A study on Morphology of Rupture of Sinus of Valsalva, Clinical Presentation, Surgical Techniques and Postoperative outcome-A single Centre Experience
Received: 19-Feb-2022 / Manuscript No. JCPR-22-54372 / Editor assigned: 21-Feb-2022 / PreQC No. JCPR-22-54372 (PQ) / Reviewed: 07-Mar-2022 / QC No. JCPR-22-54372 / Revised: 12-Mar-2022 / Manuscript No. JCPR-22-54372 (R) / Published Date: 19-Mar-2022 DOI: 10.4172/jcpr.1000159
Abstract
Background: The study was performed to analyze different presentation, type, surgical approach and long term outcome of patients with rupture of sinus of Valsalva.
Methods: We investigated 16 consecutive patients (Mean age: 33.75, Range: 26-65 years) who underwent surgical repair of sinus of valsalva between January 2014 to march 2019.
Results: Mean age of the patients in the study group was 33.75+-13.76.Most of the patients were male (62.5%). Most common presenting features were dyspnea on exertion (81.25%). Right coronary cusp (56.25%) was involved most commonly and right atrium (50%) was the most common communicating cardiac chamber. Most of the patients (75%) had associated aortic regurgitation with varying degree (Mild-12.5%, Moderate-25%, and Severe-37.5%).The surgical approach is mainly through Trans aortic and the chamber involved in all cases for better surgical outcome. Multi valvular heart disease associated with rupture of sinus of valsalva necessitates its repair or replacement results in poor postoperative outcome.
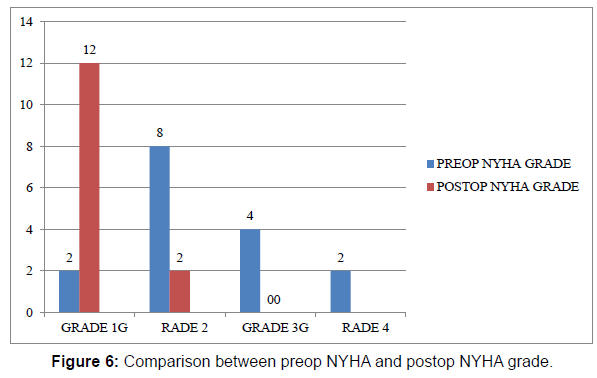
Conclusion: Rupture of sinus of Valsalva is a rare cardiac condition which requires surgical intervention. The long term outcome following surgery is satisfactory with improvement in NYHA clinical status.
Keywords
Sinus; Surgical approach; Cardiac
Abbreviations: 2D- 2 Dimensional; AR- Aortic regurgitation; AVR- Aortic valve replacement; AXC- Aortic cross clamp time; CABG- Coronary artery bypass grafting; CPB- Cardiopulmonary bypass; CT- Computed tomography; ICU- Intensive care unit; LA- Left atrium; LV- Left ventricle; LCC- Left coronary cusp; MR- Mitral regurgitation; MRI-Magnetic resonance imaging; MSCT- Multisite computed tomography; MVR- Mitral valve replacement; NCC- Non coronary cusp; NYHA- New York heart association; RA- Right atrium; RCA- Right coronary artery; RCC- Right coronary cusp; RSOV- Rupture of sinus of valsalva; RV- Right ventricle; RVOT- Right ventricular outflow tract; SAM- Subaortic membrane; SVG- Saphenous vein graft; TR- Tricuspid regurgitation; VIS- Vasoactive inotropic score; VSDVentricular septal defect.
