A Wearable Device Provides an Alternate Measurement of Free-Living Eating Rate
Received: 04-Oct-2018 / Accepted Date: 17-Oct-2018 / Published Date: 22-Oct-2018
Abstract
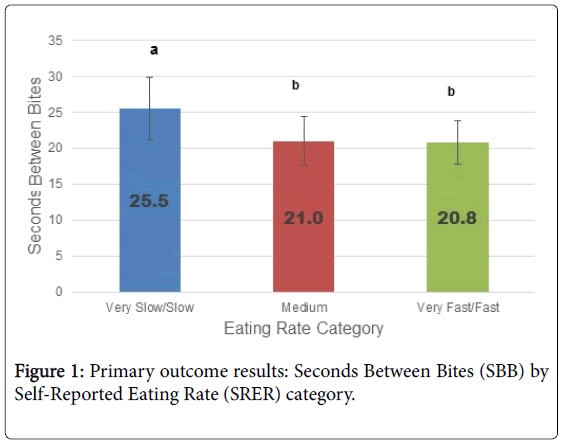
Eating rate, defined as the consumption of food per unit of time, has been associated with energy intake and obesity. However, eating rate is difficult to measure, necessitating most studies to rely on self-reported eating rate (SRER). The wrist-worn Eat Less Move More (ELMM) device has been validated to count bites by detection of a wrist-roll motion specific to eating, but has not yet been used to measure seconds between bites, as a proxy to eating rate, in free-living settings. We aimed to examine ELMM-assessed eating rate in free-living settings compared to SRER. This was a secondary analysis of the initial three days of seconds between bites data from an 8-week weight loss intervention. Participants (n=37; 62.2% female; age 36.5 ± 16.1 years; BMI 31.2 ± 3.5 kg/m2) ranked their SRER and tracked their eating in free-living settings by turning the ELMM on and off at start/end of meals. Based on baseline data, five SRER categories were collapsed into three groups: very slow/slow (n=5), medium (n=12), and fast/very fast (n=16). One-way ANOVA examined SRER group differences in average seconds between bites.There was a significant difference in seconds between bites among SRER groups (SBB, M ± SD: slow=25.5 ± 4.3, medium=21.0 ± 3.4, and fast=20.8 ± 3.0). Tukey tests showed lower average seconds between bites, indicating faster eating, in the fast SRER group compared to the slow SRER group. Lower average seconds between bites was seen in the medium SRER group compared to the slow SRER group, but there was no difference between the medium and fast SRER groups.The ELMM assessed average seconds between bites during eating occasions, and seconds between bites corresponded to SRER. Future work should assess eating rate with ELMM in larger samples and in other populations.
Keywords: Eating rate; Speed of eating; Self-monitoring; Obesity; Wearable device; Wrist-worn device; Seconds between bites
Introduction
Obesity remains highly prevalent in the United States, with approximately 67% of adults classified as overweight, and 35% as obese [1,2]. One behavior that has been associated with obesity is eating rate, defined as the amount of food consumed per unit of time [3-6]. Population studies have demonstrated a positive association between eating rate and weight gain over time. In a study exploring predictors of weight gain in a sample of 438 fire service workers, those who reported at baseline a faster eating rate while at work experienced a significantly increased weight after seven years [5]. In a sample of 529 male Japanese workers, those who self-reported as fast eaters had significantly higher weight and BMI at two different time points 8 years apart [6]. Furthermore, when compared to slow eaters, the fast eaters gained significantly more weight between the two time points [6]. Studies have also demonstrated a relationship between eating rate and obesity; a systematic review and meta-analysis of 23 studies, mostly cross-sectional, found a positive association between eating rate and obesity[3]. In addition to its establishment as a potential underlying contributor of obesity [3,7], a rapid eating rate has also been positively associated with excess body fat and central fat distribution [8,9], as well as insulin resistance [10,11]
Faster eating rates have also been shown to be positively associated with energy intake in experimental studies. In a randomized crossover design examining eating rate and energy intake in both normal weight and obese participants, those in a fast eating condition had a higher energy intake compared to those in a slow eating condition [12]. Moreover, decreasing eating rate has been associated with reductions in energy intake in 30 healthy young women [13]. A systematic review and meta-analysis demonstrated that slower eating rates led to significantly reduced food intake, and that the measure for eating rate reduction did not matter, as all led to reduced intake [14]. Results from that meta-analysis also showed that greater reductions in eating rate were associated with greater reductions in energy intake. This information provides a solid foundation for further consideration of eating rate as a potential key behavior in obesity management.
