Review Article Open Access
Abdominal Cocoon A Rare Complication of Abdominal Tuberculosis
Rajul Rastogi*
Teerthanker Mahaveer University, Moradabad, Uttar Pradesh, India
- *Corresponding Author:
- Rajul Rastogi
Assistant Professor, Teerthanker Mahaveer University
Radiodiagnosis, Moradabad
Uttar Pradesh, India
Tel: 919319942162
E-mail: eesharastogi@gmail.com
Received date: June 22, 2015;Accepted date: July 01, 2015; Published date: July 16, 2015
Citation: Rastogi R (2015) Abdominal Cocoon – A Rare Complication of Abdominal Tuberculosis. J Gastrointest Dig Syst 5:309. doi:10.4172/2161-069X.1000309
Copyright: © 2015 Rastogi R. This is an open-access article distributed under the terms of the Creative Commons Attribution License; which permits unrestricted use; distribution; and reproduction in any medium; provided the original author and source are credited.
Visit for more related articles at Journal of Gastrointestinal & Digestive System
Abstract
Tuberculosis is a common infectious disease in an Indian subcontinent. Abdominal tuberculosis is one of the commonest forms of extrapulmonary tuberculosis (next only to tubercular lymphadenitis) encountered in clinical practice. Among the various manifestations of abdominal tuberculosis, abdominal cocoon also referred to as sclerosing peritonitis or sclerosing encapsulating peritonitis is one of the most bizarre and difficult to treat manifestation. The present review article discuss abdominal cocoon secondary to abdominal tuberculosis with characteristic imaging features.
Abstract
Tuberculosis is a common infectious disease in an Indian subcontinent. Abdominal tuberculosis is one of the commonest forms of extrapulmonary tuberculosis (next only to tubercular lymphadenitis) encountered in clinical practice. Among the various manifestations of abdominal tuberculosis, abdominal cocoon also referred to as sclerosing peritonitis or sclerosing encapsulating peritonitis is one of the most bizarre and difficult to treat manifestation. The present review article discuss abdominal cocoon secondary to abdominal tuberculosis with characteristic imaging features.
Keywords
Cocoon; Tuberculosis; Computed tomography; Magnetic resonance imaging
Introduction
Abdominal cocoon is not only a rare complication of abdominal tuberculosis but also a rare cause of intestinal obstruction [1]. As this condition is characterised by thickening and fibrosis of peritoneum with subsequent wrapping of the variable length of small and sometimes, large bowel in a stack or concertina pattern, it is also known as peritonitis chronic fibrosa incapsulata or sclerosing encapsulating peritonitis [2]. This condition is difficult to diagnose clinically but can be easily recognised by imaging. Early recognition allows early management and may prevent the need for operative intervention or bowel resection.
Discussion
The term abdominal cocoon was coined by Foo et al in 1978 [3]. Various etiologic factors including previous abdominal surgery, peritonitis, chronic ambulatory peritoneal dialysis, prolonged use of the ß-blockers like practolol/propranolol, ventriculoperitoneal shunts, granulomatous diseases like sarcoidosis and tuberculosis, autoimmune diseases like systemic lupus erythematosus, viral infections, etc. have been implicated [1,4]. Geographically, the condition is predominantly seen in the tropical regions and mainly in young females.
Abdominal cocoon involves predominant encasement of a part or entire small bowel by a thick, opaque, dense and fibrous membrane. Patient may present clinically with abdominal pain or variable degrees of intestinal obstruction especially with vomiting and abdominal distension and often a soft, non-tender lump in mid-abdomen. Though, multiple studies in the form of case reports or case series have reported the occurrence of abdominal cocoon in the medical literature, yet it occurrence and diagnosis creates a dilemma especially in patients of abdominal tuberculosis [1,4-7].
Imaging Findings
X-ray abdomen in erect or supine may reveal mildly dilated small bowel loops with or without air-fluid levels in the mid-abdomen representing features of subacute to acute intestinal obstruction. Signs of tuberculosis on X-ray chest may be adjunctive in establishing the etiology.
