A Study on Diagnostic Indicators Differentiating AFRS and EMRS
Received: 07-May-2019 / Accepted Date: 17-May-2019 / Published Date: 24-May-2019 DOI: 10.4172/2161-119X.1000370
Abstract
Objectives: Allergic fungal rhinosinusitis (AFRS) and Eosinophilic mucin rhinosinusitis (EMRS) are two commonly encountered entities in our institution. In this study we intended to observe the diagnostic indicators by clinical, laboratory, histopathology and radiology of these two entities. This will help us understand the disease better.
Methods: In total, 74 rhinosinusitis patients with nasal polyposis with eosinophilic mucin were enrolled. They were divided into two groups depending on the presence of fungal elements in the nasal secretion-AFRS (polyp, fungal elements, mucin) and EMRS (polyp, no fungal elements, mucin). Evaluation of these two groups included clinical assessment, mucin histopathology, serum IgE levels and Computed tomography (CT) of Paranasal sinuses (PNS) with measurement of Hyper attenuation areas (HAA) with Hounsefield units (HU).
Results: 29 patients were enrolled in AFRS group and 45 patients in the EMRS group. We observed that the EMRS group of patients had 100% bilateral presentation compared to AFRS group (31%), The IgE levels were significantly higher in the AFRS group. Hyper attenuation areas were noted only in the CT of the AFRS group measured using Hounsfield units. It was noted that bronchial asthma was more closely associated with the EMRS group.
Conclusion: AFRS occurs in individuals who develop an atopic reaction to the fungal elements within the sinuses, whereas EMRS seems to occupy the other end of spectrum where there is no trace of fungal elements but they seem to be part of a systemic disease process. This study helps us to understand the difference with regard to clinical, histopathology studies and CT-PNS in these two groups.
Keywords: Rhinosinusitis; Histopathology; Radiology; Fungal elements
Introduction
Chronic sinusitis is a common illness, however, the etiopathogenesis of the subsets in the disease is varied. One such presentation is chronic sinusitis with nasal polyposis, eosinophilia and mucinous sinus disease. The widely recognised criterion for diagnosis of AFRS was described by Bent and Kuhn [1] who after their research found patients with AFRS are associated with Type 1 hypersensitivity, positive skin test, presence of a nasal polyp, typical CT findings, eosinophilia in mucin, positive fungal staining without fungal invasion in sinus tissue. These patients are generally difficult to treat by medical and surgical methods [2]. Allergens, superantigens and bacteria are typically involved in the ensuing sinusitis at the time of presentation to the outpatient department and are thought to be responsible for the pathophysiology of the disease [3].
In a study, Millar et al. [4] was the first to demonstrate sinus specimens were histologically akin to allergic bronchopulmonary aspergillosis (ABPA). Katzenstein et al. [5] found in his study that after subjecting the materials from sinus surgery for chronic sinusitis to histology, he observed the presence of Charcot-Leyden crystals, eosinophils and fungal hyphae. He called this as allergic mucin and described the term allergic Aspergillus sinusitis. Many years after Robson et al. [6] spoke about the term ‘allergic fungal sinusitis’ after observing that not only the Aspergillus but also other fungi were present in the cultures of specimens from chronic sinusitis.
Eosinophilic mucin rhinosinusitis (EMRS) is another common entity in this part of the world. These patients typically present with bilateral nasal polyposis with eosinophilic mucin without the fungal elements. There is also evidence for frequent association with bronchial asthma in this group of patients.
The study conducted in our institution was based on these two groups, group 1 (AFRS) and group 2 (EMRS). They were divided based on the presence or absence of the fungal hyphae. This study aims at analysing the diagnostic indicators differentiating AFRS and EMRS.
