Abernethy Malformation: A Vascular Aberration
Received: 02-Nov-2018 / Accepted Date: 15-Mar-2019 / Published Date: 25-Mar-2019 DOI: 10.4172/2161-069X.1000594
Abstract
Aims: To evaluate and asses rare congenital extrahepatic portosystemic shunts and their associated systemic manifestations.
Methods and Material: Pediatric patients presenting to the hospital for CECT (Contrast Enhanced Computed Tomography)/MRI (Magnetic Resonance Imaging) evaluation were assessed and any portal vascular abnormalities were documented and evaluated accordingly. 64 slice Phillips scanner and 3.0 tesla Phillips achieva MRI was used to acquire images.
Results and Conclusions: Abernethy malformation (CEPS) is a rare vascular aberration which when detected early and specifically characterized can help in early treatment and intervention altering the prognosis for the patient.
Keywords: Abernethy malformation; Triphasic CT (Computed Tomography); MRI; Types; associations
Key Messages
Abernethy malformation is rare anomaly. A high index of suspicion, sub-characterization and early diagnosis can aid in diagnosis. CT/MRI imaging is of paramount importance for pre-operative planning and management.
Introduction
Abernethy malformation or Congenital Extrahepatic Portosystemic Shunt (CEPS) is an uncommon entity and has been classified into two types. In abernethy malformation there is complete or partial shunting of hepatic venous supply of the porto-mesenteric blood, which drains into a systemic vein. It was reported for the first time in 1793 by John Abernethy [1].
Classification is based on the configuration of anastomosis between the two hepatic venous channels naming the Inferior Vena Cava (IVC) and Portal Vein (PV), and is governed by the presence or absence of an intrahepatic portal venous supply. In Type I, entire portal venous supply drains into the IVC with near complete absence of the intrahepatic portal venous supply. In Type II, the portal venous blood partially drains into the IVC through side-to-side anastomosis. It is crucial to identify and delineate amongst the two types, as the definitive method of treatment is separate for the two entities (Figure 1) [2,3].
The associated manifestations are primarily of clinical significance naming nodular liver lesions and congenital heart defects and may later fulminate into liver dysfunction and hepatic encephalopathy.
Case 1
A 7-year-old boy presented with retarded physical growth and epistaxis since 1 year. His body weight was 14 kg (less than 3 standard deviation) and height 118 cm (between less than 10 and less than 3 standard deviation). Liver function tests showed total bilirubin levels of 7.64 mg/dl , indirect bilirubin level of 2.3 mg/dl, ALT(Alanine Aminotransferase) level of 84 IU/cc. BT (Bleeding Time), CT (Clotting Time), INR (International Normalized ratio) were within normal limits. Alpha-feto protein levels and hepatic viral serology was normal.
CT scan of abdomen and pelvis was performed. It revealed evidence of mild hepatomegaly with multiple soft-tissue density lesions of varying-sizes involving both lobes of liver. Triphasic contrast study was performed. No evident significant enhancement was seen within the lesions on angiography phase. Portal-venous phase reveals multiple poorly enhancing lesions at the above sites. Two lesions were seen in segment VI-VII and III of liver showing enhancement on portalvenous phase. Delayed venous phase shows complete washout of contrast from the lesions. A central persistent enhancing focus was seen in few of the lesions in left lobe of liver.