Given the significance of the relationship between eating rate and obesity and energy intake, new ways to measure eating rate should be explored. There is a need for tools to assess eating rate within weight management strategies. However, eating rate is difficult to measure.
Only two studies to date have validated Self-Reported Eating Rate (SRER) against laboratory-measured eating rate [15,16]. One study compared SRER to laboratory measured eating rate in 60 healthy male and female college students [16], and found that participants who self-reported faster eating rate ate significantly faster in the laboratory than those who self-reported slow eating rates. Another study demonstrated that SRER was positively associated with measured laboratory eating rate when participants consumed three different foods within one eating occasion in the laboratory [15]. However, researchers have not been able to validate free-living eating rate against SRER, because there has previously not been a way to collect eating rate data in free living eating situations. Thus, the use of self-reported eating rate (SRER) is a limitation of most research studies in this area. If eating rate can be objectively measured, a new method of self-monitoring for weight reduction could be identified.
The Eat Less, Move More (ELMM) device, also known as the Bite Counter, is a tool that counts bites taken to track energy intake [17]. The ELMM is easy to use, can be worn like a watch, and is unique in that it is the only wearable device that can measure bite count without record keeping or calorie counting. The device is able to detect bites that occur with a minimum of six seconds between bites [18]. It has been validated in both the controlled laboratory setting and in free-living conditions to have a high sensitivity in detecting number of bites taken and a positive, moderate correlation between bites and kilocalories consumed [17,19]. A newer feature of the device is its ability to display the average number of seconds between bites (SBB) after each eating occasion [18], as an alternative form of eating rate measurement. While this number is not displayed throughout the meal, the user, upon ending the meal, can press a button on the device to see the average number of SBB of that meal. Previously no technology has been available that can assess any measure of eating rate outside of the laboratory, and the application of this device-assessed form of eating rate in free-living settings has not been previously tested. Therefore, this technology should be examined for its ability to assess free-living eating rate.
Although previous research has validated SRER against laboratory-measured eating rate [15,16] no research has examined eating rate as assessed by the ELMM device against SRER or laboratory-measured eating rate. Additionally, research has demonstrated that SRER is positively associated with BMI, and that individuals with obesity have been shown to have faster eating rates than those with a healthy BMI [7,15], yet no study has examined free-living eating rate assessment in individuals with obesity. Therefore the primary aim of this study was to examine free-living eating rate as assessed by the ELMM compared to SRER in a sample of individuals who were overweight or obese. The secondary aim of this study was to validate free-living eating rate as assessed by the ELMM (in SBB) against laboratory-measured eating rate. A tertiary objective was to compare laboratory-measured eating rate against SRER in adults with overweight and obesity.
Material and Methods
Study design and participants
This was a secondary analysis examining data from 37 participants who were recruited and randomized into the experimental group of an eight-week weight loss intervention. Non-smoking participants, ages 18-60 years, with overweight or obesity (body mass index [BMI]= 25.0-40.0 kg/m2) who were interested in losing weight were recruited from July 2016 to June 2017 from the University of Rhode Island campus in Kingston, RI and its surrounding areas. Participants were not pregnant or lactating, not taking any medications that may affect appetite, and had no metabolic disease or conditions that may impact their appetite, including diabetes, unmanaged thyroid disease, or eating disorders. Participants provided informed written consent to participate in the study, which was approved by the University of Rhode Island’s Institutional Review Board.
Procedures
Participants came into the lab for a total of three individual visits. For the purpose of this study, the first two visits are relevant. During the first visit, participants signed an informed consent, and anthropometrics were taken to assure eligibility to take part in the study. Participants were asked to characterize their eating rate on a 5- point scale according to the following categories: very slow; slow; medium; fast; and very fast. This scale has been used in previous research [4,6,7,15,16] and found to have good validity for in-laboratory eating rate measurement using the test-retest model [20]. Participants were instructed to return to the lab one week later after a 10 h fast with no caffeine or exercise before the scheduled visit.
