Research Article Open Access
A Study on Effectiveness of Ilioinguinal and Iliohypogastricnerve Block at the Time of Wound Closure for Postoperative Pain Relief in Inguinal Hernia Repair
Aye Thandar Htun*
Universiti Sultan Zainal Abidin, Terengganu, Malaysia.
- *Corresponding Author:
- Aye Thandar Htun
Universiti Sultan Zainal Abidin, kuala
terengganu, terengganu Malaysia
E-mail: ayethandarster@gmail.com
Received March 19, 2016; Accepted April 21, 2016; Published April 25, 2016
Citation: Htun TA (2016) A Study on Effectiveness of Ilioinguinal and Iliohypogastricnerve Block at the Time of Wound Closure for Postoperative Pain Relief in Inguinal Hernia Repair. J Pain Relief 5:244. doi:10.4172/2167-0846.1000244
Copyright: ©2016 Htun TA. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.
Visit for more related articles at Journal of Pain & Relief
Abstract
This study was to evaluate the effect of an ilioinguinal-iliohypogastric nerve block with bupivacaine 0.25% on the postoperative analgesia and subsequent analgesic requirements in patients undergoing unilateral open inguinal herniorrhaphy under spinal anaesthesia. Fifty consenting American society of anaesthesiologists (ASA) score I-II patients scheduled for unilateral inguinal herniorrhaphy procedures were given spinal anaesthesia with hyperbaric 0.5% bupivacaine. In a randomized fashion, half of them received an ilioinguinal-iliohypogastric nerve block (IINB) with 30 millilitre (ml) of 0.25% bupivacaine at the time of wound closure and then other half with intramuscular injection of diclofenac sodium 75 milligram (mg). The patients were observed for postoperative 24 hour, such as duration of postoperative analgesia, first on demand analgesic and total analgesic doses, 4 hourly visual analogue scales (VAS), complications of nerve block, 4 hourly haemodynamic changes and assessed patient’s satisfaction at postoperative 12 hour in both groups. The results showed that in comparison with diclofenac group (group B), significantly longer duration of postoperative analgesia in IINB group (group A) (P<0.05%) and the amount required was also significantly less postoperatively in 24 hour (P<0.05%). No complications occurred. Patient’s satisfaction score at postoperative 12 hour was higher in group (A) patients (P<0.05%). There was no significant difference in haemodynamic changes between the two groups. It is concluded that the use of IINB with bupivacaine 0.25% at the time of wound closure in patients undergoing unilateral open inguinal herniorrhaphy under spinal anaesthesia decreased pain and analgesic requirements in the postoperative 24 hour and increased patient’s satisfaction score at postoperative 12 hour.
Keywords
Inguinal herniorrhaphy; Postoperative analgesia; Ilioinguinal and Iliohypogastric nerve block
Introduction
Pain is an extraordinarily complex sensation which is difficult to define and equally difficult to measure in an accurate objective manner [1]
The relief of pain and suffering is one of the primary aims of medicine. Acute pain may be viewed as a benign self-limiting condition or a side effect of disease. Management of post-operative pain may have little or no effect on the patient's eventual outcome and may sometimes be perceived as interfering with the optimal assessment and management of surgical pathology [2].
Acute postoperative pain is a complex physiologic reaction to tissue injury, viscera distension, or disease. Historically, the treatment of postoperative pain has been given a low priority by surgeons and anaesthesiologists. As a result, patients previously accepted pain as an unavoidable part of the postoperative experience. With the development of an expanding awareness of the epidemiology and pathophysiology of pain, more attention is being focused on the management of pain in an effort to improve quality of care and decrease postoperative morbidity and mortality. So, in modern practice, postoperative pain continues to be a challenge for anaesthesiologists [3].
Despite the availability of effective analgesic agents, between 30 to 70% of patients continues to suffer severe postoperative pain. The under treatment of postoperative pain has been identified as one of the most serious deficiencies in pain management today. Our goal is to prevent postoperative pain in an efficient and cost effective manner [4].
Surgical correction of inguinal hernia in adults is one of the most common operations with an annual rate of 2800 per million populations in Europe and the United States.5 In Yangon General Hospital, surgical correction of inguinal hernia in adults in 2004, 2005, 2006 are 150, 127 and 123 cases respectively. Postoperative pain after inguinal hernia repair may persist for one to several weeks, and the consequences of pain may include an extended convalescence period. In addition, some patients may develop chronic disabling pain (0-8%) [5].