Introduction
Rupture of Sinus of Valsalva (RSOV) is a rare clinical cardiac condition with overall incidence of approximately 0.1% [1]. It may be congenital or acquired and congenital and the incidence of congenital RSOV is approximately 3.5% of congenital heart disease [2]. The postulated hypothesis for the congenital variant is congenital discontinuity of the tunica media between the aorta and annulus fibrosus of the aortic valve which leads to aneurysm formation. Acquired aneurysms may be due to trauma, atherosclerosis, infective endocarditis, syphilis, Marfan syndrome and collagen vascular disorders. Congenital aneurysms are often associated with ventricular septal defect and aortic valve dysfunction, pulmonary stenosis, bicuspid aortic valve, mitral insufficiency with or without prolapse, coarctation of the aorta, patent ductus arteriosus and tricuspid insufficiency [3]. Unruptured sinus of Valsalva aneurysms are seldom diagnosed due to its silent nature with gradual progression. RSOV may present with serious complication like conduction disturbances, coronary artery compression with infarction, endocarditis, right ventricular outflow obstruction and thrombus within the aneurismal cavity [4]. It has a bimodal age of presentation in the first and fourth decade. Most common presenting complication of aneurysm of sinus of Valsalva is rupture of the affected sinus. Most commonly affected sinus is right or non-coronary sinus which commonly communicates to right atrium or right ventricle. It may rarely rupture into left atrium, left ventricle, pericardial cavity or pulmonary artery [5]. It is usually diagnosed with 2D transthoracic and transesophageal echocardiography, multisite computed tomography (MSCT) and MRI but transesophageal echocardiography is the gold standard [6]. This condition necessitates early prioritization in terms of management to prevent morbidity and mortality associated with this disease. The surgical intervention includes simple plication, patch repair, aortic valve replacement/repair and aortic root replacement.
RSOV complicated with infective endocarditis or sepsis carries a high risk of mortality [7].
Material and Method
The primary goal of our study was to analyze clinical presentation, ruptured coronary sinus and the communicating chamber involved in rupture sinus of Valsalva. Consent was taken from every patient as per the institutional ethics committee recommendation. We investigated 16 consecutive patients with a mean age (3.75+13.76) and NYHA functional classification (I-12.5%, II-50%, III-25%, and IV- 12.5%) who underwent surgical repair of rupture of sinus of Valsalva at our institution between January 2014 to March 2019. The most common indication of surgery was dyspnea on exertion (81.25% of the patients). Communication with the respective cardiologist and the patient’s relative guaranteed the highest compliance. 2D transthoracic echocardiography was done in all cases for diagnosis. Additional investigation inform of cardiac CT angiogram was done in two patients in view of diagnostic dilemma. Cardiac catheterization was done in three patients in view of age more than 45 years as per institutional protocol.
All patients underwent median sternotomy with standard Aortobicaval cannulation for cardiopulmonary bypass under normothermia with intermittent cold blood cardioplegic arrest. Fibrillatory arrest was done in six patients for severe aortic regurgitation.Transaortic approach with additional opening of the communicating chamber was done in all patients. All patients underwent patch closure of rupture of sinus of Valsalva and additional procedure was done according to the associated cardiac anomalies.
The secondary outcome was measured in terms of cross clamp time, cardiopulmonary bypass time, associated cardiac lesion necessitates surgery, vasoactive inotropic score, hours of mechanical ventilation, intensive care unit stays and hospital stays after operation.
All patients were followed up for a period of minimum 12 months in terms of improvement of NYHA functional status.
This is a single center retrospective analysis of 16 patients who underwent surgery for rupture of sinus of Valsalva. Baseline data covariable including age, type of presentation, NYHA functional status, surgical approach, cross clamp time, cardiopulmonary time, vasoactive inotropic score, duration of mechanical ventilation, intensive care stays and hospital stays after surgery were summarized as mean and standard deviation. Negative binomial models were assess the baseline data with the other parameters of the study. In case of nonlinear effects of the co-variable predictions were transformed with logarithmic and polynomial functions. All statistical calculations were conducted with standard statistical programs (SPSS 8.01, SPSS, Inc., and Chicago, IL).
Result
The mean age at presentation in this study was 33.75 years with standard deviation of 13.76 years. 62.5% of the patients were male and 37. The most common presenting symptom was dyspnea on exertion (81.25% of patients) followed by palpitation (25% of patients) and angina on exertion (12.5% of patients).Most of the patients presented with NYHA (New York heart association) grade II (50%) (Table 1).
| Parameters | Data |
|---|---|
| Age | Mean-33.375, Standard deviation-13.769 |
| Sex | Male-10 (62.5%).Female-6 (37.5%) |
| Dyspnea on exertion | 14 (81.25% patient) |
| Palpitation | 4 (25% patient) |
| Angina | 8 (12.5% patient) |
| NYHA Class | I-2 (12.5%) II-8 (50%) III-4 (25%) IV-2 (12.5%) |
| Anasarca | 2 (12.5%) |
Table 1: Patient particular and presenting symptom.