Upon return to the lab for the second visit, anthropometrics were taken for descriptive purposes. Then, an ad libitum standardized test meal was served in a separate area of the lab. Participants were offered a choice of instant oatmeal flavors: maple brown sugar (491.1 g, 819.6 kcal= 1.67 kcal/g) or cinnamon spice flavor (=497.1 g, 845.6 kcal, 1.7 kcal/g). The mixed macronutrient standardized test breakfast consisted of oatmeal enriched with protein powder and mixed with milk and butter to provide 53% carbohydrate, 15% protein and 32% fat as analyzed by the Food Processor SQL (ESHA Research, Salem, OR). Participants were offered a choice of spring water, hot decaffeinated coffee or hot decaffeinated tea with no additives, and were told to eat as they normally would, until comfortably full. The UEM computer recorded the exact start and stop times of the meal, as well as pre- and post-weight of the meal in grams. Eating rate of the meal was calculated using both grams and kcalories consumed, divided by the number of minutes of meal duration. After the test meal, participants were educated on how to use the ELMM outside of the lab for all meals and snacks, and were instructed to turn it on at the start of each meal and off at the end of each meal.
The ELMM tracked number of bites taken during each meal, along with total meal duration of participants. Eating rate as assessed by the ELMM is measured in units of seconds between bites (SBB). A lower SBB number indicates a faster eating rate, as there are on average fewer seconds, or less time, between bites throughout the meal. For the purpose of this study, data from the first three days of recorded eating occasions were examined to measure SBB. If participants did not use the device for a day during the first three days, that day was coded as missing. To assess lab-measured eating rate for the secondary outcome, UEM-measured test meal data from the second laboratory visit were used.
Statistical analysis
All statistical analyses were performed with SPSS 24 (Statistical Package for Social Sciences, IBM-SPSS Inc., Armonk, New York). Descriptive statistics were used to summarize demographics using means, standard deviations, frequencies and percentages, and skewness and kurtosis of all variables was examined. The primary outcome, ELMM-assessed eating rate (in SBB measured by the device), was examined using one-way analysis of variance (ANOVA) to determine group differences among SRER categories. The five eating rate categories were collapsed into three categories due to the low number of participants who self-reported their eating in the extreme categories (“very slow”, n=1, and “very fast”, n=6). Therefore the “very slow” and “slow” categories were combined into one “slow” category, and the “fast” and “very fast” categories were combined into one “fast” category. After applying three standard deviations to these data, no influential outliers were identified. Pearson’s correlations explored secondary outcome associations between ELMM-assessed eating rate (in SBB) and UEM-measured eating rate. One-way ANOVA and Spearman’s correlations examined tertiary outcome SRER group differences and associations among UEM-measured eating rate and SRER categories. All statistical tests were two-tailed, and considered significant with p values of <0.05.
Results
Participant characteristics are presented in Table 1. Participants (n=37) were mostly women (62.2%), Caucasian (69%), had a mean age of 36.5 ± 16.1 years, and a mean BMI of 31.2 ± 3.5 kg/m2. There were no statistically significant differences among SRER groups in age, BMI, sex, race or ethnicity.
| Characteristic | (n=37) |
|---|---|
| Mean ± SD | |
| Age, years | 36.5 ± 16.1 |
| Body mass index (kg/m2) | 31.2 ± 3.5 |
| Sex, n (%) | |
| Male | 14(37.8) |
| Female | 23(62.2) |
| Ethnicity, n (%) | |
| Hispanic or Latino | 2(5.4) |
| Not Hispanic or Latino | 29(78.4) |
| No answer | 6(16.2) |
| Race, n (%) | |
| American Indian or Alaskan Native | 0 |
| Asian | 6(16.2) |
| Black or African American | 2(5.4) |
| Caucasian | 26(70.3) |
| Other | 1(2.7) |
| No answer | 2(5.4) |
Table 1: Participant characteristics.
