Research Article Open Access
A Survey of GPS Regarding Current Knowledge and Post-operative Care of Bariatric Surgical Patients
Adams HL1*, Cairney S1, Allport JA2 and Jaunoo SS1
1Warwickshire Surgical Research Group, UK
2University Hospitals Coventry and Warwickshire NHS Trust, UK
- *Corresponding Author:
- Adams HL
Warwickshire Surgical Research Group
UHCW, Clifford Bridge Road
Coventry, CV2 2DX, 156 Barnhorn Road
Bexhill on Sea, East Sussex, TN39 4QL, UK
Tel: +44 24 7696 40
E-mail: h.l.adams@doctors.org.uk
Received date: April 9, 2015; Accepted date: May 25, 2015; Published date: May 31, 2015
Citation: Adams HL, Cairney S, Allport JA, Jaunoo SS (2015) A Survey of GPS Regarding Current Knowledge and Post-operative Care of Bariatric Surgical Patients. J Gastrointest Dig Syst 5:294. doi:10.4172/2161-069X.1000294
Copyright: © 2015 Adams, et al. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.
Visit for more related articles at Journal of Gastrointestinal & Digestive System
Abstract
Background: National Institute of Clinical Excellence (NICE) estimates that 257,000 people in England could qualify for and undergo bariatric surgery. Less than 9,000 procedures were carried out in 2010-2011. Primary care is the access point to these services for patients and provides critical support afterwards. For the National Health Service (NHS) to meet the increasing demand for bariatric services, primary care involvement is crucial.
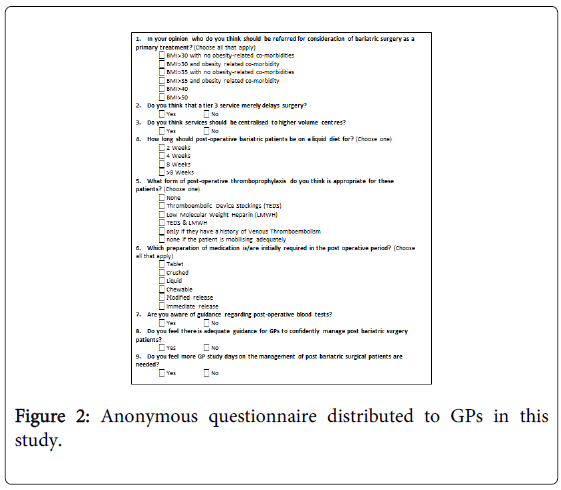
Methods: An anonymous online questionnaire was circulated to General Practitioners (GP) to assess their knowledge of the referral process for bariatric services and post-operative care. GPs throughout the West Midlands, North East, North West and South East of England were invited to answer an electronic questionnaire.
Results: 2417 GPs responded to the questionnaire. 67% thought surgery was appropriate for patients with Body Mass Index (BMI) >35 and related co-morbidities, whereas only 46% thought it appropriate for BMI>50 and lower rates for lower BMIs or the absence of co-morbidities. 49% felt the tiered service delayed surgery while two-thirds supported centralisation of services. 90% of GPs felt ill equipped by current guidelines to manage post-operative patients and only 30% knew of guidelines regarding blood tests. Questions relating to specific post-operative management had a large spread of answers; Liquid diet requirement: 2 weeks 23%, 4 weeks 37%, 8 weeks+ 39%. Appropriate post-operative medication forms: liquid 76%, crushed 34%, chewable 24%, tablet 10%. Free text analysis showed GPs wanted more information about these patients with a preference for detailed discharge summaries, written guidelines and general obesity management study days.
Conclusion: To ensure appropriate patients have access to bariatric services, GPs need further education and guideline dissemination. The majority of GPs felt ill equipped to manage bariatric surgical patients. The importance of detailed plans in discharge letters is clear. GPs would also benefit from post-operative guidelines and overarching obesity study days.
Keywords
Bariatric surgery; Body mass index; Obesity
Introduction
Obesity is rapidly becoming the most important challenge that health services face in the developed world. The prevalence of obesity in over 16 year olds in England has reached 26% in men and 24% in women, for morbid obesity this is 1.6% and 3.9% respectively [1-4]. Lifestyle changes typically produce minimal and short lived results, as do medical interventions [5]. Surgical options have been shown to produce significant, lasting results [6-8]. In 2010/11 less than 9,000 bariatric surgery procedures were performed [2].