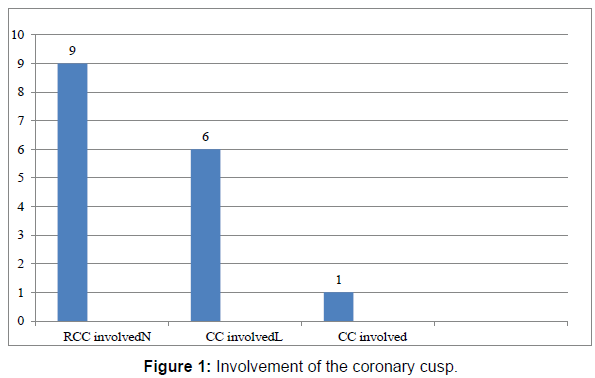
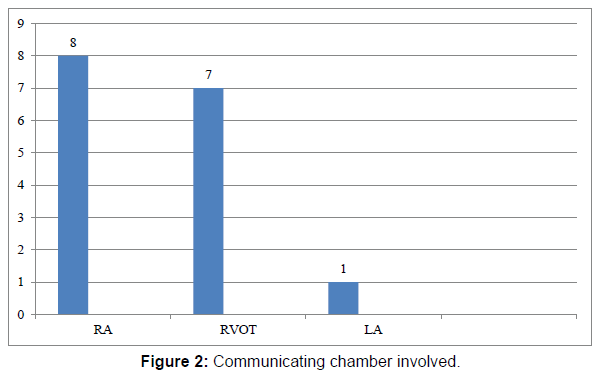
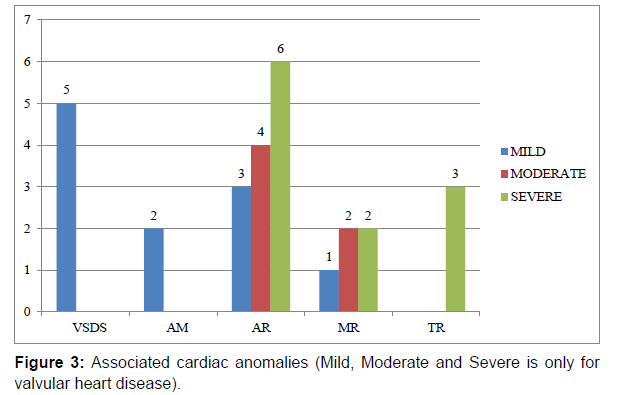
56.25% of the patients had RCC involvement whereas 37.25% and 6.25% of the patients had NCC and LCC involvement respectively. The communicating cardiac chamber was RA in half of the cases whereas RVOT and LA was the communicating chamber in 43.75% and 6.25% of the cases. Mild, moderate severe LV dysfunction was present in 37.5%, 12.5% and 6.25%.Three fourth of the patient had an associated valvular aortic regurgitation and of the patients underwent aortic valve replacement as repair resulted in sub optimal outcome. Other lesions found on echocardiography were VSD (31.25%), SAM (12.5%), Mild MR (6.25%), moderate MR (12.5%), severe MR (12.5%), moderate TR (6.25%) and severe TR (18.75%). Primary pathology of MR was due to rheumatic heart disease. Coronary angiogram was done in 3 patients due to late age of presentation in which 1 patient had distal RCA stenosis necessary venous grafting (Table 2).
| Cusp involved | RCC (right coronary cusp)-9 (56.25%) NCC (non- coronary cusp)-6 (37.5%) LCC (left coronary cusp)-1 (6.25%) |
| Chamber involved | RA (right atrium)-8(50%) RVOT (right ventricular outflow tract)-7 (43.75%) LA (left atrium)-1(6.25%) |
| RV(right ventricle) function | Good-16 (100%) |
| LV(left ventricle) function | Good-7 (43.75%) Mild dysfunction-6 (37.5%) Moderate dysfunction-2 (12.5%) Severe dysfunction-1 (6.25%) |
| Aortic regurgitation(AR) | No-4 (12.5%) Mild-2 (12.5%) Moderate-4 (25%) Severe-6 (37.5%) |
| Other lesion | VSD (ventricular septal defect)-5 (31.25%) SAM (Subaortic membrane)-2 (12.5%) Mild MR (Mitral regurgitation)-1 (6.25%) Moderate MR-2 (12.5%) Severe MR-2 (12.5%) Moderate TR-1 (6.25%) Severe TR (Tricuspid regurgitation)-3 (18.75%) |
Table 2: Echocardiographic features.