Common ELMM-assessed eating rate ranges, as measured in SBB, included measurements between 13-43 SBB, with some more extreme values falling as fast as 10 and as slow as 52 average SBB. Results for the primary outcome of ELMM-assessed eating rate (in SBB) are presented in Figure 1. ELMM-assessed eating rate according to the three SRER groups were: slow=25.5 ± 4.3, medium=21.0 ± 3.4, and fast=20.8 ± 3.0 (mean ± SD) seconds between bites. There was a significant difference among SRER groups (F2,20=4.1, p=0.03, partial η2 = 0.22). Post-hoc Tukey tests showed that participants in the fast SRER group had a significantly lower SBB (indicating fewer SBB thus faster eating rate) than those in the slow SRER group (p=0.03). Participants in the medium SRER group had a significantly lower SBB than those in the slow SRER group (p=0.04), but there was no significant difference in SBB between medium and fast SRER groups (p=0.98). Spearman’s correlations showed no significant association between ELMM-assessed eating rate and SRER (r=-0.28, p=0.12).
One-way ANOVA examined group differences in free-living ELMM-assessed eating rate in seconds between bites (SBB). Higher numbers in SBB denote slower eating rates, while lower numbers show faster eating rates. Post hoc Tukey tests show differences between each SRER category. a= p<0.05: Very slow/slow compared to Medium; b= p<0.05: Very slow/slow compared to Fast/very fast.
For analyses of in-laboratory eating rate as measured by the UEM, the calculation of eating rate was performed using both grams of food consumed per minute, as well as kcalories consumed per minute. Higher numbers indicate faster eating rates, as there are more grams or kcalories being consumed per minute throughout the meal. (This is the opposite of SBB measurement in ELMM-assessed eating rate.) There were no significant associations between free-living eating rate, as assessed by the ELMM, and laboratory measured eating rate on the UEM in grams per minute (r= -0.30, p= 0.09) or in kcalories per minute (r= -0.28, p= 0.12). Table 2 shows tertiary outcome results for UEM-measured eating rate in grams per minute and kcalories per minute by SRER category. There were no significant differences in laboratory-measured eating rate among SRER categories as measured by the UEM in grams per minute (F2,34=1.35, p=0.27), or in kcalories per minute (F2,33=1.05, p=0.36); however, the numbers increased consistently from lower to higher from the slow category to the fast category, and a medium effect size was seen in both (partial η2= 0.07 and 0.06 for grams/minute and kcalories/minute, respectively). No significant associations were found between UEM-measured eating rate in grams/minute and SRER (r = 0.26, p = 0.12).
| SRER Category | N | UEM measured eating rate in grams/minute (Mean ± SD) | p value | Eta squared | UEM measured eating rate in kcals/minute (Mean ± SD) | p value | Eta squared |
|---|---|---|---|---|---|---|---|
| Very slow/slow | 5 | 23.9 ± 13.9 | 0.27 | 0.07 | 40.0 ± 23.1 | 0.36 | 0.06 |
| Medium | 15 | 31.6 ± 16.1 | 53.3 ± 27.0 | ||||
| Fast/very fast | 16 | 36.8 ± 16.4 | 59.3 ± 26.3 |
One-way ANOVA examined group differences in Universal Eating Monitor (UEM)-measured eating rate between Self-Reported Eating Rate (SRER) categories. Higher numbers (kcal per minute) denote faster eating rates, while lower numbers show represent slower eating rates.
Table 2: In-laboratory measured eating rate by SRER category.
Discussion
Eating rate is a behavior that is positively associated with obesity and energy intake, and may be a changeable activity that can lead to reduced energy intake. This study is the first to investigate a device that is capable of assessing eating rate in free-living settings, which has the potential lay the groundwork to move forward the research in this area. In 37 participants with overweight and obesity, the ELMM provided SBB information as a proxy to eating rate measurement over three days of free-living eating occasions. Free-living eating rate assessed as SBB by the ELMM corresponded with the three SRER categories of participants in our study, with a significant difference in SBB among eating rate categories.
