A Twelve Months Follow-Up: Influence Of Origin and Duration of Hearing-Loss on Tnrts after Cochlear Implantation
Received: 04-Jul-2016 / Accepted Date: 24-Aug-2016 / Published Date: 31-Aug-2016 DOI: 10.4172/2161-119X.1000258
Abstract
Introduction: People with profound sensorineural hearing loss benefit from cochlear implantation. Nevertheless there are discrepancies as far as signal processing and hearing results are concerned. The large variety of patients in terms of age, cause and duration of deafness is one explanation. Neural response telemetry (tNRT) gives information about the function of the hearing nerve and the device. Previous studies couldn`t exactly show evident correlations between NRTs and cause or length of hearing-loss. Aim of the present study was the re-evaluation of tNRTs in a 12 months follow-up as a function of duration and reason of deafness. Patients and methods: 168 patients (82 female, 86 male) implanted at the department between 2008 and 2013 with an implant of Cochlear® were included into the study. 71 patients received a CI512 and 52 patients a CI24RE device, while 45 patients were supplied with the slim straight electrode array CI422. tNRTs were measured at each of the 22 electrodes intraoperatively, after 6 and after 12 months. Results: tNRT-values showed a reduction of tNRT-values over parts of the monitored period. Patients with Menière`s disease showed slightly higher values but the differences regarding the cause of deafness weren`t significant. Implant recipients with a mean time of hearing loss or a mean time of hearing aid supply showed a tendency of lower tNRTs. However the results weren’t significant. Conclusion: Within the first six months after CI implantation tNRTs decreased significantly. Patients with Menière's disease showed decent higher tNRTs. Patients with a period of deafness longer than two years presented lower tNRT thresholds. Participants with a mean time hearing aid supply prior CI surgery also provided a trend towards lower tNRTs. The impact of tNRTs on residual hearing in dependence of different shaped electrode arrays as well as the effect on speech perception should be focused in upcoming studies.
Keywords: Cochlea implant; NRT; ECAP; Hearing loss; Electrode; Deafness; Hearing aid
252743Introduction
People with severe to profound sensorineural hearing loss benefit from cochlear implantation [1,2] Nevertheless there are meanderings with regard to diverse age groups: Younger patients tend to have better hearing results than the older ones [3,4]. The large variety of patients in terms of cause and duration of deafness could be another explanation for the different hearing outcomes. The predictability of hearing success after cochlear implantation at a certain point of time is one of the most often discussed questions. As a matter of course the patient asks for the likeliness of a good hearing result after surgery. Electric compound action potentials (ECAPs) are an objective indicator for the nerve- and device- function and are determined for each of the 22 electrodes on both the slim straight (CI 422) and the precurved (CI24 RE and CI 512) arrays. Having been utilized for more than 20 years now, the importance for the clinical use is still in focus of applied research and application feasibilities in further development [5,6].
ECAPs are potentials from the hearing nerve after stimulation from a CI-electrode and correspond to wave I of the ABR. The stimulation occurs at one electrode and the answering potential gets recorded at the after next electrode. Thus stimulation artefacts can be avoided. A logical theory is that lower values are expected to result in better hearing abilities, because the nerve-reaction already occurs at a minor stimulation level. Intra- and postoperative measurements of ECAPs and determination of the threshold level are very important for a successful supply with cochlear implants and are already part of the daily routine [7]. Intraoperative ECAPs confirm the CI- function and record the hearing nerves answer to direct stimulation. Postoperative ECAPs are additionally important for the very first CI - fitting process as well as in the following controls [7].
ECAPs can be measured by using the NRT-System (Neural Response Telemetry). They are detected visually by marking the first potential that appears after the lowest stimulation level (vNRT). The more common method is to measure several potentials at different stimulation levels and calculate a regression value (tNRT) [8]. However there are even more options to obtain NRTs: In the fitting process of the cochlear implant MAPs (mapping) can be used to optimize the patient`s hearing result: A T-Level (behavioral threshold) demonstrates the threshold at which a sound can be recognized and a C-Level (comfort level) distinguishes a comfortable volume [8]. Though it is not recommended to use NRTs for programming only [9]. It is known that NRTs decrease after surgery [10] and even in case of intraoperative absence NRTs can appear and/or increase with a latency of some months [11]. Literature provides contrary opinions to what extent there is an effect of the patient’s age [3,4,12]. Previous studies couldn`t exactly show evident correlations between NRTs and cause or length of hearing-loss either [2,13]. King et al. analyzed for 21 patients that NRT-thresholds and the slope of the NRT growth function are predictors for the C-Level in patients with a hearing loss less than 20 years [14]. Nevertheless for a larger collective there is no comprehensive knowledge about other parameters influencing NRT values. A further question is if there is a change of these factors in the course of time. Aim of the present study was the evaluation of tNRTs of 168 individuals in a 12 months follow-up as a function of duration and reason of deafness.
