A Staining Artefact Presumed to be Pathology in a Patient Investigated for Megaloblastic Anaemia and Myelodysplastic Syndrome: A Case Study at Groote Schuur Hospital
Received: 02-Nov-2019 / Accepted Date: 13-Nov-2019 / Published Date: 25-Nov-2019 DOI: 10.4172/2476-2024.1000156
Abstract
Artefacts are structures that are not normally present in well prepared smears. Well stained smears are the cornerstone of diagnostic haematology and this requires properly stained smears achieved by adherence to standard operating procedures (SOPs) to ensure reliability of results. Artefacts on smears may baffle the examiner and may in fact be assessed as real pathology by an inexperienced examiner or conceal real pathology. This case report describes a patient who was referred to the haematology department for work-up of a macrocytic anaemia to exclude megaloblastic anaemia and myelodysplastic syndrome. The initial blood smear processed consisted of numerous basophilic stippling-like inclusions which was perplexing as the degree of BS has never been encountered before. This prompted a repeat of the blood smear which showed resolution of the artefact. Basophillic stippling can be seen in megaloblastic anaemia and myelodysplastic syndromes.
Keywords: Basophilic stippling; Staining artifact; Megaloblastic anaemia; Myelodysplastic syndrome
Abbreviations
BS: Basophilic Stippling; SOPs: Standard Operating Procedures; PAS: Periodic Acid Schiff; RBC: Red Blood Cell
Introduction
Stains are used in haematology pathology to highlight cell morphology. The stain used in our laboratory for staining peripheral blood and bone marrow aspirate smears is the Diff-Quick stain which is a brand of the Romanowski stain. The main components of a Romanowski stain are:
A cationic or basic dye (methylene blue or its oxidation products such as azure B), which binds to anionic sites on proteins and gives a blue-grey color to nucleic acids (DNA or RNA), nucleoproteins, granules of basophils and weakly to granules of neutrophils.
An anionic or acidic dye, such as eosin Y or eosin B, which binds to cationic sites on proteins and gives an orange-red colour to haemoglobin and eosinophil granules [1].
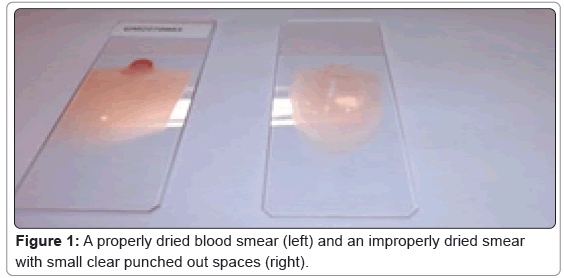
The correct procedure for preparation of smears for cell morphology is to prepare smears of adequate length and to allow the smear to air dry properly before staining. Figure 1 shows properly dried and improperly dried blood smears.
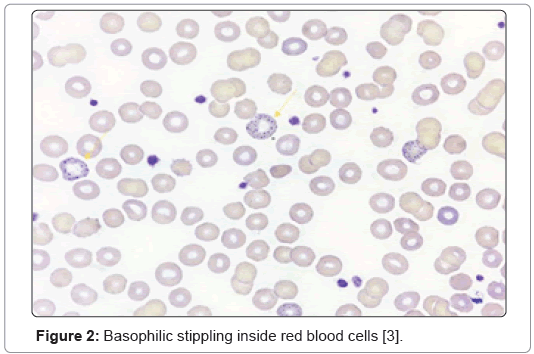
Improper smear processing in this case resulted in an artefact inside red blood cells that was presumed to be Basophilic Stippling (BS). Though very occasional cells with basophilic stippling can be seen in normal people, increased numbers are seen in megaloblastic anaemia, dyserythropoieticstates, thalassemia, lead poisoning, a variety of haemolytic anaemias, Pyramidine 5 nucleotidase deficiency etc. [2-5]. Figure 2 shows true basophilic stippling inside red blood cells.
Figure 2: Basophilic stippling inside red blood cells [3].
Case Study
A 49-year-old female patient was referred to haematology for a work-up of a long standing macrocytic anaemia to rule out megaloblastic anaemia or a myelodysplastic syndrome. She had a background history of diabetes, hypertension, nephrotic syndrome and is partially blind. She was on no drugs that could cause the anaemia and there was no history of haemorrhage (Table 1).
| FBC | Differential count | ||
|---|---|---|---|
| WCC | 4.25 × 109/L | Neutrophils | 62% |
| Hb | 5.2 g/dL | Lymphocytes | 29.40% |
| MCV | 108.2 fL | Monocytes | 4.90% |
| PLT | 189 × 109/L | Eosinophils | 1.60% |
| Basophils | 0% | ||
| Immature granulocytes | 2.10% |
Table 1: A full blood count and differential count.