Techniques for postoperative analgesia after inguinal hernia repair include systemic analgesics such as non-steroidal antiinflammatory drug (NSAID) or opioids, incisional local anaesthetics, inguinal field block, preemptive analgesia, multimodal analgesia, intrawound analgesics-NSAID or opioids and cryoanalgesia.
An ideal postoperative analgesic should be safe with minimal side effects, give rapid pain relief and easily available. Opioids remain the mainstay of postoperative analgesia traditionally, but their common adverse effects such as itching, nausea and vomiting and their likelihood of drug dependence with frequent use and cost of the drugs are the drawback in their usage [6]. NSAID although they are easily available and widely used, their analgesic potency is not enough to control postoperative pain in some patients [5].
Peripheral nerve blocks provide excellent analgesia over a limited field and with minimal systemic effects. The blocks are generally easy to perform, inexpensive and very safe. The technique is widely used both for surgery and for postoperative pain treatment [3].
In our clinical practice, herniotomy & heniorrhaphy operations are performed under spinal anaesthesia. As postoperative analgesics, we routinely use intramuscular (IM) diclofenac injection or suppository. If the patient complains of pain, further analgesics will be given by pro re nata (p.r.n) basis.
The aim of this study is to evaluate the effectiveness of ilioinguinal and iliohypogastric nerve block at the time of wound closure, in controlling postoperative pain relief after open inguinal hernia repair and to compare with commonly used medication that is diclofenac sodium injection. The result of this study will be beneficial in postoperative pain relief after hernia repair as one of the alternative methods.
Methods
Study Population: Adult patients undergoing elective open inguinal hernia repair operation under spinal anaesthesia
Place of Study: Yangon General Hospital and New Yangon General Hospital, Myanmar
Study Period: From August 2006 to December 2007
Study Design: Hospital based randomized interventional comparative study
Sample Size Determination: A total of 50 male patients, 25 subjects for each method of pain relief were recruited for the study.
Selection of Subjects: (i) Inclusion Criteria
• Age –above 18 year
• ASA PS I, II & III
• -Elective open inguinal hernia repair surgery under spinal anaesthesia
(ii) Exclusion Criteria
• ASA IV and V
• Patients with allergy to local anaesthetics
• Patients with contraindication to spinal anaesthesia
Randomization: Total 50 patients were randomly allocated into two groups (A&B) by using a random (Table 1).
| Characteristics | Group (A) | Group (B) | t | P value* |
|---|---|---|---|---|
| Total number ofpatients | 25 | 25 | ||
| Age(year) Mean(SD) | 45.04(17.19) | 47.32(12.43) | 0.49 | 0.63(NS) |
| Weight(kg) Mean(SD) | 56.56(7.66) | 56.84(5.06) | 0.19 | 0.88(NS) |
| Height(cm) Mean(SD) | 162.8(5.37) | 161.4(5.55) | 0.90 | 0.38(NS) |
| ASA grading(I/II) | 11/14 | 15/10 |
*Paired samples T test.Data are presented as mean and standard deviation. P value < 0.05 is statistically significant. There were no significant statistical differences in age, weight and height between two groups.
Table 1: Patient's demographic characteristics.
Group (A) - Spinal anaesthesia with ilioinguinal and iliohypogastric nerve block after wound closure
Group (B) - Spinal anaesthesia with intramuscular injection of diclofenac after wound closure
All patients for study were seen before the day of surgery for preanaesthetic assessment and preparation for anaesthesia and surgery. Informed consent from each patient was obtained after explaining the procedure.