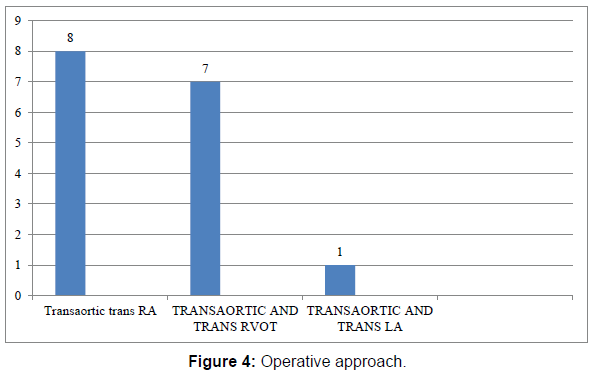
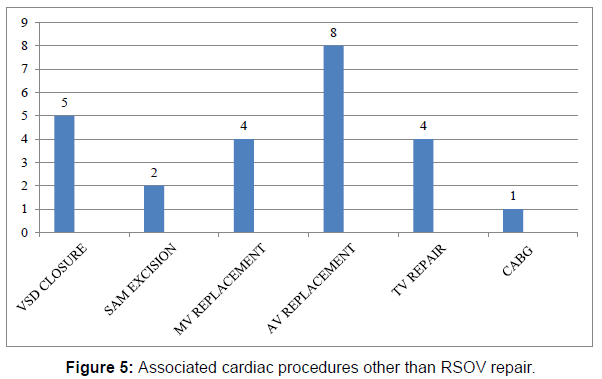
87.5% of the patients underwent elective surgery whereas 12.5% of patients underwent emergency surgery due to heart failure. During operation Transaortic and Trans RA, Transaortic and Trans RVOT, Transaortic and Trans LA approach were used in 50%, 43.75%, and 6.25%. Other procedures done are VSD Closure (31.25%) SAM excision (12.5%) Mitral valve replacement (25%) Aortic valve replacement (43.75%) Tricuspid valve repair (25%) CABG single graft SVG to RCA (6.25%) respectively. Mean AXC and CPB time was 90.93 minutes and 113.66 minutes. Mean VIS score just after operation was 21.5.Mean duration of mechanical ventilation was 12.87 hours. Mean ICU stay and hospital stay were 5.25 days and 8.18 days consecutively. There were two in hospital mortality one is due to recurrent ventricular tachycardia refractory to electromechanical conversion and other was due to persistent postoperative low cardiac output syndrome refractory to management .Both the patient had multi valvular rheumatic heart disease. Mean follow up was 45 months. There were no late death or late intervention during follow up and 85.71% patients were NYHA I 14.29% patients were NYHA II of the surviving individuals (Table 3 and Figures 1-6).
| Surgery type | Emergency-2 (12.5%) Elective-14 (87.5%) |
| Surgical approach | Transaortic and trans RA-8 (50%) Transaortic and trans RVOT-7 (43.75%) Transaortic and trans LA-1 (6.25%) |
| Other procedure | VSD Closure-5 (31.25%) SAM excision-2 (12.5%) Mitral valve replacement-4 (25%) Aortic valve replacement-8 (50%) Tricuspid valve repair-4 (25%) CABG (coronary artery bypass grafting) single graft-1 (6.25%) |
| AXC (aortic cross clamp) Time | Mean-90.93minute, Standard deviation-18.65 minute |
| CPB (cardiopulmonary bypass) Time | Mean-113.56 minute, Standard deviation-23.74 minute |
| VIS score | Mean-21.5, Standard deviation-6 |
| Hours of ventilation | Mean-12.87 Hours, Standard deviation-5.41 Hours |
| ICU Stay | Mean-5.25 days, Standard deviation-3.07days |
| Hospital stay | Mean-8.18 days, Standard deviation-3.87 days |
Table 3: Operative and immediate postoperative features.
