054.
- Gleeson D (1992) Acid-base transport systems in gastrointestinal epithelia.Gut 33: 1134-1145.
- Johnson CD, Mole DR, Pestridge A (1995) Postprandial alkaline tide: does it exist?Digestion 56: 100-106.
- Vaziri ND, Byrne C, Ryan G, Wilson A (1980) Preservation of urinary postprandial alkaline tide despite inhibition of gastric acid secretion.Am J Gastroenterol 74: 328-331.
- Niv Y, Abu-Avid S, Neumann G (1993) Further applications of blood gas analysis to gastric acidity determination.Clin Chim Acta 215: 9-19.
- Ahmad A (1986) Abolition of postprandial alkaline tide after vagotomy and its use as a screening test in the assessment of vagotomy.Br J Surg 73: 917-919.
- Niv Y, Asaf V (1995) Abolition of postprandial alkaline tide in arterialized venous blood of duodenal ulcer patients with cimetidine and after vagotomy.Am J Gastroenterol 90: 1135-1137.
- Niv Y, Vardi I (1995) Calcium channel blocker decreases pentagastrin-stimulated alkaline-tide: a role for extracellular calcium in gastric acid secretion.Isr J Med Sci 31: 215-217.
- Regev A, Drori R, Fraser GM, Niv Y (2001) Abolition of pentagastrin-stimulated alkaline tide using the carbonic anhydrase inhibitor acetazolamide.Isr Med Assoc J 3: 247-250.
Relevant Topics
- Constipation
- Digestive Enzymes
- Endoscopy
- Epigastric Pain
- Gall Bladder
- Gastric Cancer
- Gastrointestinal Bleeding
- Gastrointestinal Hormones
- Gastrointestinal Infections
- Gastrointestinal Inflammation
- Gastrointestinal Pathology
- Gastrointestinal Pharmacology
- Gastrointestinal Radiology
- Gastrointestinal Surgery
- Gastrointestinal Tuberculosis
- GIST Sarcoma
- Intestinal Blockage
- Pancreas
- Salivary Glands
- Stomach Bloating
- Stomach Cramps
- Stomach Disorders
- Stomach Ulcer
Recommended Journals
Article Tools
Article Usage
- Total views: 17751
- [From(publication date):
April-2015 - Jul 12, 2025] - Breakdown by view type
- HTML page views : 13081
- PDF downloads : 4670