Patients and Methods
168 patients (82 female, 86 male) implanted at the department between 2008 and 2013 with an implant of Cochlear® were included into the study. 123 were supplied with a perimodiolar electrode-array: 71 patients with a CI512 and 52 patients with a CI24RE. 45 patients received the slim straight CI422. Electrode insertion was performed 44 times via the round window and 124 times via cochleostomy. A retrospective analysis of tNRTs during operation as well as 6 and 12 months after surgery was performed. Patients with incomplete data set of tNRTs were excluded.
After inserting the electrode array into the cochlear NRTs were determined in an open operative site at each of the 22 electrodes automatically by a program of the company. Every electrode shows specific amplitudes after stimulating the nerve with different intensity levels. By detecting the regression value of above-threshold potentials at each electrode the tNRTs are obtained. A profile of the cochlear implant is shown in a chart and gives information of the tNRTs of each electrode (in CL=current level).
Quantity and mean-scores were calculated for all 22 electrodes and both different array-types. The analysis of variance and the Wilcoxon- Test were determined using SPSS-22. Significant results were set for p<0.05. The comprehensive experience of performing more than 1000 cochlear implants at the clinic showed a useful cut for good results at a tNRT<164 CL. This study was performed in accordance with the Declaration of Helsinki and was approved by the local ethics committee.
Results
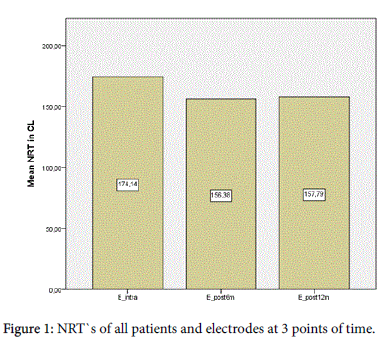
In all age cohorts tNRTs were reproducible intra- and postoperatively. An analysis of all tNRT-values over all patients and each electrode at three points of time revealed a reduction of tNRTvalues over the monitored period. The mean value of the tNRTs improved after 6 months significantly (p=0.000) from 174.14 to 156.38 and despite a slightly following not significant increase (p=0.403) the value remained at this lower standard after 12 months (157.79). Figure 1 shows the mean tNRTs of all patients and electrodes at three points of time.
Origin of hearing loss
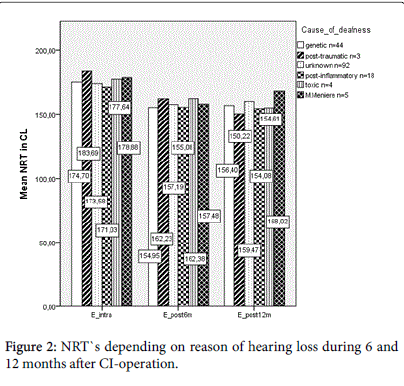
Taking into account the eight main causes of deafness, the largest three groups included the patients with unknown (n=92), genetic (n=44) and post-inflammatory (n=18) reasons of deafness. The genetic group can be subdivided into Connexin26 associated hearing loss (n=5) and other genetic (n=39) reasons. Menières disease (n=5), posttraumatic (n=3) and toxic (n=4) causes were less frequently (Figure 2). In the analysis of variance (ANOVA) of slim straight electrodes the differences between the groups weren`t significant intraoperatively (p=0.806) or after 6 (p=0.757) and 12 (p=0.480) months. Perimodiolar electrodes didn’t show significant results either (p=0.935 and p=0.756 and p=0.453). For statistically reasons the minor cluster of autoimmune (n=1) and otosclerotic (n=1) patients had to be excluded for this calculation.