Materials and Methods
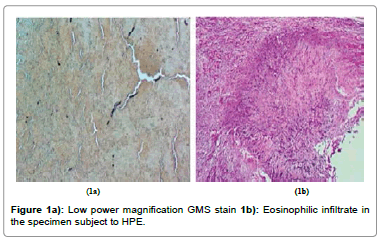
We conducted the study after the approval of the Institutional human ethics committee in the Department of Otorhinolaryngology, Department of Pathology, and Department of Radiology of our institution from Jan 2016 to July 2018. We reviewed patients who presented with the triad of nasal polyposis, eosinophilia and mucin. In total 74 patients were selected, and were separated into two groups Allergic fungal rhinosinusitis (AFRS) and Eosinophilic mucin rhinosinusitis (EMRS) based on the fungal hyphae identification. Group 1/AFRS group stained positive for fungal material and presented with polyposis, whereas group 2/EMRS did not have fungal elements in the mucin, both presented with polyposis. With these criteria 29 patients were grouped under AFRS and 45 patients under EMRS. All 74 patients underwent anterior rhinoscopy and Diagnostic nasal endoscopy (DNE) with 0 degrees and 30 degrees Hopkin’s telescope and Karl Storz camera system. The mucin collected from the nasal cavity was subjected to histopathological examination. Histology sections were preserved with the help of 10% buffered formalin. Staining was done with hematoxylin and eosin, PAS, and Gomori ‘s methenamine silver to identify fungal materials (Figure 1a and 1b). All 74 patients had their serum IgE and absolute eosinophil count tested. An absolute eosinophil count of more than 440 cells/μL was considered to indicate eosinophilia in our study. Computed tomography of Paranasal sinuses (CT-PNS) was taken to look for hyper attenuation areas and the Hounsfield units (HU) of the hyper attenuation areas (HAA) were measured. We assessed the presence of bone erosion, the number of sinuses involved and sinus wall expansion. History/ treatment of Bronchial asthma was recorded. All patients underwent Functional endoscopic sinus surgery (FHFESS) with preoperative evaluation and anaesthetic concurrence. A powered instrument like microdebrider was used for the procedure. Results were tabulated and the two groups were compared.
PASW ver. 18.0 was adopted for statistical study. Chi-square test was used to determine differences between for epidemiology, BA, counts, IgE values and HU values. A P-value<0.05 was considered to be statistically significant.
Results
All the parameters observed were recorded and tabulated (Table 1). Epidemiologically, younger people seem to be more involved with AFRS than EMRS, though there was no statistical difference (P=0.128). Male to Female ratio was not significant enough between the two groups (2.25:1-1.6:1).
| Variables | AFRS (Group 1) | EMRS (Group 2) |
|---|---|---|
| n=74 | 29 | 45 |
| Age | 33.3 | 42.4 |
| Gender (Male : Female) | 2.25 : 1 | 1.6 : 1 |
| Bronchial asthma | 3/29(10%) | 29/45(64%) |
| Eosinophil count | 522 | 606 |
| Serum IgE | 706.15 IU/ml (p<0.001) | 164.96 IU/ml |
| CT imaging | ||
| Bilateral disease | 20/29(68%) | 45/45(100%) |
| HAA (HU) | 112.2 HU (p<0.05) | 73.9 HU |
| Expansion | 8/29 (27%) | none |
| Surgical method | TFSE/FH-FESS | TFSE/FH-FESS |
| Oral steroids | Yes | Yes |
| Recurrence | 12/29(41%) | 21/45(465) |
Table 1: The demographic, clinical and investigation of the two groups.