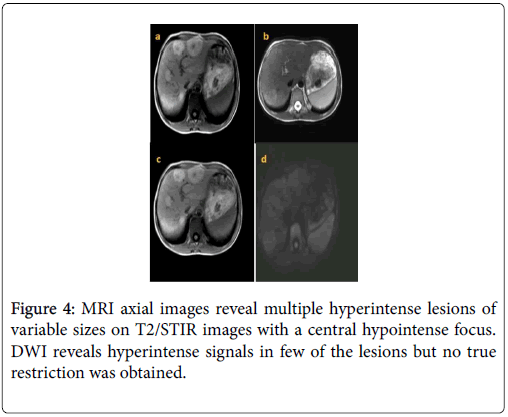
The main portal vein and its branches were absent; however superior mesenteric vein and splenic vein could be traced. They fused to form a short extra-hepatic portal vein draining into sub-hepatic inferior vena cava suggestive of Type-Ib Abernethy malformation. No evident venous thrombosis was noted. MRI liver (T1W (T1 Weighted imaging), T2W (T2 Weighted imaging) and DWI (Diffusion Weighted Imaging)) was performed which revealed multiple altered signal intensity lesions of varying-sizes involving both lobes of liver. They appeared hypo-to-hyperintense on T2W images and appear hyperintense on T1W images. Diffusion weighted images reveals mild diffusion restriction in lesions in segment VI-VII and III of liver. Rest of the lesions does not show significant restriction.
Image guided percutaneous trucut biopsy of the liver nodules was performed. Histopathology revealed hepatocytes with thick walled arteries and proliferation of bile ducts separated by fibrotic bands which lacked portal channels. These features were pointed towards tissue diagnosis of FNH (Focal Nodular hyperplasia) (Figure 2-4).
Case 2
A 2-year-old male child with altered sensorium, increased serum bilirubin and deranged hepatic enzymes, raised PT and INR presented to the hospital. CECT Triphasic scan the abdomen revealed a fusiform aneurysmally dilated main portal vein, which continued as the left branch for a short distance ending abruptly. The right branch of PV was non-visualized. An abnormal side-to-side shunt between the extrahepatic MPV and the IVC was observed. The patient was referred to interventional radiologist for closure of the shunt but was lost to follow-up thereafter (Figure 5).
Discussion
Aberration in the involution process of the embryologically formed anastomoses between the vitelline venous pair (which eventually forms the portal vein),results in the abnormal development of portal system and its anatomical variations giving rise to Congenital Extrahepatic Portosystemic Shunt (CEPS) or Abernethy malformation [4-6]. CEPS with near total absence of portal vein are defined as Type I. It is further sub-classified into types Ia and Ib according to the course of the splenic and mesenteric veins. Partial shunts with a residual degree of portal venous supply to the liver are defined as type II.
Apart from non-existence of portal vein, numerous associated liver lesions have been documented in majority of the reported cases with preponderance of Focal Nodular Hyperplasia (FNH). The incidence of such lesions has been attributed to increase in hepatic arterial supply secondarily due to absent portal venous flow [7-9]. An alternative hypothesis recounts the absence of portal hepatotrophic factors with systemic shunting of the visceral venous return, as a trigger for development of hepatic lesions, due to defunct proliferationregeneration mechanism of the liver. Other reported plethora of lesions included hepatic adenoma, hepatoblastoma, hepatocellular carcinoma and in few cases cirrhosis.
Many congenital cardiac diseases have been documented as associated with CEPS, few being- atrial septal defect, Ventricular septal defect, patent ducts arteriosus & patent foramen ovale [10]. Other associated abnormalities include situs ambiguous, malrotation, polysplenia, annular pancreas, duodenal atresia, skeletal anomalies and genitourinary malformations. The associations are more commonly seen in patients with type I CEPS, with the exception of anomalies of renal tract which are evenly distributed (Table 1).
| Anomalies associated with abernethy malformation | ||
|---|---|---|
| Cardiovascular Anomalies | Gastrointestinal Anomalies | Genitourinary Anomalies |
| •ASD | •Liver lesions | •Multicystic dysplastic kidney |
| •VSD | •Polysplenia | •Bilateral ureteropelvic stenosis |
| •PDA | •Biliary atresia | •Vesicoureteral reflux |
| •TOF | •Choledochal cyst | •Crossed fused renal ectopia |
| •PFO | - | •Hypospadias |
| Dextrocardia, Mesocardia | Skeletal Anomalies | - |
| - | Vascular Anomalies | - |
| - | •Interruption of the IVC | - |
| - | •Double IVC | - |
Table 1: The management of each case is different and is determined by the type, clinical scenario and symptomatology of patient.