Anaesthetic machine, all monitors, oxygen supply and required equipment were checked being in perfect working condition. Venous access was secured with 18 gauge (G) intravenous (IV) cannula. Electrocardiogram (ECG), pulse oximeter and non-invasive blood pressure monitor (NIBP) were continuously displayed. Preoperative blood pressure (BP), pulse rate (PR) and oxygen saturation were recorded as baseline data. The resuscitative drugs such as atropine, ephedrine, diazepine and thiopentone were prepared before the procedure. Patient was placed on operating (Table 2) in lateral position. Under aseptic condition, 25 G Quinke spinal needle was inserted into L3-4 or L4-5 interspace. Removed the stylet and confirmed correct placement by noting free flow of cerebrospinal fluid into hub of the needle. Connect the syringe containing the predetermined dose of local anaesthetic (0.5% heavy bupivacaine) and was injected slowly. Remove the needle and place the patient gently into supine position. Closely monitor BP, PR and respiratory function. Determine the ascending sensory level by noting the response to gentle pin prick or cold alcohol swab. When desired level of sensory block (T6) was obtained, operation was started. Monitor the patient cardiovascular status throughout the operation. If there was any complication, the appropriate treatment was given. After wound closure, under aseptic condition:
| Characteristics | Group (A) Group (B) | t | P value | |||
|---|---|---|---|---|---|---|
| Mean | SD | Mean | SD | |||
| Duration of operation(min) | 76.00 | 15.00 | 76.00 | 15.78 | 0.08 | 0.93(NS) |
| Duration of post-opanalgesia(hr) | 16.44 | 8.23 | 8.78 | 5.33 | 4.25 | 0.00(S) |
There was no significant statistical difference in duration of operation between two groups. The duration of postoperative analgesia in group (A) was 16.44 ± 8.23 (hr) and that of group (B) was 8.78 ± 5.33 (hr). There was significant difference in duration of postoperative analgesia (P=0.00).'
Table 2: Comparison of duration of operation and post-op analgesia in two groups.
Group (A) – Ilioinguinal and iliohypogastric nerve block was done by the following way.
The puncture point was identified by skin pencil at the junction union of the lateral quarter with the three medial quarters on the line connecting the anterior superior iliac spine with the umbilicus. A 24 G short bevel needle was inserted in a 45 degree angle to the skin in caudal and medial direction. After passing through the skin and subcutaneous tissue, the needle meets the firm resistance of the external oblique sheath. The needle was then pushed to penetrate this sheath with a definite snap and 30 ml of local anaesthetic (LA) solution (0.25% plain bupivacaine with adrenaline 1:200000 (5 μg/ml)) was injected to each side.
Group (B) - Intramuscular injection of diclofenac sodium 75 mg was given after wound closure.
Patients were assessed 4 hour intervals postoperatively by the author. The VAS scoring was used to assess postoperative pain, determine duration of analgesia and haemodynamic changes and associated complication were noted at these hours. Patients were allowed to ask for intramuscular injection of diclofenac sodium 75 mg as a rescue analgesic if they could not tolerate pain and if necessary, second dose of diclofenac was given and noted.
Patient’s satisfaction score was evaluated at postoperative 12 hour. Data was completed after 24 hour postoperative period and categorized their group accordingly
Pre-recorded data using proforma were processed into computer data entry software the SPSS 11.5 version. Background variables of the subjects, pain scores and rescue pain medication were analyzed and correlated using paired samples T test. Statistical significance of difference between two groups was decided if p value of test statistic was less than 0.05.
Results
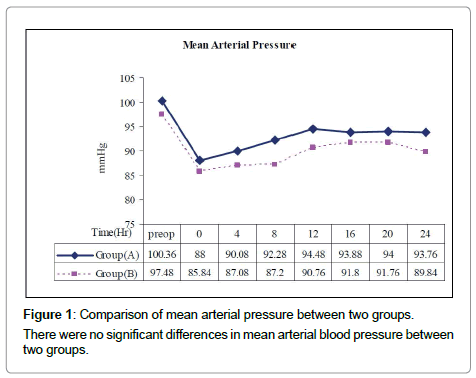
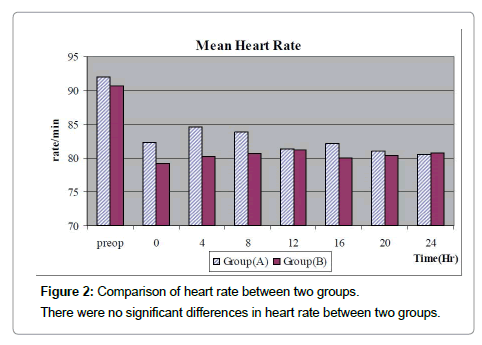
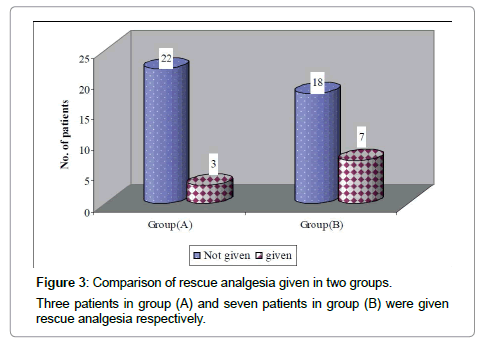
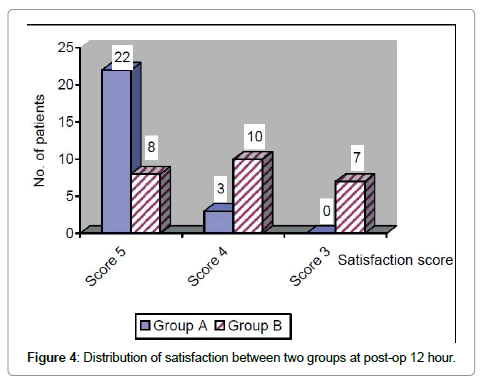
During the period of August 2006 to December 2007, total 50 male patients undergoing unilateral elective inguinal hernia repair under spinal anaesthesia in Yangon general Hospital and New Yangon General Hospital were randomly allocated into two groups by using a random (Tables 3-10) (Figures 1-4).