Duration of hearing loss
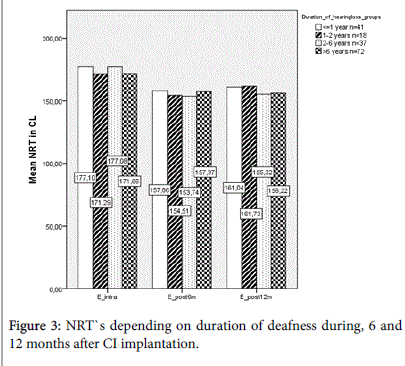
The patients were divided into four groups regarding the time of hearing loss before cochlear implantation (<1 year (n=41), 1-2 years (n=18), 2-6 years (n=37), >6 years (n=72)). The analysis of variance for slim straight electrodes didn`t show significant differences intraoperatively (p=0.555), after 6 (p=0.514) and after 12 months (0.281). Similar results were obtained for the precurved models (p=0.293 und p=0.168 und p=0.195). In the 12 months control decent tendencies of slightly higher tNRT-values were seen in patients with a hearing loss for less than 2 years (Figure 3).
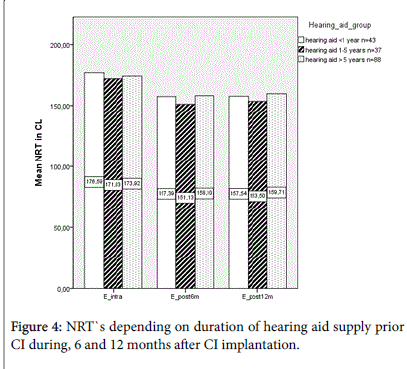
43 CI users had been supplied with a hearing aid for less than one year. While another 37 patients wore a hearing aid 1 to 5 years in advance, 88 participants used a device longer than 5 years prior to CI implantation (Figure 4). The cluster of patients utilizing a hearing aid 1-5 years prior to CI implantation showed slightly lower tNRT values than the others. However there were no significant results intraoperatively (p=0.548), after 6 (p=0.142) and after 12 months (p=0.197) either.
Discussion
Electric compound action potentials (ECAPs) are an indicator for the hearing nerve- and the device- performance in and after CI implantation [7]. A logical theory is that lower values are expected to result in better hearing outcome as the nerve’s reaction occurs to a lower stimulation level. In the course of observed time there are changes of the tNRTs depending on different factors. Mittmann et al. for example discussed the influence of the electrode array’s position inside the cochlea by using a NRT-ratio and proved a high correlation to the results of a radiological control [15]. The impact of further parameters and the possibility of exerting influence on ECAP performance are discussed separately in the following:
NRT in the course of time
Contour advanced electrode arrays are known to result in lower thresholds compared to the slim straight types [10]. However in the present investigation both showed similar characteristics regarding different items: A significant drop of tNRTs could be revealed after 6 months. Chen et al. though showed a significant decrease of tNRTs already after 24 h caused by an almost immediate restoration of neuronal sensitivity and interaction between matrix and electrodes [16]. It is possible that the CI-users of the investigated cohort would have shown the same phenomenon if they were reevaluated at an earlier point of time after implantation than after 6 months. Experience shows that tNRTs as well as the impedances are lower in closed operative settings than determined in an open operative site. Chen et al. didn`t specify the exact measuring circumstances. That might be an explanation for the origin of the rapid NRT-decrease. In contrast Tanamati et al. claimed in their study, that during the first year no significant changes to ECAPs could be found [17]. Brown et al. supported this thesis and assumed only small changes in the development of ECAPs over a 5 to 6 years observation [18]. However, the present results are not in contrast to these observations, as it could be demonstrated as well, that tNRT values kept stable after the initial drop.
Origin of hearing loss
With regard to the cause of deafness significant correlations to tNRT thresholds couldn’t be shown. The same conclusion was drawn by Kutscher et al. [13] who didn`t see a correlation between the recovery function and etiology of hearing loss. Anyhow the results of the present survey clarified that the cluster of patients with Menière’s disease at all three points of time had higher NRTs than the two largest groups (genetic and unknown origin). Nevertheless the outcome was statistically not significant. The difference was most obvious 1 year after implantation. McRackan et al. also claimed that the hearing outcome of Ménière’s disease patients is worse than in the general CI population [19]. Assuming that lower ECAPs are associated with better hearing results, the thesis of McRackan and co-workers can be supported. However cochlear implantation is still the best option to treat profound hearing-loss in patients with Mèniere`s disease [20]. Miyagawa et al. focused on the genetic causes of deafness and claimed that patients with certain gene mutations show relatively good results. [21] Kraaijenga et al. showed that otosclerosis and meningitis are negative predictors for the hearing outcome [22].