Treatments options comprise of vascular interventional procedures like balloon-occluded retrograde trans-venous obliteration or embolization with metallic coils. Surgical occlusion of shunts may be attempted. Liver transplantation is deemed as the last resort. Emergency scenarios of hepatic encephalopathy or bleeding entail urgent occlusion of the shunt [11].
The diagnosis of Abernethy malformation and its associated anomalies is intricate and it is quintessential to detect and decipher other associated cardiovascular and hepatic anomalies. The long-term prognosis is dependent on satisfactory control of the metabolic derangements and regulation of hepatic function. A multi-disciplinary approach with early diagnosis and intervention is primordial to categories and effectively treat CEPS [12].
Conflicts of Interest
Conflict of interest disclosed was none.
References
- Abernethy J (1793) Account of two instances of uncommon formation in the viscera of the human body. Philos Trans R Soc 83:59-66.
- Alonso-Gamarra E, Parrón M, Pérez A, Prieto C, Hierro L, et al.( 2011) Clinical and radiologic manifestations of congenital extrahepatic portosystemic shunts: A comprehensive review. Radiographics 31:707-22.
- Howard ER, Davenport M (1997) Congenital extrahepatic portocaval shunts-the Abernethy malformation. J Pediatr Surg 32:494-497
- De Gaetano AM, Gui B, Macis G, Manfredi R, Di Stasi C (2004) Congenital absence of the portal vein associated with focal nodular hyperplasia in the liver in an adult woman: Imaging and review of the literature. Abdom Imaging 29:455-459.
- Turkbey B, Karcaaltincaba M, Demir H, Akcoren Z, Yuce A, et al. (2006) Multiple hyperplastic nodules in the liver with congenital absence of portal vein: MRI findings.Pediatr Radiol 36:445-448.
- Kinjo T, Aoki H, Sunagawa H, Kinjo S, Muto Y (2001) Congenital absence of the portal vein associated with focal nodular hyperplasia of the liver and congenital choledochal cyst: A case report. J Pediatr Surg 36:622−625.
- Kumar A, Kumar J, Aggarwal R, Srivastava S (2008) Abernethy malformation with portal vein aneurysm. Diagn Interv Radiol 14:143-146.
- Tanaka Y, Takayanagi M, Shiratori Y, Imai Y, Obi S,et al. (2003) Congenital absence of portal vein with multiple hyperplastic nodular lesions in the liver. J Gastroenterol 38:288-294.
- Kondo F, Nagao T, Sato T, Tomizawa M, Kondo Y, et al.(1998) Etiological analysis of focal nodular hyperplasia of the liver, with emphasis on similar abnormal vasculatures to nodular regenerative hyperplasia and idiopathic portal hypertension. Pathol Res Pract 194:487-495.
- Morse SS, Taylor KJ, Strauss EB, Ramirez E, Seashore JH (1986) Congenital absence of the portal vein in oculoauriculovertebral dysplasia (Goldenhar syndrome). Pediatr Radiol 16:437-439.
- Barton JW 3rd, Keller MS (1989) Liver transplantation for hepatoblastoma in a child with congenital absence of the portal vein. Pediatr Radiol 20:113-114.
- Naeije R (2003) Hepatopulmonary syndrome and portopulmonary hypertension. Swiss MedWkly 133:163−169.
Citation: Saxena S, Patel D, Mishra S, Jha SAK (2019) Abernethy Malformation: A Vascular Aberration. J Gastrointest Dig Syst 9: 594. DOI: 10.4172/2161-069X.1000594
Copyright: © 2019 Saxena S, et al. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.
Select your language of interest to view the total content in your interested language
Share This Article
Recommended Journals
Open Access Journals
Article Tools
Article Usage
- Total views: 4579
- [From(publication date): 0-2019 - Nov 06, 2025]
- Breakdown by view type
- HTML page views: 3674
- PDF downloads: 905