| First on demand analgesic given time (Hr) | Group (A) | Group (B) | t | P value |
|---|---|---|---|---|
| Number of patients given analgesia | 3 | 7 | ||
| Mean (SD) | 7.33 (3.06) | 9.29 (4.57) | 0.67 | 0.52 (NS) |
| Median duration | 8 | 8 | ||
| Minimum duration | 4 | 5 | ||
| Maximum duration | 10 | 17 |
Data are presented as minimum, maximum and median duration and mean first on demand analgesic given time with standard deviation. There was no significant difference in first on demand analgesic given time between two groups.
Table 3: Comparison of first on demand analgesic given time (hr) between two groups.
| Hour | Group A | Group B | t | P value | ||||||
|---|---|---|---|---|---|---|---|---|---|---|
| Minimum | Maximum | Mean | SD | Minimum | Maximum | Mean | SD | |||
| 4 | 0 | 8 | 0.56 | 1.960 | 0 | 6 | 1.24 | 2.107 | 1.345 | 0.19* |
| 8 | 0 | 6 | 0.84 | 1.675 | 0 | 6 | 2.24 | 2.368 | 2.763 | 0.01* |
| 12 | 0 | 4 | 0.36 | 1.036 | 0 | 6 | 2.84 | 2.304 | 5.283 | 0.00* |
| 16 | 0 | 4 | 0.32 | 0.945 | 0 | 6 | 1.28 | 1.792 | 2.274 | 0.03* |
| 20 | 0 | 3 | 0.40 | 0.957 | 0 | 5 | 0.44 | 1.294 | 0.116 | 0.90 |
| 24 | 0 | 0 | 0.00 | 0.000 | 0 | 4 | 0.24 | 0.879 | 1.365 | 0.18 |
* = statistically significant Data are presented as minimum, maximum, mean and standard deviation. VAS scores in group A at 8, 12 and 16 hr were 0.84 ± 1.675, 0.36 ± 1.036 and 0.32 ± 0.945 respectively. VAS scores in group B at 8, 12 and 16 hr were 2.24 ± 2.368, 2.84 ± 2.304 and 1.28 ± 1.792 respectively. There were significant difference in VAS scores in two groups at 8, 12 and 16 hr (P=0.01, 0.00, 0.03).
Table 4: Comparison of VAS pain score between two groups.
| Characteristics | Group (A) Mean(SD) | Group (B) Mean(SD) | t | P value |
|---|---|---|---|---|
| Systolic blood pressure (mmHg) | 135.00(18.54) | 131.60(13.36) | 0.70 | 0.49 |
| Diastolic Blood pressure (mmHg) | 83.60(11.59) | 80.20(10.15) | 1.03 | 0.31 |
| Mean Arterial Pressure (mmHg) | 100.36(13.49) | 97.48(10.02) | 0.83 | 0.42 |
| Heart Rate (/min) | 92.04(13.15) | 90.76(11.47) | 0.39 | 0.69 |
Data are presented as mean and standard deviation. There were no significant differences in preoperative baseline physiological variables between two groups.