Discussion
The clinical condition of acute rupture of congenital sinus of Valsalva was first described in 1839 [8]. In 1956 first successful surgical repairs of sinus of Valsalva aneurysms was performed at the Mayo Clinic and the University of Minnesota [9]. Primary lesion of congenital sinus of Valsalva aneurysms is due to separation of the aortic media of the sinus from the media adjacent to the crux line of the aortic valve cusp which is due to absence of normal aortic elastic tissue and media in this region. The congenitally weak area gradually enlarges under aortic pressure to form an aneurysm [10]. Acquired sinus of Valsalva aneurysms caused by arteriosclerosis, Behcet’s disease, endocarditis, Medionecrosis, penetrating injuries or syphilis are usually readily distinguishable from congenital forms which are more diffuse, involving more part of the sinus or multiple sinuses and often the ascending aorta, and therefore project into the pericardium outside the heart [11]. Localized windsocks are developed from aneurysm which ultimately ruptures into an adjacent low-pressure cardiac chamber but in about one fourth of patients have direct fistulous communication between the aortic sinus and the heart [12]. Most commonly involved cusp is right coronary cusp followed by non-coronary cusp and left coronary cusp is rarely involved [13]. In our study right coronary cusp was most commonly involved cusp followed by non-coronary cusp and left coronary cusp. Most common chamber involved is right atrium followed by right ventricle but rarely may ruptured to left atrium, left ventricle, pulmonary artery, ventricular septum and pericardium [1]. In our study right atrium is commonly involved followed by right ventricle and only in one patient left atrium was involved. The presentation of the lesion depends on the size of the shunt and presence of associated defects. Patient with large shunt and associated lesions presents early due to early development of symptoms. LV volume overload, right ventricular hypertension is present due to shunt and congestive heart failure develops due to increased pulmonary blood flow. Presence of endocarditis also affects symptoms and presentation [14]. Infant to patients of seventh decade can be involved [15]. Presentation is usually common in third decade of life [16]. In our study age range was 22- 65 with mean age 33.75. RSOV is more common in Asia and male are commonly affected [17]. In our study 62.5% of the patients were male. Common presenting symptoms are dyspnea, pain, palpitations, or fatigue [15]. In our study most common presenting symptom is dyspnea on exertion and 37.5% patients presented with heart failure. RSOV is commonly associated with ventricular septal defect, aortic valve abnormality, and pulmonary stenosis, coarctation of aorta, atrial septal defect, patent ductous arteriosus, and Tetralogy of Fallot [18]. Presence of VSD affects in which chamber rupture occurs and coexisting VSD may alter clinical presentation of the patients. In our study VSD is present in 31.25% of patients and sub aortic membrane is present in 12.5% of patients.VSD are commonly sub aortic followed by perimembranous [19]. In our study 60% of VSD are sub aortic and 40% of VSD are perimembranous. However, most published reports indicate that the AV replacement is needed in 20%-30% [15]. Postoperative cardiac function depends on preoperative AR and left ventricular functions [14]. Untreated ruptured aneurysms of the sinus of Valsalva patients die within 1 year most commonly due to heart failure that’s why presence of congestive HF suggests a large shunt and warrants urgent operation [20]. Transthoracic and transesophageal echocardiography, multi detector computed tomography, magnetic resonance imaging, cath angiographies are different modalities to diagnose RSOV but transesophageal echocardiography is gold standard. Tran’s thoracic echocardiography should be done judiciously because VSD may be missed due to RSOV jet [21]. Treatment is surgical excision of the redundant part followed by patch closure of the defect. Commonly elective surgery is done but emergency surgery is indicated in patients with acute detoriation. Repair is done under cardiopulmonary bypass with aortic and bicaval cannulation and aortic and RA cannulation is preferred if chamber involved is RVOT or LA. Normally cardioplegic arrest is done but aortic regurgitation is commonly present so in that case fibrillatory arrest is done. Ante grade cardioplegia followed by ostial