Duration of hearing loss
Nehmè et al. negated an influence of the duration of hearing loss on the ECAP outcome [23]. Their cohort was mainly made up of congenitally deafened patients. The period of deafness corresponded to the age at CI operation and the age at implantation didn`t affect the NRTs. These results were in agreement with the current study which didn`t figure out significant differences concerning the length of deafness either. However it could be clarified that 12 months after surgery there was a tendency of lower tNRT thresholds in patients with a duration of hearing loss longer than two years before implantation. These results can be explained with a presumably lighter hearing loss than after a rapid profound deafness (which normally gets implanted earlier) and more various cohorts in the present study. Nehmè et al. investigated only 34 mainly congenitally deafened patients [23], while in the current study 168 CI users with congenital and acquired hearing loss were included. Zeh et al. added, that even in the period of rehabilitation of cochlea implantation there were no differences with regard to the duration of deafness [2].
Kutscher et al. proclaimed there is no correlation between nerve recovery function and time of hearing aid use prior to CI [13]. Lazard et al. supports the thesis that the hearing aid use has a significant influence on the outcome of the hearing performance [24]. In spite there weren`t significant results in the recent study either decent lower tNRTs for patients who utilized a device 1-5 years before operation could be shown. It can be assumed, that patients with a mean time hearing aid provision have better residual hearing conditions and may more often suffer from a slowly progressive hearing loss. The interest for a cochlear implant develops stealthy in the course of time and this issue is accompanied with lower tNRTs. An explanation for the poorer outcome of the short-term supply (less than one year) could be a rapid more severe hearing loss, that couldn`t be treated satisfactorily with conventional hearing aids. The need for cochlear implantation comes straight away and a more profound hearing loss might have been the reason for higher tNRTs. In contrast, if patients have been suffering from profound hearing loss for many years without benefitting from the hearing device for a long time, a degeneration of the hearing nerve might already have occurred. This phenomenon is also reflected in higher tNRT thresholds. An explanation for Kutscher et al.`s contrary thesis [13] might be the smaller collective (n=50). Furthermore only Nucleus24 devices were included, while in the present study CI 422, CI 512 and CI 24 RE were analyzed. A detailed investigation on this issue is the main emphasis of further upcoming publications.
Conclusion
Within the first six months after CI implantation tNRTs decreased significantly and remained stable in the following course of time. Despite of a small number of patients with Ménière’s disease, this group showed decent higher tNRTs than CI users with other reasons of hearing loss. Patients with a period of deafness longer than two years presented lower tNRT thresholds. Participants with a mean time hearing aid supply prior CI surgery also provided a trend towards lower tNRTs. The impact of tNRTs on residual hearing as well as the effect on speech perception over the course of time will be subject for upcoming studies. Furthermore a current evaluation of the electrode arrays tonotopy and differences between slim straight and contour advanced electrode arrays is in process.
References
- Runge CL, Henion K, Tarima S, Beiter A, Zwolan TA (2016) Clinical Outcomes of the cochlearâ„¢ nucleus(â®) 5 cochlear implant system and smartsoundâ„¢ 2 signal processing.J Am AcadAudiol 27: 425-440.
- Zeh R, Baumann U (2015) [Inpatient rehabilitation of adult CI users: Results in dependency of duration of deafness, CI experience and age].HNO 63: 557-576.
- AlSanosi A, Hassan SM (2014) T he effect of age at cochlear implantation outcomes in Saudi children. Int J PediatrOtorhinolaryngol 78:272-276.
- Beyea JA, McMullen KP, Harris MS, Houston DM, Martin JM, et al. (2016) Cochlear implants in adults: Effects of age and duration of deafness on speech recognition.OtolNeurotol .
- Gordon KA, Ebinger KA, Gilden JE, Shapiro WH (2002) Neural response telemetry in 12- to 24-month-old children.Ann OtolRhinolLaryngolSuppl 189: 42-48.
- Abbas PJ, Brown CJ, Shallop JK, Firszt JB, Hughes ML, et al. (1999) Summary of results using the nucleus CI24M implant to record the electrically evoked compound action potential.Ear Hear 20: 45-59.
- Wesarg T, Arndt S, Aschendorff A, Laszig R, Zirn S (2014) Intraoperative audiological-technical diagnostics during cochlear implant surgery. HNO 62:725-734.