Table 5: Preoperative (baseline) physiological variables.
| Time(Hr) | Group (A) Group (B) | t | P value | |||
|---|---|---|---|---|---|---|
| Mean | SD | Mean | SD | |||
| Preop | 135.00 | 18.540 | 131.60 | 13.364 | 0.700 | 0.490 |
| 0 | 118.04 | 17.712 | 115.24 | 12.722 | 0.637 | 0.5.30 |
| 4 | 122.40 | 14.442 | 116.20 | 12.186 | 1.656 | 0.111 |
| 8 | 124.60 | 15.473 | 119.28 | 11.549 | 1.314 | 0.201 |
| 12 | 127.20 | 16.651 | 120.60 | 9.823 | 1.760 | 0.091 |
| 16 | 129.4 | 14.31 | 122.40 | 11.648 | 1.95 | 0.06 |
| 20 | 126.40 | 15.513 | 121.80 | 10.790 | 1.178 | 0.250 |
| 24 | 125.00 | 16.583 | 119.40 | 12.017 | 1.421 | 0.168 |
Table 6: Systolic blood pressure (mmhg) in two groups.
| Time(Hr) | Group (A) Group (B) | t | P value | |||
|---|---|---|---|---|---|---|
| Mean | SD | Mean | SD | |||
| Preop | 83.60 | 11.594 | 80.20 | 10.153 | 1.034 | 0.311 |
| 0 | 75.00 | 10.778 | 70.52 | 8.171 | 2.013 | 0.055 |
| 4 | 77.00 | 7.638 | 73.00 | 8.292 | 1.789 | 0.086 |
| 8 | 75.80 | 8.742 | 71.40 | 6.042 | 1.963 | 0.061 |
| 12 | 79.60 | 9.456 | 76.20 | 6.658 | 2.028 | 0.054 |
| 16 | 77.60 | 7.789 | 77.20 | 6.934 | 0.242 | 0.811 |
| 20 | 78.40 | 10.966 | 76.80 | 7.890 | 0.520 | 0.608 |
| 24 | 76.80 | 11.075 | 75.60 | 8.206 | 0.417 | 0.680 |
Data are presented as mean and standard deviation. There were no significant differences in systolic and diastolic blood pressure between two groups.
Table 7: Diastolic blood pressure (mmhg) in two groups.
| Group (A) | Group (B) | |||
|---|---|---|---|---|
| No. | Percent | No. | Percent | |
| Moderate pain but need medication (score3) | - | - | 7 | 28.0 |
| Mild pain but can withstand (Score4) | 3 | 12.0 | 10 | 40.0 |
| No pain at all (Score5) | 22 | 88.0 | 8 | 32.0 |
| Total | 25 | 100.0 | 25 | 100.0 |
Data are presented as number and percent of patients between two groups. Patients receiving score 5 (no pain at all) in group (A) was 22 (88%) and in group (B) was 8 (32%).
Table 8: Comparison of level of satisfaction at post-operative 12 hour between two groups.
| Mean satisfaction score | Std. Devation | t | P value | |
|---|---|---|---|---|
| Group (A) | 4.88 | 0.33 | 4.91 | 0.00(S) |
| Group (B) | 4.04 | 0.79 |
Data are presented as mean and standard deviation. Satisfaction score in group A at postoperative 12 hour was 4.88 ± 0.33 and that of group B was 4.04 ± 0.79 respectively. There was significant statistical difference in satisfaction score at postoperative 12 hour between two groups (P=0.00).
Table 9: Comparison of satisfaction score between two groups.
| Complications | Yes/No |
|---|---|
| Haematoma | No |
| LA toxicity | No |
| Vascular puncture | No |
There was no incidence of complications associated with nerve block during postoperative 24 hour.
Table 10: Complications of nerve block.
Discussion
Postherniorrhaphy pain is a significant clinical problem that may have economic consequences because it can prolong convalescence [7]. The purpose of this study was to evaluate the benefits of IINB for postherniorrhaphy pain. The primary end-point was IM diclofenac injection as we hypothesized that an effective IINB should decrease the need for NSAID analgesia. IINB have been reported to produce excellent postoperative pain control in adults and children following such treatment as hernia repair and groin surgery. The nerve block has also been assessed for reducing pain following caesarean section [8]. According to previous studies we used bupivacaine as our local anaesthetic due to its long acting effects. The study by Dierking and colleagues suggested that the duration of action of lidocaine is too short to prevent postoperative central sensitization.