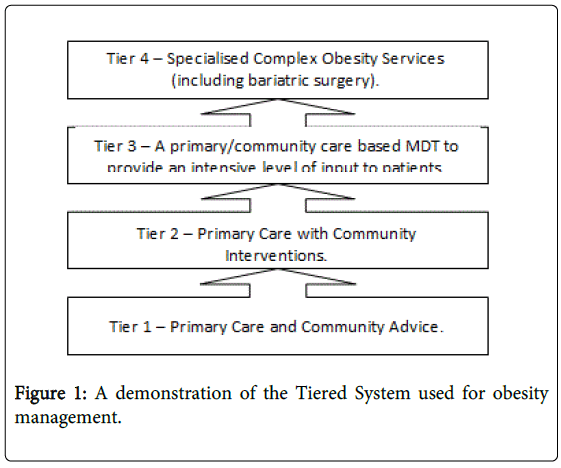
Guidelines have been produced to rationalise obesity management from primary care through to Specialised Complex Obesity Services [2,9]. Obesity is classified based on an individual’s Body Mass Index (BMI), obesity diagnosed at BMI>30 and morbid obesity BMI>40, as shown in Table 1. Obesity services are modelled on a tiered system (Figure 1). Tiers 1-3 offered in the community with varying levels of input from the bariatric Multi-Disciplinary Team (MDT) and Tier 4 the Specialised Complex Obesity Services (including bariatric surgery). Treatment is initiated in a stepwise manner.
| BMI ( kg/m2) | Classification |
|---|---|
| <18.5 | Underweight |
| 18.5-24.9 | Normal |
| 25-29.9 | Overweight |
| 30-30.0 | Obese |
| >40 | Morbidly obese |
Table 1: The classification system for body mass index.
Only when an individual has failed to maintain weight loss despite fully engaging with a structured weight loss programme can they be considered for surgery.
Eligibility criteria for bariatric surgery has been developed to optimise risk versus benefit for patients, ensure cost effectiveness for the NHS, whilst not incentivising weight gain to meet the criteria. Patient selection is based on a combination of BMI and co-morbidities which are likely to improve with weight loss [9], shown in Table 2.
| Indications | Requirements |
|---|---|
| 1. A. BMI>40orBMI >35 with obesity related co-morbidities improved with weight lossand | Full engagement with Tier 3 or 4 MDT services for 12-24 months including: |
| Dietary and exercise advice | |
| Exclusion of underlying disease | |
| Assessment and management of co-morbidities | |
| B.Failure of non-surgical treatment for 6 months | Full psychological assessment |
| 2.BMI>50 | Consideration of risk versus benefit |
Table 2: The indications and requirements involved in the selection of patients for bariatric referrals.
Post-operative patients need specific advice regarding diet, medication and thromboprohpylaxis tailored specifically to their care. Follow up by bariatric surgical services should continue for a minimum of 2 years [9-11]. After this, care is transferred to primary care for support and monitoring of nutrition and weight [3].
NICE estimates 0.53% of England’s adult population meet the criteria and would opt for surgical intervention [12]. This equates to 257,000 patients that require complex obesity services with referral and support from primary care.
The aim of this study was to investigate the current understanding of GPs regarding the referral process and post-operative management.
Materials and Methods
GPs in the West Midlands, North East, North West and South East of England were invited to complete an anonymous online Questionnaire, Figure 2. There were no incentives provided for response and no reminders sent. Only fully completed questionnaires were included in the analysis. Simple descriptive statistics were used to analyse categorical data. Thematic analysis was used for free text responses (Questions 3, 8, and 9).
Results
A total of 2417 questionnaires were submitted and eligible for inclusion in this study.
Referral for surgery as primary treatment was most frequently considered (67%) for patients with BMI>35 and an obesity related co-morbidity, the rate was 13% for a BMI>30 with an obesity related co-morbidity. In the absence of co-morbidities primary surgical referral rates were thought to be as follows; 1% for BMI>30, 15% for BMI>35 and 47% for BMI>40 or >50. Free text answers from other questions reported that a number of GPs had negative opinions of bariatric surgery and felt that “surgery is not the answer”.
GPs were split as to whether the tiered system merely delays surgery with 49% reporting that it did. Centralisation of services was supported by 60% of respondents. Free text responses revealed that while GPs felt that centralisation could improve surgical outcomes, they were concerned that localised services would be lost, thus losing an important input for follow up of patients.