cardioplegia is done. There are three main operative approaches: (1) Transaortic- through the aortic root via an aortotomy, (2) Trans RA/LA/RVOT- through the cardiac chamber in which the aneurysm has ruptured, or (3) A dual approach through both an aortotomy and an incision into the involved cardiac chamber. Dual approach is preferred to assess the adequacy of repair and to prevent any iatrogenic injury to the adjacent cardiac tissue during repair. The choice of approach is determined by the presence of aortic valvular pathology such as aortic regurgitation, the size of the lesion, the presence of concomitant cardiac anomaly such as a ventricular septal defect, and the sinus communicating the cardiac chamber. Ruptured sinus can be closed primarily or with patch. Primary closure has been routinely used for the repair of small lesion. Patch closure is preferred for repair of larger lesion, as primary closure in those cases may distort the aortic sinus resulting in aortic valve incompetence, or may cause excessive tissue tension in the repair site resulting in delayed recurrent rupture. Inter ventricular septum should be checked for VSD because it may be missed during echocardiography .Immediate surgical outcome is good and in hospital mortality is less than 5% [22]. In our study mortality is 12.5% as both the patients had multi valvular rheumatic heart disease and required mitral and aortic valve replacement. The presence of VSD, AR, or both cause volume overload along with rupture of SVA. Postoperative LV dysfunction is anticipated with significant volume load either due to acute ruptures leading to HF or the presence of coexisting lesions. Postoperative left ventricular dysfunction is unrelated to the cardiac status of the patient [16]. Heart block may be present in about 2-3% of the patients may land up with heart block of variable degree during immediate postoperative period [1]. The incidence of reoperation is found to be more if direct closure of the ruptured sinus of Valsalva is done over the patch closure [22] Marked left ventricle enlargement with severe AR is a risk factor for premature death in the late postoperative period. Long-term results are excellent if aortic valve replacement is not done [23]. Device closure is also reported for RSOV. Complications of device closure are device migration, residual shunt, new onset AR, RVOT obstruction, impingement on coronary artery and site rupture. The treatment of choice is surgical approach over device closure due to the limited data available in favor of device therapy [24].
Conclusion
RSOV is a rare cardiac disease with varied presentation ranging from asymptomatic to life threatening condition. The individuals need surgical repair as the procedure results in satisfactory outcome. Associated cardiac condition necessitating surgery is a risk factor for poor outcome.
References
- Chu SH, Hung CR, How SS, Chang H, Wang SS, et al. (1990) Ruptured aneurysms of the sinus of Valsalva in Oriental patients. J Thorac Cardiovasc Surg 99: 288-298.
- Post MC, Braam RL, Groenemeijer BE, Nicastia D, Rensing BJ, et al. (2010) Rupture of right coronary sinus of Valsalva aneurysm into right ventricle. Neth Heart J 18: 209-211.
- Choudhary SK, Bhan A, Sharma R, Airan B, Kumar AS, et al. (1997) Sinus of Valsalva aneurysms: 20 years’ experience. J Card Surg 12: 300-308.
- Wang ZJ, Zou CW, Li DC, Li HX, Wang AB, et al. (2007) Surgical repair of sinus of Valsalva aneurysm in Asian patients. Ann Thorac Surg 84: 156‑160.
- Lin CY, Hong GJ, Lee KC, Tsai YT, Tsai TS et al. (2004) Ruptured congenital sinus of valsalva aneurysms. J Card Surg 19: 99-102.
- Shah RP, Ding ZP, Ng AS, Quek SS (2001) A ten-year review of ruptured sinus of valsalva: clinic-pathological and echo-Doppler features. Singapore Med J 42: 473-476.
- Vural KM, Sener E, Taşdemir O, Bayazit K (2001) Approach to sinus of Valsalva aneurysms: a review of 53 cases. Eur J Cardiothorac Surg 20: 71-76.
- Hope J (1839) A treatise of disease of the heart and great vessels (3rd Edn). London: Churchill.
- Bontils-Roberts EA, DuShane JW, McGoon DC, Danielson GK (1971) Aortic sinus fistula: surgical considerations and results of operation. Ann Thorac Surg 12: 492-502.
- Edwards JE, Burchell HB (1956) Specimen exhibiting the essential lesion in aneurysm of the aortic sinus. Proc Staff Meet Mayo Clin 31: 407-412.
- Morris GC Jr, Foster RP, Dunn RJ, Cooley DA (1958) Traumatic aortico–ventricular fistula: report of two cases successfully repaired. Am Surg 24: 883-888.