In this study, bupivacaine 0.25% was used. The use of a higher concentration of bupivacaine (0.5%) might have provided more effective and longer lasting postoperative analgesia. However, in a previous study in 1995 by Harrison CA, involving preincisional IINB and wound infiltration, bupivacaine 0.5% failed to produce an analgesic effect beyond the first six hour after elective hernia repair [9]. Adrenaline 1:200000 (5 μg/ml) was added to 0.25% bupivacaine solution in this study. This was evidenced by Yee [10]. She found that bupivacaine infiltration with adrenaline can produce more prolonged duration of analgesia compared with bupivacaine alone for postoperative pain relief in inguinal hernia repair. Complications associated with the use of adrenaline such as haemodynamic derangements were not reportedly found. In the current study, we measure SBP, DBP, MAP and HR as preoperative baseline variables and at 4 hour interval postoperatively. There were no significant changes between these variables in these groups.
NSAIDs are frequently used to treat mild to moderate pain and as a component of multimodal regimens for moderate to severe pain. In 1998, the Royal College of Anaesthetists issued guidelines for the use of NSAIDs in the peri-operative period. Based on the strongest evidence available, it is stated that ‘In situations where there are no contraindications, NSAIDs are the drug of choice after many day-case procedures’. However, controversy still surrounds the use of NSAIDs because of their significant gastrointestinal, haematological and renal side effects [3]. The current study failed to observe these side effects. Regarding to failure of nerve block, there were 5 patients who had block failure and we excluded them from this study. This study determined the case as block failure when the patient complaints of pain after 3 hour from the start of spinal anaesthesia as the duration of action of spinal anesthesia usually last for 2-3 hour. In 2006, Kudra et al. found that IINB can be successfully accomplished from any point if the needle bevel lies between the two muscle planes above and below the internal oblique. Overall failure rate of IINB was 6% among 102 children in their study groups [11].
This study observed the complications of nerve block such as haematoma, LA toxicity and vascular puncture upto postoperative 24 hour. But there were no complications within the study group. In 1995, DingY and Paul EW studied the effect of an IINB with bupivacaine 0.25% on the postoperative analgesic requirement and recovery profile in outpatients undergoing inguinal herniorrhaphy with LA infiltration. They concluded that the use of IINB with bupivacaine 0.25% as an adjuvant during inguinal herniorrhaphy under monitored anaesthesia care (MAC) decreased pain in the PACU and oral analgesic requirements after discharge from the day-surgery unit. In the present study, we use spinal anaesthesia instead of MAC and nerve block was performed at the time of wound closure. Volume and concentration of bupivacaine were the same [6].
The previous studies demonstrated IINB or infiltration either preincision or postincision. But Lee et al. could not demonstrate the pre-emptive analgesic effect of preincisional bupivacaine infiltration [12]. Similarly, Toivonen et al. studied the effect of preincisional IINB on postoperative analgesic requirement in day-surgery patients undergoing herniorrhaphy under spinal anaesthesia [13]. They concluded that no long-term analgesia could be demonstrated by a preincisional IINB performed during spinal anaesthesia in day-surgery inguinal herniorrhaphy patients. Thus, reduced analgesic requirement was seen only for about 6 hour postoperatively. For this reason, IINB was performed at the time of wound closure in our study.
There are several studies of IINB in children undergoing inguinal hernia repair under general anaesthesia and 0.25% bupivacaine was commonly used. In 1999, Dr. Nu Nu May found that IINB with bupivacaine 0.25% was effective in perioperative and postoperative pain in children undergoing inguinal hernia repair. In contrary to children, as we performed IINB in adults in this study, surgery was done under spinal anaesthesia.
For assessment of pain in the current study, the primary outcome assessment was a reduction in VAS scores. It was observed that reduction in VAS pain scores at 8, 12 and 16 hour postoperative period in group A. It was statistically significant as well as clinically relevant. There were no significant differences in the time needed for first on demand analgesic dose and cumulative amount of rescue analgesic doses.
The limitation of this study was inability to evaluate the postoperative pain of the patients after 24 hr and side effects of diclofenac sodium injection. The author would like to suggest future study should evaluate the incidence of chronic pain state after inguinal hernia repair in our country.