Classic barium finding include serpentine/concertina pattern of dilated small bowel loops in a fixed U-shaped cluster [5,8] or a "cauliflower sign"; latter however is nonspecific. There is associated delayed transit of contrast in small-intestine. Fluoroscopy may reveal failure of bowel loops to separate on application of intra-abdominal pressure.
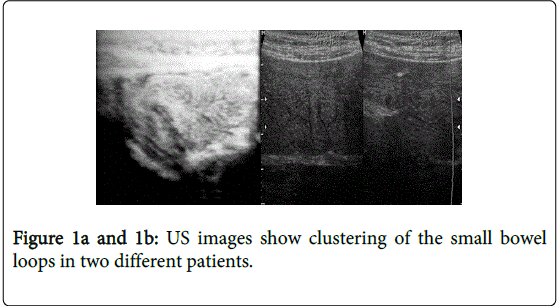
Ultrasonographic findings (Figure 1a and 1b) include clustering of small bowel loops in anterior and middle part of abdominal cavity with narrow posterior base representing cauliflower pattern associated with mural thickening of bowel loops, altered bowel peristalsis, adherence to anterior abdominal wall and to each other, interloop fluid with echogenic strands, mesenteric/omental adenopathy and thin or thick membrane formation during the late stage of the disease [7,9,10]. Bowel loop separation may not be achieved on applying pressure with ultrasound probe. Repeated scans may fail to reveal any change in the bowel loop appearance representing adhesion/agglutination of bowel loops.
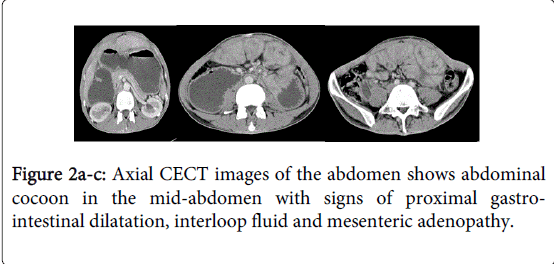
CT features (Figure 2a-2c) include clustering of partial to whole small bowel in mid-abdomen with agglutination and encasement by a membrane of variable thickness [11,12]. Other features include signs of obstruction, angulations of intestinal loops representing interloop adhesions, bowel mural thickening, interloop or free ascites, peritoneal thickening and enhancement, peritoneal or bowel mural calcifications and reactive adenopathy [4]. The cluster of bowel loop may be apparently adherent to the anterior abdominal wall. Delineating extent of encapsulation especially on the posterior aspect is decisive in determining the need of surgical intervention making CT abdomen, the investigation of choice in suspected cases of abdominal cocoon.
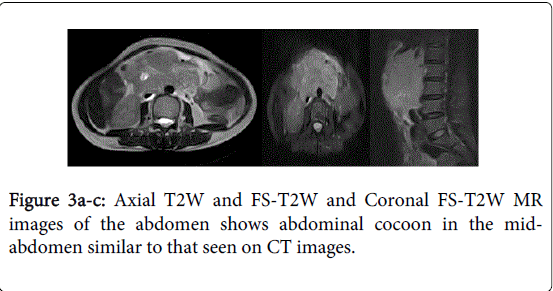
MRI features: Though a search of medical literature has not revealed description of MRI findings in cases of abdominal cocoon. But in our experience, the findings parallel those that seen on computed tomography. Though computed tomography is usually preferred over magnetic resonance imaging in the evaluation of abdominal cocoon yet the latter may be a preferred technique in patients with contraindication to CT contrast agents (Figure 3a-3c).
Prior to CT/MRI, the correct diagnosis was usually made at surgery [5,6]. The characteristic feature noted in these cases is the absence of greater omentum in the region of involved small bowel. The treatment is rarely conservative and consists of surgically freeing the bowel loops of adhesions between loops and the capsule/cocoon wall and removal of encapsulating membrane. Late cases may require resection of the necrotic/narrowed portion of bowel loops with end-to-end anastomosis. Perforation is a rare complication.