The existing need for an objective measure of free-living eating rate was highlighted by the findings on SRER of individual meals from a study by Petty and colleagues, who found no differences among SRER categories in free-living meals [16]. To our knowledge, this was the only study previously attempting validation of free-living eating rate against SRER. In that study, information was collected from three free-living meals by self-reported start and stop times of meals from a oneday food record. Dietary recall has historically been regarded as a suboptimal means of obtaining information about consumption due to inaccuracy [21-23]. A lack of accuracy in reporting meal duration may further compound this inaccuracy, and differences between fast and slow eaters in self-reported eating rate from free-living meals may go undetected [16]. Thus, the ability of the ELMM to tangibly reflect free-living eating rate is an important first step toward more a more objective measure of free-living eating rate.
In the current study, a significant difference was found in ELMM-assessed free-living eating rate between slow and medium eaters, and between slow and fast eaters, but there was no significant difference between medium and fast eaters. This may be because participants had a BMI within the 27-40 kg/m2, most of whom self-reported as medium or fast eaters, which is consistent with the literature demonstrating the positive association between faster eating rates and BMI [7,15]. Additionally, because the ELMM detects bites in six-second intervals [18], bites that take place in shorter intervals may be missed.
Secondary outcomes in the present study included examining relationships between ELMM-assessed and UEM-measured eating rate, and no significant associations were found. While the UEM is a valid tool to measure in-laboratory eating rate due to good test-retest reliability [20], we compared in-laboratory eating rate with free-living eating rate as measured by the ELMM. These two types of eating occasions differ. The lab-measured eating rate by UEM was done under standardized laboratory conditions, which differs from real-world eating conditions. Moreover, the UEM measures food disappearance in grams or kcalories, but the ELMM does not because it is not able to detect bite size. Instead, it measures duration of pauses between bites, reflecting one unique aspect of slow eating. Additionally, the UEM-measured eating rate was based on one meal only, and the meal was pre-selected for the participants. In comparison, the present study examined ELMM-assessed eating rate by using three days of eating occasions from free-living settings, in which participants self-selected their own foods, and it has been established in the laboratory setting that different foods are consumed at different eating rates [24-26]. These differences may account for the lack of significant correlation between the two different types of measures.
Tertiary outcomes of the present study showed no significant differences in SRER categories between the UEM-measured laboratory eating rate of participants with overweight and obesity. A medium effect size was seen (univariate eta squared = 0.07); therefore with additional participants we may have seen statistical significance. Two previous studies validated laboratory measured eating rate against SRER. Petty and colleagues demonstrated that eating rate as measured in the laboratory, using the UEM, aligned with SRER in a study with 60 healthy weight participants, who were selected by study design to measure eating rate across eating rate category groups [16]. To this end, that research group selected approximately 20 participants per group from an online survey from a larger study, and found significant differences in UEM-measured eating rate among SRER categories. Our study did not show significant differences, perhaps related in part to an uneven group distribution, as this was a secondary data analysis. Future studies may consider a larger number of participants and stratifying them according to eating rate category, to establish an even distribution among eating rate categories. The meal offered in the present study was a breakfast meal after a 10 h fast, compared to a pasta-based lunch after a 4 h fast following a standardized breakfast at home in the Petty and colleagues study [16]. Finally, the present study recruited individuals with overweight and obesity while Petty and colleagues studied healthy weight individuals. Therefore, lack of an adequate number of participants in each group and differences in meal type, timing and conditions, and in participants’ BMI, may have contributed to differences in results.
Van den Boer and colleagues also compared SRER and laboratory-measured eating rate in 57 adults [15]. In that study, participants self-reported their eating rate, and eating rate was measured by UEM for three food products (soft bun with cheese, apple, and vanilla custard). Laboratory-measured eating rate increased proportionately and significantly (all p<0.01) with SRER for all three food products measured, and self-reported fast eaters had a significantly higher eating rate compared to self-reported slow and average speed eaters, but no significant differences were found in eating rate between slow and average speed eaters. Therefore, SRER was positively associated with measured laboratory eating rate. However, those participants were younger (mean age, 22.6 ± 2.8 years) with healthy weight (mean BMI, 22.1 ± 2.8 kg/m2) whereas present study participants were older (mean age, 36.5 ± 16.1 years) with overweight or obesity (mean BMI, 31.2 ± 3.5 kg/m2). Thus, the present study was the first to attempt comparisons of SRER in participants with overweight and obesity, and we saw a medium effect size in our analyses. A larger sample might be beneficial to support the findings for this outcome in the future.