Responses regarding post-operative management were widely varied. There was no consensus on duration for which a liquid diet is required, with 23% opting for 2 weeks, 37% 4 weeks, 29% 8 weeks and 10%>8 weeks. The majority of GPs thought patients would need both Low Molecular Weight Heparin (LMWH) and Thromboembolic Device (TED) stockings post-operatively, however 13% felt neither were necessary and 7% thought they were only needed if there was a history of Venous Thromboembolism (VTE). Liquid medication was most frequently chosen post-operatively (76%), crushed (34%) and chewable (24%) were also common. Immediate release medication was deemed necessary by 9% of respondents.
Whilst 70% of GPs were not aware of any guidance about post-operative blood tests, 90% felt there was insufficient guidance for them to confidently manage these patients. Thematic analysis showed two-thirds of respondents thought sufficient guidance should be encompassed in the discharge letter and adapted for individual patient management, whilst the remaining one-third felt they should not be looking after these patients who require specialist follow up.
GP study days providing management of bariatric surgical patients were supported by 66% of respondents. The free text responses showed that GPs opposing the idea of study days did so because they felt this follow up was “not their job” (1/3), that electronic information (discharge letters and guidance) was sufficient (1/3) and that study days were limited and bariatric surgery was not common enough to warrant tutorials. GPs in favour of study days reported a lack of availability and 82% suggested a half day covering post-operative management or encompassing it within a full day focussed on general obesity management.
Discussion
Bariatric surgery has been shown to be a safe and effective treatment for obesity [6,7,12]. However guidelines currently recommend it should be the primary treatment choice when BMI>50. This was identified by almost half of respondents as being appropriate for primary referral. Responses showed that GPs thought both the level of obesity and related co-morbidities were relevant for referral, with the patient most likely to be considered appropriate for surgery if BMI>35 and co-morbidities. With an estimated 257,000 patients appropriate for bariatric surgery [1] it is important that GPs can identify these cases to ensure appropriate access to services. However knowledge is not the only barrier, with some GPs expressing negative opinions of bariatric surgery influencing their referral to Tier 3 or 4 services.
GPs were split between the delaying effects of the tiered system. It is designed to provide adequate support throughout the process for patients and to make sure they are fully engaged to reap maximum benefit from surgery. Some comments from GPs acknowledged the need for thorough preparation and counselling of these patients before surgery.
Centralisation of bariatric services has been shown to benefit bariatric services. International Federation for the Surgery of Obesity and Metabolic Disorders (IFSO) has stated there needs to be a minimum volume of cases for both hospitals and surgeons involved, there is clear data demonstrating improved outcomes [11]. Larger centres can provide a structured team to allow 24 hour cover and advice. Two thirds of GPs supported centralisation for these reasons, concerns were expressed about the accessibility of these centres for patients who may find it difficult to travel. Indeed as bariatric services increase from the 9,000 cases in 2010/11 the opportunity to increase the number of centres whilst not reducing individual volumes may be of benefit.
Responses to the questions regarding post-operative management were quite varied. This is explained by the concerning 90% of GPs who felt ill equipped to manage post-operative bariatric patients and 60% unaware of any guidelines regarding blood tests. Guidance suggests there should be specialist surgical input for two years post procedure, after this, care can be wholly transferred to the GP. This lack of knowledge was evident by the wide range of responses given about the specifics of post-operative care. A number of GPs noted that their answers were indeed guesses, based on no knowledge or evidence. British Obesity and Metabolic Surgery Society (BOMSS) has recently developed guidelines regarding post-operative biochemical monitoring [13,14]. NICE has also recently updated guidelines for bariatric surgery referrals and type 2 diabetes mellitus [9].
In the free text answers many themes were evident. Some GPs felt that this was such a rare topic that it was of minimal importance, only 2 respondents acknowledged that this specialty is set to increase. Many respondents flagged the importance of ongoing involvement of specialist centres and indeed questioned the necessity for the involvement of primary care. Further education and guidance was popular. Detailed discharge summaries were the most frequently suggested route to provide post-operative guidance and are indeed the recommended method to shared care plans [15]. Dissemination of written referral and post-operative guidelines were also popular along with study days relating to general obesity management. A number of GPs were keen for access to specialist services for ongoing advice when required.
The only research previously tackling this topic showed very similar results. Of 230 respondents from Scotland, 30% did not know of referral guidelines and 76% were not comfortable managing these patients [16].