Microscopic examination of capsule/covering membrane reveals presence of vascular, fibrous and collagenous components associated with variable chronic inflammatory infiltrate showing presence of lymphocytes or plasma cells; presence of caseating, epithelioid granuloma; and reactive or caseating mesenteric adenopathy [7,13]. Acid fat bacilli may or may not be isolated on culture. Ascitic fluid may reveal increased ADA levels.
Conclusion
Abdominal cocoon secondary to abdominal tuberculosis is a rare acquired condition characterised by encapsulation of small bowel by a fibrous membrane associated with interloop adhesions. This condition can be confidently diagnosed by utilizing various radiological investigations. Early recognition results in appropriate management and prevents extensive surgical treatment.
References
- Rastogi R (2008) Abdominal cocoon secondary to tuberculosis.Saudi J Gastroenterol 14: 139-141.
- Tsunoda T, Mochinaga N, Eto T, Furui J, Tomioka T, et al. (1993) Sclerosing encapsulating peritonitis combined with peritoneal encapsulation.Arch Surg 128: 353-355.
- Foo KT, Ng KC, Rauff A, Foong WC, Sinniah R (1978) Unusual small intestinal obstruction in adolescent girls: the abdominal cocoon.Br J Surg 65: 427-430.
- Krestin GP, Kacl G, Hauser M, Keusch G, Burger HR, et al. (1995) Imaging diagnosis of sclerosing peritonitis and relation of radiologic signs to the extent of the disease.Abdom Imaging 20: 414-420.
- Sieck JO, Cowgill R, Larkworthy W (1983) Peritoneal encapsulation and abdominal cocoon. Case reports and a review of the literature.Gastroenterology 84: 1597-1601.
- Hur J, Kim KW, Park MS, Yu JS (2004) Abdominal cocoon: preoperative diagnostic clues from radiologic imaging with pathologic correlation.AJR Am J Roentgenol 182: 639-641.
- Sarmast AH, Showkat HI, Sherwani A, Kachroo MY, Parray FQ (2012) Abdominal tuberculosis with a cocoon.Iran Red Crescent Med J 14: 503-504.
- Sahoo SP, Gangopadhyay AN, Gupta DK, Gopal SC, Sharma SP, et al. (1996) Abdominal cocoon in children: a report of four cases.J PediatrSurg 31: 987-988.
- Hollman AS, McMillan MA, Briggs JD, Junor BJ, Morley P (1991) Ultrasound changes in sclerosing peritonitis following continuous ambulatory peritoneal dialysis.ClinRadiol 43: 176-179.
- Wani I, Ommid M, Waheed A, Asif M (2010) Tuberculous abdominal cocoon: original article.UlusTravmaAcilCerrahiDerg 16: 508-510.
- Wig JD, Gupta SK (1998) Computed tomography in abdominal cocoon.J ClinGastroenterol 27: 259-260.
- Neslihan T, Alp D, Murat K, Bengi G, Nuri O, et al. (2009) Intestinal Obstruction due to abdominal cocoon: CT findings. European Journal of Radiology Extra 70: e79-e81.
- Kaushik R, Punia RP, Mohan H, Attri AK (2006) Tuberculous abdominal cocoon--a report of 6 cases and review of the Literature.World J EmergSurg 1: 18.
Relevant Topics
- Constipation
- Digestive Enzymes
- Endoscopy
- Epigastric Pain
- Gall Bladder
- Gastric Cancer
- Gastrointestinal Bleeding
- Gastrointestinal Hormones
- Gastrointestinal Infections
- Gastrointestinal Inflammation
- Gastrointestinal Pathology
- Gastrointestinal Pharmacology
- Gastrointestinal Radiology
- Gastrointestinal Surgery
- Gastrointestinal Tuberculosis
- GIST Sarcoma
- Intestinal Blockage
- Pancreas
- Salivary Glands
- Stomach Bloating
- Stomach Cramps
- Stomach Disorders
- Stomach Ulcer
Recommended Journals
Article Tools
Article Usage
- Total views: 16796
- [From(publication date):
August-2015 - Jul 15, 2025] - Breakdown by view type
- HTML page views : 12176
- PDF downloads : 4620