Strengths of this study included the ability of the researchers to review recorded data sheets sent via email from participants who downloaded these data using the software that accompanies the device. We examined free-living eating rate using the first available wearable device capable of such assessment. Limitations include the widely Caucasian sample, which may make it difficult to generalize to other populations. However, our sample encompassed a wide range of ages from 18-60, which makes the findings more generalizable to different adult age groups. This study recruited participants with overweight and obesity, and further validation of the ELMM as an appropriate and accurate tool to measure free-living eating rate should be conducted in other populations including those in the healthy BMI range. However, it is within populations with overweight and obesity that eating rate research is most needed.
Fast eating rates have been shown to affect obesity, glucose intolerance, and undesirable adipose distribution [3,4,9,10], as well as energy intake [12-14]. Eating rate as a changeable behavior may inform future programs that address energy intake reduction and weight management strategies. Finding new ways to measure eating rate in free-living settings is an important step in weight management
Conclusion
The results from this study provide the first efforts in examining free-living eating rate as assessed by the ELMM as average SBB during eating occasions, and found that SBB corresponded to SRER. This is an important first step in assessing this tool’s ability to provide information about eating rate in free-living settings, which lays groundwork for future research addressing eating rate as a changeable behavior for weight management. Future studies should consider recruiting larger, equal size samples within each eating rate category for analysis of SBB and its comparison to SRER, as well as assessing eating rate with the ELMM in other, more diverse populations.
Funding sources
This work was supported by a grant awarded by The Obesity Society. The funders had no role in study design, collection, analysis or interpretation of the data, writing the manuscript, or the decision to submit the paper for publication.
Contributors
K Melanson, G Greene and J Beatty were responsible for study design. K Melanson and G Greene proofread the manuscript and provided valuable feedback. J Beatty supervised the collection of data, analyzed the data, and wrote the manuscript.
Conflict of Interest
All authors declare that there are no conflicts of interest.
Acknowledgment
The authors wish to thank the undergraduate students in the Energy Balance Laboratory for their assistance in data collection and entry.
References
- Ng M, Fleming T, Robinson M, Thomson B, Graetz N, et al. (2014) Global, regional, and national prevalence of overweight and obesity in children and adults during 1980-2013: a systematic analysis for the Global Burden of Disease Study 2013. Lancet 384: 766-81
- Flegal K, Kruszon-Moran D, Carroll M, Fryar C, Ogden C, et al. (2016) Trends in Obesity Among Adults in the United States, 2005 to 2014. JAMA 315: 2284-91.
- Ohkuma T, Hirakawa Y, Nakamura U, Kiyohara Y, Kitazono T, et al. (2015) Association between eating rate and obesity: a systematic review and meta-analysis. Int J Obesity 39: 1589-96.
- Otsuka R, Tamakoshi K, Yatsuya H, Murata C, Sekiya A, et al. (2006) Eating fast leads to obesity: findings based on self-administered questionnaires among middle-aged Japanese men and women. J Epidemiol 16: 117-24
- Gerace T, George V (1996) Predictors of weight increases over 7 years in fire fighters and paramedics. Prev Med 25: 593-600
- Tanihara S, Imatoh T, Miyazaki M, Babazono A, Momose Y, et al. (2011) Retrospective longitudinal study on the relationship between 8-year weight change and current eating speed. Appetite 57: 179-83
- Sasaki S, Katagiri A, Tsuji T, Shimoda T, Amano K, et al. (2003) Self-reported rate of eating correlates with body mass index in 18-y-old Japanese women. Int J Obes Relat Metab Disord 27: 1405-10
- Kral J, Buckley M, Kissileff H, Schaffner F (2001) Metabolic correlates of eating behavior in severe obesity. Int J Obes Relat Metab Disord 25: 258-64
- Yaguchi-Tanaka Y, Kawagoshi Y, Sasaki S, Fukao A (2013) Cross-sectional study of possible association between rapid eating and high body fat rates among female Japanese college students. J Nutr Sci Vitaminol 59: 243-9
- Otsuka R, Tamakoshi K, Yatsuya H, Wada K, Matsushita K, et al. (2008) Eating fast leads to insulin resistance: findings in middle-aged Japanese men and women. Prev Med 46: 154-9.