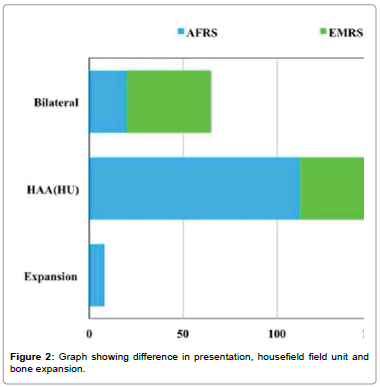
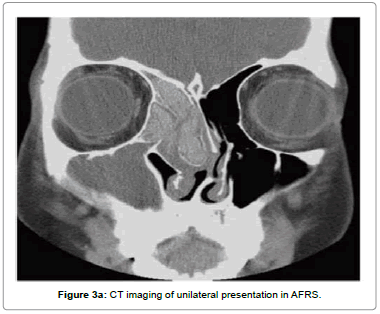
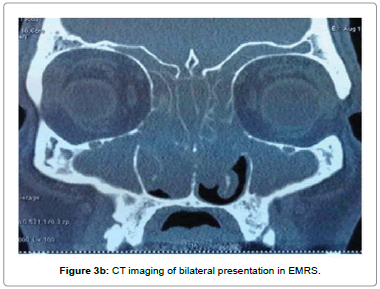
It was observed that only 7.7% of patients with AFRS had bronchial asthma, whereas 65.4% of patients with EMRS had episodes of bronchial asthma previously (P=0.001) (Figure 2). 31% of patients in the AFRS group had bilateral disease, whereas 100% of the EMRS patients had bilateral disease (P<0.001) (Figure 2, Figure 3a and 3b). The number of patients who had revision surgery to alleviate the disease was more in group 1 than in group 2.
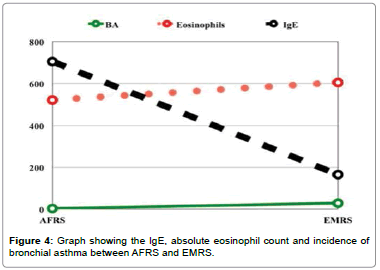
Laboratory findings revealed that the serum IgE levels in the AFRS group (706.15 IU/mL) was higher than in the EMRS group of patients (164.96 IU/mL, P<0.05). 69.2% of the AFRS group and 76.9% of the EMRS group had eosinophilia (absolute eosinophil count >440 cells/ μL). The differences were not statistically significant (Figure 4).
Radiologically, all patients in the AFRS group had hyper attenuation areas (HAA) on a CT scan, as compared to 73% of patients in the EMRS group (P=0.039). The HU scores of hyper attenuation areas in the AFRS group of patients (112.2 HU) was significantly more than the EMRS group of patients (73.9 HU; P<0.001) (Figure 2). 27% of the AFRS patients had the expansion of the sinus cavity.
All patients with AFRS and EMRS were treated with endoscopic sinus surgery for ventilation and drainage. Oral prednisone was used in all the patients in the immediate postoperative period at 0.25 mg/kg every morning for 10 days and then tapered off over the next ten days.
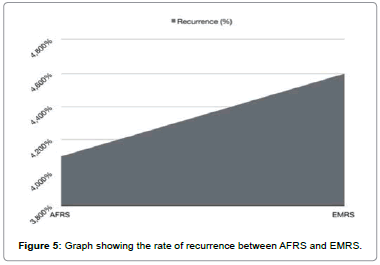
Among the AFRS group, 12 out of the 29 patients had recurrence at three months follow up (Figure 5). Among the EMRS group, 21 out of the 45 patients had recurrence at 3 months follow up. In total, 23 patients had a recurrence (both groups) and among them, 11 patients needed revision surgery. Rest of the patients were managed with oral and intranasal corticosteroids.
Discussion
Although the International mycology society has given some guidelines for classifying the group of patients, it needs more definition and better understanding [7]. The study conducted in our institution was based on just two groups, group 1 (AFRS) and group 2 (EMRS). Over the past two decades, fungal etiopathogenesis in chronic sinusitis has had its proportions of supporters and detractors [8]. However, even now most of the rhinologists try to maintain a distinction between AFRS and other causes of chronic sinusitis [8,9].
Ramadan and Quraishi [10] documented that AFRS occurs in a younger population. The same was evident in our study but there was no statistical difference. Ferguson [11] reported that 41% of patients with AFRS were asthmatic, compared with 93% of patients with EMRS. Another study noted that 100% of patients with eosinophilic mucin rhinosinusitis without hyphae had asthma, whereas merely 25% of patients with AFRS had asthma [10]. In the present study, similar results were seen; 65% of patients with EMRS were asthmatic, while just 10% in the AFRS group had asthma. This indicates that EMRS could be a part of systemic disease.