Conclusions
GPs have crucial roles in the provision of bariatric services. They are gatekeepers to higher levels of care and are essential in ongoing monitoring and support to this growing population of patients. Further education of GPs is crucial so they are able to fulfil this role safely and effectively. Further work is also needed from Tier 3 and 4 bariatric services to engage with Primary Care to ensure GPs do not feel they are having to manage an extra workload without help and advice. This will help to ensure bariatric services remain as valuable as they currently are.
References
- (2007) National Institute for Health and Care Excellence (NICE). Bariatric surgical service for the treatment of people with severe obesity pp. 1-26.
- (2013) NHS Commissioning Board. NHS Commissioning Board Clinical Commissioning Policy?: Complex and Specialised Obesity Surgery pp. 2-18.
- Jagadesham VP, Sloan M, Ackroyd R (2014) Bariatric surgery: implications for primary care. BJGP 64: 384-385.
- Moody A (2013) Adult anthropometric measures, overweight and obesity. Chapter 10 in: Craig R, Mindell J, editors. Health Survey for England 2012: Health, social care and lifestyles. Leeds: Health and Social Care Information Centrepp. 1-39.
- (2000) National Heart Lung and Blood Institute. The Practical Guide. Identification, Evaluation, and Treatment of Overweight and Obesity in Adults pp. 26-27.
- Christou N V, Sampalis JS, Liberman M, Look D, Auger S, et al. (2004) Surgery decreases long-term mortality, morbidity, and health care use in morbidly obese patients. Ann Surg. 240: 416-423, discussion pp. 423-424.
- Colquitt JL, Picot J, Loveman E, Clegg AJ (2009). Surgery for obesity. Cochrane Database of Systematic Reviews.
- Buchwald H (2012) A Bariatric Surgery Algorithm. Obesty Surg. 12: 733-746.
- (2014) National Institute for Health and Care Excellence (NICE). CG189: Obesity: identification, assessment and management of overweight and obesity in children, young people and adults. National Institute for Health and Care Excellence, Clinical Guideline 189.
- (2012) BOMSS Service Standards & Commissioning Guidance Working Party. PROVIDING BARIATRIC SURGERY BOMSS Standards for Clinical Services & Guidance on Commissioning pp. 1-16.
- Fried M, Yumuk V, Oppert JM, Scopinaro N, Torres A, et al. (2014) Interdisciplinary European guidelines on metabolic and bariatric surgery. ObesSurg24: 42-55.
- Sjostrom L, Narbro K, Sjostrom CD, Karason K, Larsson B, et al. (2007) Effects of bariatric surgery on mortality in Swedish obese subjects. N Engl J Med. 357: 741-752.
- O’Kane M, Pinkney J, Aasheim E, Barth J, Batterham R, et al. (2014) BOMSS Guidelines on perioperative and postoperative biochemical monitoring and micronutrient replacement for patients undergoing bariatric surgery pp. 1-27.
- O’Kane M, Pinkney J, Aasheim E, Barth J, BatterhamR,et al. (2014) GP Guidance?: Management of nutrition following bariatric surgery.
- (2012) National Confidential Enquiry Into Patient Outcome and Deaths (NCEPOD). Too Lean a Service?? A review of the care of patients who underwent bariatric surgery.
- Kynaston J, Mitchell A, Bruce D (2012) PMO-050 A survey of GP’s knowledge and attitudes towards bariatric surgery in Scotland. Gut pp. A94–A94.
Relevant Topics
- Constipation
- Digestive Enzymes
- Endoscopy
- Epigastric Pain
- Gall Bladder
- Gastric Cancer
- Gastrointestinal Bleeding
- Gastrointestinal Hormones
- Gastrointestinal Infections
- Gastrointestinal Inflammation
- Gastrointestinal Pathology
- Gastrointestinal Pharmacology
- Gastrointestinal Radiology
- Gastrointestinal Surgery
- Gastrointestinal Tuberculosis
- GIST Sarcoma
- Intestinal Blockage
- Pancreas
- Salivary Glands
- Stomach Bloating
- Stomach Cramps
- Stomach Disorders
- Stomach Ulcer
Recommended Journals
Article Tools
Article Usage
- Total views: 14508
- [From(publication date):
June-2015 - Apr 05, 2025] - Breakdown by view type
- HTML page views : 9994
- PDF downloads : 4514