- Zeng X, Cai L, Ma J, Ma Y, Jing J, et al. (2018) Eating fast is positively associated with general and abdominal obesity among Chinese children: A national survey. Sci Rep 8: 14362.
- Shah M, Copeland J, Dart L, Adams-Huet B, James A, et al. (2014) Slower eating speed lowers energy intake in normal-weight but not overweight/obese subjects. J Acad Nutr Diet 114: 393-402
- Andrade A, Greene G, Melanson K (2008) Eating slowly led to decreases in energy intake within meals in healthy women. J Am Diet Assoc 108: 1186-91.
- Robinson E, Almiron-Roig E, Rutters F, de Graaf C, Forde C, et al. (2014) A systematic review and meta-analysis examining the effect of eating rate on energy intake and hunger. Am J Clin Nutr 100: 123-51.
- van den Boer JK, van de Wiel A, Feskens E, Geelen A, Mars M, et al. (2017) Self-reported eating rate is associated with weight status in a Dutch population: a validation study and a cross-sectional study. Int J Behav Nutr Phy 14: 1-11.
- Petty A, Melanson K, Greene G (2013) Self-reported eating rate aligns with laboratory measured eating rate but not with free-living meals. Appetite 63: 36-41.
- Dong Y, Hoover A, Scisco J, Muth E (2012) A New Method for Measuring Meal Intake in Humans via Automated Wrist Motion Tracking. Appl Psychophys Biof 37: 205-15
- Yiru S, Salley J, Muth E, Hoover A (2017) Assessing the Accuracy of a Wrist Motion Tracking Method for Counting Bites Across Demographic and Food Variables. IEEE J Biomed Health Inform 21: 599-606.
- Scisco J, Muth E, Hoover A (2014) Examining the Utility of a Bite-Count-Based Measure of Eating Activity in Free-Living Human Beings. J Acad Nutr Diet 114: 464-9
- Hubel R, Laessle R, Lehrke S, Jass J (2006) Laboratory measurement of cumulative food intake in humans: results on reliability. Appetite 46: 57-62.
- Roberto C, Larsen P, Agnew H, Baik J, Brownell K, et al. (2010) Evaluating the impact of menu labeling on food choices and intake. Am J Public Health 100: 312-8.
- Jonnalagadda S, Mitchell D, Smiciklas-Wright H, Meaker K, Van Heel N, et al. (2000) Accuracy of energy intake data estimated by a multiple-pass, 24-hour dietary recall technique. J Am Diet Assoc 100: 303-8.
- Ma Y, Olendzki B, Pagoto S, Hurley T, Magner R, et al. (2009) Number of 24-hour diet recalls needed to estimate energy intake. Ann Epidemiol 19: 553-9.
- Bolhuis D, Forde C, Cheng Y, Xu H, Martin N, et al. (2014) Slow food: sustained impact of harder foods on the reduction in energy intake over the course of the day. PLoS One 9: e93370
- van den Boer J, Werts M, Siebelink E, de Graaf C, Mars M, et al. (2017) The Availability of Slow and Fast Calories in the Dutch Diet: The Current Situation and Opportunities for Interventions. Foods 6: 87.
- Viskaal-van Dongen M, Kok F, de Graaf C (2011) Eating rate of commonly consumed foods promotes food and energy intake. Appetite 56: 25-31.
Citation: Beatty J, Greene G, Melanson K (2018) A Wearable Device Provides an Alternate Measurement of Free-Living Eating Rate. J Nutr Diet 1:105.
Copyright: © 2018 Beatty J, et al. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.
Share This Article
Open Access Journals
Article Usage
- Total views: 3401
- [From(publication date): 0-2018 - Apr 04, 2025]
- Breakdown by view type
- HTML page views: 2543
- PDF downloads: 858