In summary, IINB at the time of wound closure provided superior analgesia for upto 24 hour after unilateral inguinal herniorrhaphy compared to IM diclofenac sodium injection. This method was safe and no associated complication was reportedly found.
Conclusion
Inguinal hernia repair is one of the most common surgical procedures all over the world. The challenge to the anaesthetists is to provide optimal postoperative pain relief after hernia repair. The prevention of acute postoperative pain is so important because it has the risk of transition to chronic pain state. There is substantial evidence that ilioinguinal-iliohypogastric nerve block gives excellent postoperative pain relief after hernia repair. Outcome of this study revealed that ilioinguinal-iliohypogastric nerve block with 0.25% bupivacaine at the time of wound closure after unilateral open inguinal herniorrhaphy provided superior, efficacious postoperative pain relief without complications than traditional use of intramuscular injection of diclofenac sodium.
References
- Smith G (2001) Postoperative pain. In:Aitkanhead AR, Rowbothan DJ (eds.) Text Book ofAnaesthesia.Edinburgh: Churchill living stone p: 544-554.
- Cooper JG, Haetzman M, Stickle BR (2001) Effective post-operative analgesia:Educational review.
- Rawal N (2001) Analgesia for day-case surgery. Br J Anaesth 87: 73-87.
- Moote CA (1994) The prevention of postoperative pain. Can J Anaesth 41: 527-533.
- Callesen T, Bech K, Thorup J, Andersen J, Nielsen R, et al. (1998) Cryoanalgesia: effect on postherniorrhaphy pain. AnesthAnalg 87: 896-899.
- Yifeng D, Paul FW (1994) Postherniorrhaphy pain in outpatients after preincision ilioinguinal-iliohypogastric nerve block during monitored anaesthesia care. Canadian Journal of Anaesthesia 42: 12-15
- Bell EA, Jones BP, Olufolabi AJ, Dexter F, Phillips-Bute B, et al. (2002) Iliohypogastric-ilioinguinal peripheral nerve block for post-cesarean delivery analgesia decreases morphine use but not opioid-related side effects. Canadian journal of anesthesia49: 694-700.
- Harrison CA, Morris S, Harvey JS (1994) Effect of ilioinguinal and iliohypogastric nerve block and wound infiltration with 0.5% bupivacaine on postoperative pain after hernia repair. Br J Anaesth 72: 691-693.
- Yi KP (1998) A study of effectiveness of bupivacaine infiltration at the time of wound closure for postoperative pain relief in inguinal hernia repair. M.Med.Sc(Anaesthesiology) Dissertation.
- Kundra P, Sivashanmugam T, Ravishankar M (2006) Effect of needle insertion site on ilioinguinal-iliohypogastric nerve block in children. ActaAnaesthesiolScand 50: 622-626.
- Lee IH, Lee IO, Kong MH, Lee MK, Kim NS (2000) The preemptive analgesic effect of bupivacaine infiltration on postoperative pain after inguinal herniorrhaphy. Korean Journal of Anaesthesia 38:645-650.
- Toivonen J, Permi J, Rosenberg PH (2001) Effect of preincisional ilioinguinal and iliohypogastric nerve block on postoperative analgesic requirement in day-surgery patients undergoing herniorrhaphy under spinal anaesthesia. ActaAnaesthesiolScand 45: 603-607.
- May NN (1999) a study of perioperative pain relief in Paediatric Inguinoscrotal surgery with field block technique. M.Med.Sc(Anaesthesiology) Dissertation.
Relevant Topics
- Acupuncture
- Acute Pain
- Analgesics
- Anesthesia
- Arthroscopy
- Chronic Back Pain
- Chronic Pain
- Hypnosis
- Low Back Pain
- Meditation
- Musculoskeletal pain
- Natural Pain Relievers
- Nociceptive Pain
- Opioid
- Orthopedics
- Pain and Mental Health
- Pain killer drugs
- Pain Mechanisms and Pathophysiology
- Pain Medication
- Pain Medicine
- Pain Relief and Traditional Medicine
- Pain Sensation
- Pain Tolerance
- Post-Operative Pain
- Reaction to Pain
Recommended Journals
Article Tools
Article Usage
- Total views: 11648
- [From(publication date):
May-2016 - Jul 19, 2025] - Breakdown by view type
- HTML page views : 10688
- PDF downloads : 960