Laboratory testing
Peripheral blood smear
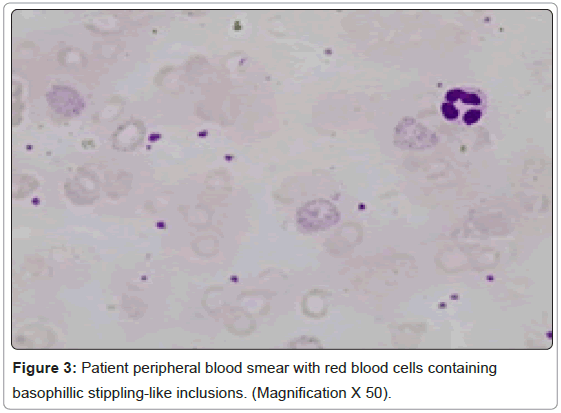
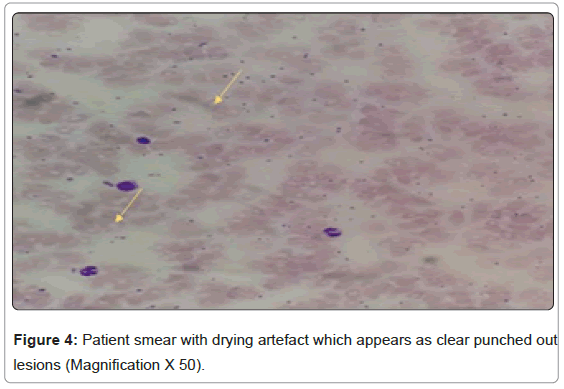
Of note on the peripheral blood smear were numerous basophilic stippling like inclusions which were identified as basophilic stippling initially in a background of a drying artefact. My concern was the numerous red cell inclusions (Figure 3). At this stage the results for the B12 and folate levels became available and showed no deficiencies in the two vitamins. Other possible causes of BS were entertained at this point and the clinicians were advised on further investigations. A decision was eventually made to repeat the peripheral blood smear (Figure 4).
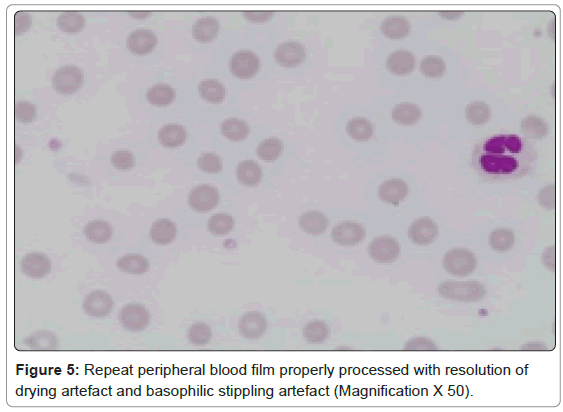
The peripheral blood smear was repeated and the correct procedure was followed in the preparation and processing of the smear and showed resolution of both the drying artefact and the basophilic stippling artifact (Figure 5).
Other tests and results relevant to the case were:
1. Coombs test: Negative (repeated twice)
2. LDH: 231
3. Haptoglobin: 0.15 g/L
4. Ferritin 1684
5. Antibody screen: Negative
6. Complement screen: Negative
7. PNH screen: Negative
8. TSH: Normal
9. Creatinine 231
10. Absolute reticulocyte count: Slightly elevated
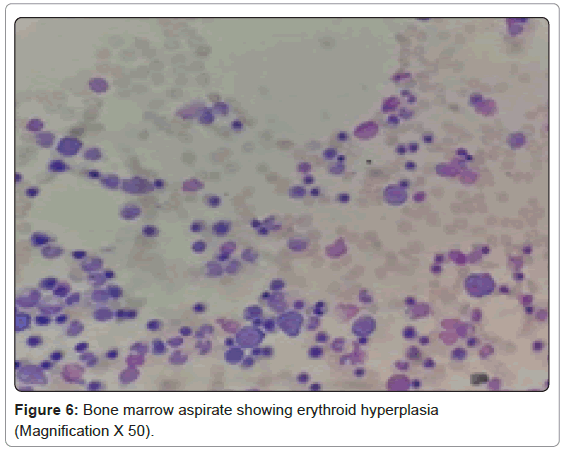
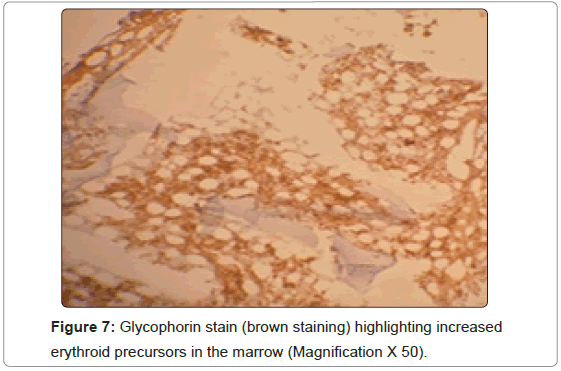
11. Bone marrow biopsy: hyper cellular with erythroid hyperplasia and dysplasia in the erythroid and granulocytic series (Figures 6 and 7).