The IgE values were more in AFRS patients, sometimes reaching a value of >1,000 IU/mL [12,13]. Many studies have documented higher IgE values in AFRS group of patients than in EMRS patients [9,11]. Although the difference between the group is not statistically significant, it helps in predicting the recurrence rates after treatment [9]. Our study showed similar results. 69% of patients in the AFRS group and 77% in the EMRS group had an increase in eosinophil count in our study. The difference was not statistically significant.
Many studies have documented the laterality of the disease using imaging [11,14]. Ferguson [11] documented that EMRS was constantly documented as bilateral disease, while AFRS was almost always unilateral disease in half of all cases. In our study, 69% of patients with AFRS had bilateral disease, while all the patients with EMRS had bilateral disease.
The radiologic imaging is pathognomonic in the diagnosis of the disease spectrum. It was documented in earlier studies that there was increased attenuation/hyperdense areas in CT of paranasal sinuses of AFRS patients [15]. These hyper attenuation areas in AFRS are because of the likely deposition of heavy metals, calcium, and inspissated intra sinus debris [14]. In the study conducted in our institution, the areas of hyper attenuation were documented in all patients diagnosed with AFRS, while only 73% of patients EMRS group showed them. The hyper attenuation areas were statistically significant between the two groups (P=<0.001). The HU score in the areas of hyper attenuation (HAA) in the AFRS group of patients was significantly more than in the EMRS group of patients.
In the AFRS group of patients, demineralisation of the sinus wall bones can occur, resulting in thinning of the sinus wall and of the sinus. Many authors documented that bone erosion is because of the pressure atrophy by the ever-increasing mucin content and the effects of inflammatory mediators within it and not because of the fungal invasion [16]. Nussenbaum et al. [17] documented that bone erosion into anatomical regions was encountered in 20% of patients with AFRS. In our study, 23% of patients in the AFRS group had erosion and expansion of the sinus, while none of them in the EMRS group showed any expansion of the sinus. The accumulation of allergic mucin obstructs the involved sinuses and exacerbates the problem [17].
The treatment modalities are similar for AFRS and EMRS group of patients. Treatment requires surgery and aggressive postoperative medical management with close follow-up [13,18]. Surgery is the treatment of choice. Functional Endoscopic Sinus Surgery was sufficient to clear the inspissated mucin and debris to help in continued sinus drainage. Systemic corticosteroids form an integral part in the treatment of AFRS [19]. This medical therapy is essential because these diseases have a tendency to recur. It is documented that serum IgE levels and eosinophil counts are valid indicators for recurrence of the disease.
The predicted recurrence rate for sinusitis with polyposis is 60% according to a study. All the patients were assessed at the end of three months. In our study, 12 out of the 29 patients had a recurrence in the AFRS group and 21 out of the 45 patients had a recurrence in the EMRS group. Out of the 23 recurrences (both groups), 11 patients needed revision surgery. Rest of the patients were managed with oral and intranasal corticosteroids. Thus, long-term follow-up is essential in both diseases.
Conclusion
It is evident from our study that the AFRS group of patients had higher IgE values, increased eosinophil counts and hyper attenuation areas (HAA) in CT scans with unilateral involvement in most of the cases. The EMRS group of patients showed a higher incidence of asthma than the AFRS group with a uniformly bilateral disease with lower IgE levels when compared with the AFRS patients. Also, we observed that EMRS is a systemic disease(bilaterality and association with asthma) that needs long-term follow up. The Hyper attenuation areas (HAA) and the mean HU scores for the contents were significantly lower in the EMRS group than in the AFRS group of patients. We hope that an elaborate randomised prospective study in the future will give a greater understanding of these disease entities.
Limitations
Follow up schedule was a major hindrance to the study.
Declaration of Ethical Issues
The author hereby declares that there were no ethical issues involved in the publishing of this article in any journal.
Declaration of Conflicting Interests
The author(s) declared the following potential conflicts of interest with respect to the research, authorship, and/or publication of this article: The authors certify that they have no affiliations with or involvement in any organisation or entity with any financial interest or non-financial interest in the subject matter or materials discussed in this manuscript.