- Rosenberg H, Williams WG, Trusler GA, Smallhorn J, Rowe RD, et al. (1986) Congenital aortico–right atrial communications: the dilemma of differentiation from coronary cameral fistula. J Thorac Cardiovasc Surg 91: 841-847.
- Killen DA, Wathanacharoen S, Pogson GW Jr (1987) Repair of intrapericardial rupture of left sinus of Valsalva aneurysm. Ann Thorac Surg 44: 310-311.
- Murashita T, Kubota T, Kamikubo Y, Shiiya N, Yasuda K. (2002) Long‑term results of aortic valve regurgitation after repair of ruptured sinus of Valsalva aneurysm. Ann Thorac Surg 73: 1466‑1471.
- Azakie A, David TE, Peniston CM, Rao V, Williams WG (2000) Ruptured sinus of Valsalva aneurysm: Early recurrence and fate of the aortic valve. Ann Thorac Surg 70: 1466‑1470.
- Diwakar A, Patnaik SS, Hiremath CS, Chalam KC, Dash PK (2019) Rupture of Sinus of Valsalva-A 15 Years Single Institutional Retrospective Review: Preoperative Heart Failure has an Impact on Post operative Outcome?. Ann Card Anaesth 22: 24-29.
- Van Son JA, Danielson GK, Schaff HV, Orszulak TA, Edwards WD, et al. (1994) Long-term outcome of surgical repair of ruptured sinus of Valsalva aneurysm. Circulation 90: 1120-1129.
- Au WK, Chiu SW, Mok CK, Lee WT, Cheung D (1998) Repair of ruptured sinus of Valsalva aneurysm: determinants of long-term survival. Ann Thorac Surg 66: 1604.
- Sakakibara S, Konno S (1968) Congenital aneurysm of the sinus of Valsalva associated with ventricular septal defect: anatomical aspects. Am Heart J 75: 595-603.
- Kirklin JW, Barratt‑Boyes BG (2013) Congenital aneurysm of the sinus of Valsalva. In: Cardiac Surgery. (4th edn). New York Churchill Livingstone 1326‑1341.
- Weyman AE, Dillon JC, Feigenbaum H, Chang S (1975) Premature pulmonic valve opening following sinus of Valsalva aneurysm rupture into the right atrium. Circulation 51: 556-560.
- Abe T, Komatsu S (1988) Surgical repair and long-term results in ruptured sinus of Valsalva aneurysm. Ann Thorac Surg 46: 520-525.
- Murashita T, Kubota T, Kamikubo Y, Shiiya N, Yasuda K (2002) Longterm results of aortic valve regurgitation after repair of ruptured sinus of Valsalva aneurysm. Ann Thorac Surg 73:1466-71.
- Weinreich M, Yu P J, Trost B (2015) Sinus of Valsalva Aneurysms: Review of the Literature and an Update on Management. Clin Cardiol 38: 185-189.
Indexed at , Google Scholar , Crossref
Indexed at , Google Scholar , Crossref
Indexed at , Google Scholar , Crossref
Indexed at , Google Scholar , Crossref
Indexed at , Google Scholar , Crossref
Indexed at , Google Scholar , Crossref
Indexed at , Google Scholar , Crossref
Indexed at , Google Scholar , Crossref
Indexed at , Google Scholar , Crossref
Indexed at , Google Scholar , Crossref
Indexed at , Google Scholar , Crossref
Indexed at , Google Scholar , Crossref
Indexed at , Google Scholar , Crossref
Indexed at , Google Scholar , Crossref
Citation: Kumar R, Rawat S, Halder V, Ghosh S, Dutta ARS, et al. (2022) A study on Morphology of Rupture of Sinus of Valsalva, Clinical Presentation, Surgical Techniques and Postoperative outcome-A single Centre Experience. J Card Pulm Rehabi 6: 159. DOI: 10.4172/jcpr.1000159
Copyright: © 2022 Kumar R, et al. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.
Share This Article
Open Access Journals
Article Tools
Article Usage
- Total views: 2535
- [From(publication date): 0-2022 - Mar 31, 2025]
- Breakdown by view type
- HTML page views: 2033
- PDF downloads: 502