- Potts LG, Skinner MW, Gotter BD, Strube MJ, Brenner CA (2007) Relation between neural response telemetry thresholds, T- and C-levels, and loudness judgments in 12 adult nucleus 24 cochlear implant recipients.Ear Hear 28: 495-511.
- McKay CM, Chandan K, Akhoun I, Siciliano C, Kluk K (2013) Can ECAP measures be used for totally objective programming of cochlear implants?J Assoc Res Otolaryngol 14: 879-890.
- Christov F, Munder P, Berg L, Bagus H, Lang S (2016) ECAP analysis in cochlear implant patients as a function of patient's age and electrode-design. Eur Ann Otorhinolaryngol Head Neck Dis 1:S1-S3.
- Moura AC, Goffi-Gomez MV, Couto MI, Brito R, Tsuji RK, et al. (2014) Longitudinal analysis of the absence of intraoperative neural response telemetry in children using cochlear implants. Int Arch Otorhinolaryngol 18:362-368.
- Carvalho B, Hamerschmidt R, Wiemes G (2015) Intraoperative Neural Response Telemetry and Neural Recovery Function: A Comparative Study between Adults and Children.Int Arch Otorhinolaryngol 19: 10-15.
- Kutscher K, Goffi-Gomez MV, Befi-Lopes DM, Tsuji RK, Bento RF (2010) Cochlear implant: Correlation of nerve function recovery, auditory deprivation and etiology.Pro Fono 22: 473-478.
- King JE, Polak M, Hodges AV, Payne S, Telischi FF (2006) Use of neural response telemetry measures to objectively set the comfort levels in the Nucleus 24 cochlear implant. J Am AcadAudiol 17: 413-431.
- Mittmann P, Todt I, Ernst A, Rademacher G, Mutze S, et al. (2016) Electrophysiological detection of scalar changing perimodiolar cochlear electrode arrays: a long term follow-up study. Eur Arch Otorhinolaryngol.
- Chen JK, Chuang AY, Sprinzl GM, Tung TH, Li LP (2013) Impedance and electrically evoked compound action potential (ECAP) drop within 24 hours after cochlear implantation.PLoS One 8: e71929.
- Tanamati LF, Bevilacqua MC, Costa OA (2009) Longitudinal study of the ecap measured in children with cochlear implants.Braz J Otorhinolaryngol 75: 90-96.
- Brown CJ, Abbas PJ, Etlert CP, O'Brient S, Oleson JJ (2010) Effects of long-term use of a cochlear implant on the electrically evoked compound action potential.J Am AcadAudiol 21: 5-15.
- McRackan TR, Gifford RH, Kahue CN, Dwyer R, Labadie RF, et al. (2014) Cochlear implantation in Ménière's disease patients.OtolNeurotol 35: 421-425.
- Samy RN, Houston L, Scott M, Choo DI, Meinzen-Derr J (2015) Cochlear implantation in patients with Meniere's disease.Cochlear Implants Int 16: 208-212.
- Miyagawa M, Nishio SY, Usami S (2016) A comprehensive study on the etiology of patients receiving cochlear implantation with special emphasis on genetic epidemiology.OtolNeurotol 37: e126-e134.
- Kraaijenga VJ, Smit AL, Stegeman I, Smilde JJ, van Zanten GA, et al. (2015) Factors that influence outcomes in cochlear implantation in adults, based on patient related characteristics - a retrospective study. ClinOtolaryngol.
- Nehmé A, El Zir E, Moukarzel N, Haidar H, Vanpoucke F, et al. (2014) Measures of the electrically evoked compound action potential threshold and slope in HiRes 90K(TM) users.Cochlear Implants Int 15: 53-60.
- Lazard DS, Vincent C, Venail F, Van de Heyning P, Truy E, et al. (2012) Pre-, per- and postoperative factors affecting performance of postlinguistically deaf adults using cochlear implants: A new conceptual model over time. PLoS One 7:e48739.
Citation: Christov F, Munder P, Berg L, Arnold J, Bagus H, et al. (2016) A Twelve Months Follow-Up: Influence Of Origin and Duration of Hearing-Loss on Tnrts after Cochlear Implantation. Otolaryngol (Sunnyvale) 6:258. DOI: 10.4172/2161-119X.1000258
Copyright: © 2016 Christov F, et al. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.
Share This Article
Recommended Journals
Open Access Journals
Article Tools
Article Usage
- Total views: 11923
- [From(publication date): 8-2016 - Apr 04, 2025]
- Breakdown by view type
- HTML page views: 11053
- PDF downloads: 870