Funding
The author(s) received no financial support for the research, authorship, and/or publication of this article.
References
- Bent JP, Kuhn FA (1994) Diagnosis of allergic fungal sinusitis. Otolaryngol Head Neck Surg 111: 580-588.
- Sok JC, Ferguson BJ (2006) Differential diagnosis of eosinophilic chronic rhinosinusitis. Curr Allergy Asthma Rep 6: 203-214.
- Borish L, Rosenwasser L, Steinke JW (2006) Fungi in chronic hyperplastic eosinophilic sinusitis: reasonable doubt. Clin Rev Allergy Immunol 30: 195-204.
- Millar JW, Johnston A, Lamb D (1981) Allergic aspergillosis of the maxillary sinuses [abstract] Thorax 36: 710.
- Katzenstein AL, Sale SR, Greenberger PA (1983) Allergic Aspergillus sinusitis: a newly recognized form of sinusitis. J Allergy Clin Immunol 72: 89-93.
- Robson JM, Hogan PG, Benn RA, Gatenby PA (1989) Allergic fungal sinusitis presenting as a paranasal sinus tumour. Aust N Z J Med 19: 351-353.
- Chakrabarti A, Denning DW, Ferguson BJ, Ponikau J, Buzina W, et al. (2009) Fungal rhinosinusitis: a categorization and definitional schema addressing current controversies. Laryngoscope 119: 1809-1818.
- Hamilos DL (2010) Allergic fungal rhinitis and rhinosinusitis. Proc Am Thorac Soc 7: 245-252.
- Hutcheson PS, Schubert MS, Slavin RG (2010) Distinctions between allergic fungal rhinosinusitis and chronic rhinosinusitis. Am J Rhinol Allergy 24: 405-408.
- Ramadan HH, Quraishi HA (1997) Allergic mucin sinusitis without fungus. Am J Rhinol 11: 145-147.
- Ferguson BJ (2000) Eosinophilic mucin rhinosinusitis: a distinct clinicopathological entity. Laryngoscope 110: 799-813.
- Collins M, Nair S, Smith W, Kette F, Gillis D et al. (2004) Role of local immunoglobulin E production in the pathophysiology of noninvasive fungal sinusitis. Laryngoscope 114: 1242-1246.
- Schubert MS, Goetz DW (1998) Evaluation and treatment of allergic fungal sinusitis. I. Demographics and diagnosis. J Allergy Clin Immunol 102: 387-394.
- Mukherji SK, Figueroa RE, Ginsberg LE, Zeifer BA, Marple BF et al. (1998) Allergic fungal sinusitis: CT findings. Radiol 207: 417-422.
- Bozeman S, de Shazo R, Stringer S, Wright L (2011) Complications of allergic fungal sinusitis. Am J Med 124: 359-368.
- Manning SC, Holman M (1998) Further evidence for allergic pathophysiology in allergic fungal sinusitis. Laryngoscope 108: 1485-1496.
- Nussenbaum B, Marple BF, Schwade ND (2001) Characteristics of bony erosion in allergic fungal rhinosinusitis. Otolaryngol Head Neck Surg 124: 150-154.
- Schubert MS (2001) Fungal rhinosinusitis: diagnosis and therapy. Curr Allergy Asthma Rep 1: 268-276.
- Hamilos DL (2011) Chronic rhinosinusitis: epidemiology and medical management. J Allergy Clin Immunol 128: 693-707.
Citation: Ramalingam V, Kamindan K, Kumar A, Karthikeyan (2019) A Study on Diagnostic Indicators Differentiating AFRS and EMRS. Otolaryngol (Sunnyvale) 9: 370. DOI: 10.4172/2161-119X.1000370
Copyright: © 2019 Ramalingam V, et al. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.
Share This Article
Recommended Journals
Open Access Journals
Article Tools
Article Usage
- Total views: 3834
- [From(publication date): 0-2019 - Apr 03, 2025]
- Breakdown by view type
- HTML page views: 3050
- PDF downloads: 784