12. Cytogenetics showed a normal female karyotype.
Bone marrow biopsy
A PAS (Periodic Acid Schiff) stain was also performed and showed fine granular staining on erythroid precursors. Normal erythroid cells are PAS negative. Positivity is seen in disease states such erythroleukemias, acute lymphoblastic leukemias, thalassaemias, certain lymphomas etc.
A diagnosis of MDS with multilineage dysplasia with possible underlying low grade hemolysis was made. The patient is managed by the clinical hematologists.
Discussion
Artefacts on peripheral blood smears may come from improper processing of smears and can be mistaken for real pathology. The BS artefact was caused by improper drying of the smear before staining it. Drying artefact is recognised in red blood cells as round to crescent shaped punched out regions or refractile vacuole like structures.
Basophillic stippling artefact results when the eosin component of the stain precipitates around red blood cell areas that are inadequately dried, this could also cause other artefacts that could be mistaken for erythroparasites or other cytoplasmic inclusions [6].
As blood smear assessment in a patient investigated for a haematological problem forms a fundamental step in overall patient health assessment, laboratory work up of a case to exclude pathology requires adherence to standard operating procedures (SOPs) in order to produce reliable and accurate results. Non adherence to SOPs can produce erroneous results with can lead to misdiagnosis and improper treatment of patients [7-10].
Conclusion
Improper processing of smears leads to a waste of resources and the wrong diagnosis can have a negative impact on patient management. This case was a learning curve for technologists, technicians and registrars in my laboratory and validated the fact that Standard Operating Procedures (SOPs) should always be adhered to by the laboratory staff to yield accurate and reliable results. It was the first time to see basophilic stippling occurring as an artefact and it is not mentioned in any of the major haematology textbooks.
Declarations
Ethics approval and consent to participate: Granted by the University of Cape Town Medical Research Council.
Consent for publication: Obtained.
Availability of data and materials: National Health Laboratory Services, Laboratory Information System (LIS).
Competing interests: None.
Funding: None.
Author Contributions: None.
Acknowledgements
Siphendulwe Matolweni, my daughter for assisting me with certain aspects of this article. She is a BSc student at Stellenbosch University Cape Town.
References
- Bain J B, Bates I, Laffan MA (2017) Dacie and Lewis Practical Haemalology. Chapter 4 (12th edn) Elsevier LTD.
- Knollmann-Ritschel BE, Markowitz M (2017) Lead Poisoning. Acad Pathol 4: 1-3.
- Chan NCN, Chan KP (2017). Coarse basophilic stippling in lead poisoning. Blood 129: 3270.
- Vander Meeren S, Van Damme A, Jochmans K (2015) Prominent basophilic stippling andhemochromatosis in glucose-6-phosphate dehydrogenase deficiency. Int J Hematol 101: 112-113.
- Bain BJ (2006) Blood Cells: A Practical Guide. Chapter 3 (4th edn) Blackwell Publishing.
- Walker D (2016) Veterian Key: Fastest Veterinary Medicine Insight Engine. Chapter 26. Peripheral Blood Smears.
- Green R, Mitra AD (2017) Megaloblastic anemias: Nutritional and other causes. Med Clin 101: 297-317.
- Potter K, Wu J, Lauzon J, Ho J (2017) Beta cell function and clinical course in three siblings with thiamine-responsive megaloblastic anemia (TRMA) treated with thiamine supplementation. J Pediatr Endocrinol Metab 30: 241-246.
- Goel S, Gajendra S, Sahni T, Jha B, Dang M, et al. (2017) Role of NEUT-X & NEUT-Y in picking up megaloblastic anaemia on peripheral blood & in differentiating from other macrocytic anaemia. Indian J Med Res 145: 395.
- Ashrafulla MR, Lodhi MI, Kuknoor GR, Katakol S (2017) A rare case of Diphyllobothriasis and Megaloblastic anaemia in a middle-aged lady from South India. Indian J Mircrobiol Res 4: 471-472.
Citation: Ntobongwana M (2019) A Staining Artefact Presumed to be Pathology in a Patient Investigated for Megaloblastic Anaemia and Myelodysplastic Syndrome: A Case Study at Groote Schuur Hospital. Diagn Pathol Open 4: 156. DOI: 10.4172/2476-2024.1000156
Copyright: © 2019 Ntobongwana M. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.
Share This Article
Open Access Journals
Article Tools
Article Usage
- Total views: 3679
- [From(publication date): 0-2019 - Apr 02, 2025]
- Breakdown by view type
- HTML page views: 2941
- PDF downloads: 738