Perspective Article Open Access
A Sociobiological Model of Early Childhood Caries: The Role of Allostatic Load
Leah Z. FitzGerald*1, Nar Gulvartian1, Francisco J. Ramos-Gomez2 and Brian Prestwich31Nursing Department, Mount Saint Mary’s University, Los Angeles, California, USA
2School of Dentistry, University of California Los Angeles, Los Angeles, California, USA
3Geffen School of Medicine at University of California Los Angeles, Los Angeles, CA, USA
- *Corresponding Author:
- Leah Fitzgerald
Mount Saint Mary’s University
Los Angeles, CA, USA
Tel: 2134772500
E-mail: lfitzgerald@msmu.edu
Received date: June 03, 2017; Accepted date: June 13, 2017; Published date: June 20, 2017
Citation: FitzGerald LZ, Gulvartian N, Ramos-Gomez FJ, Prestwich B (2017) A Sociobiological Model of Early Childhood Caries: The Role of Allostatic Load. Pediatr Dent Care 2: 138. doi: 10.4172/2573-444X.1000138
Copyright: © 2017 FitzGerald LZ, et al. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.
Visit for more related articles at Neonatal and Pediatric Medicine
Abstract
Abstract Objective: Even though many factors have been linked to increased ECC risk, few studies have specifically presented this information as a single comprehensive model. The purpose of this paper is to review the scope and usefulness of the proposed conceptual model in guiding future research of ECC risk as it relates to allostatic load. Methods: The various social, behavioural, and biological risk factors that emerge from the cumulative effects of chronic stress, defined as allostatic load, are discussed separately before being incorporated into a single sociobiological model of ECC. Results: In addition to biological realities, children experience profound impacts from their environments and family circumstances. The risk of developing ECC is especially pronounced in socially disadvantaged contexts. This information, as it is presented in the proposed conceptual model, reveals unique allostatic factors that work to increase risk at the level of the individual child, family, community, and society. Giving clinicians an idea of these realities has the capacity to more effectively screen and risk stratify children on the basis of dental health in the hopes of ultimately increasing their overall health as well. Conclusion: The proposed model provides a conceptual framework that relates factors of allostatic load to increased ECC risk. It demonstrates that a population-based, interprofessional collaboration strategy is essential to delivering effective prevention and treatment modalities to at-risk children. Future research regarding translational strategies has the capacity to reduce the prevalence of the biological, developmental, and psychosocial risk factors and thus ECC as a whole.
Keywords
Early childhood caries; Allostatic load; Conceptual model; Stress; Sociobiological model
Introduction
Early childhood caries (ECC) is the most common chronic disease among children. In fact, it is five times more common than asthma. From a physiologic standpoint, the main cariogenic bacteria, Streptoccocus mutans (S. mutans), produces acids in the mouth that could lead to the early demineralization of dental enamel characteristic of ECC [1]. When left untreated, ECC can result in malnutrition, childhood speech problems, and low self-esteem. It is also often associated with increased risk of diabetes, cardiovascular disease, and premature births. The reality remains that conceptual models regarding the development of caries focus on only a limited number of contributing variables. Many studies have identified gender, ethnicity, and socioeconomic status (SES) as additional risk factors for ECC [2]. Therefore, a comprehensive model regarding the causes and consequences of ECC is important to developing treatment modalities and reducing the prevalence of these longer-term complications.
Oral health is subject to both social and behavioral stressors that have the capacity to increase the biological risk of developing ECC. For example, prevalence is especially high among individuals who lack access to dental care, affecting up to 50% of low-income children [3]. For this reason, the etiologic model of ECC proposed in this manuscript includes an exploration of allostatic load as a potential source of higher risk.
Allostasis is described as the active process by which the body makes changes to homeostatic parameters in response to daily events and stressors [4]. Deviations from these parameters occur as an adaptation to stress. The cumulative physiologic toll of these repeated attempts at stress adaptation is referred to as allostatic load, which can have pathogenic effects on the body’s regulatory systems. The hypothalamicpituitary- adrenal (HPA) axis is a major regulatory system that is subject to the effects of allostatic load. Exposure to stress activates the HPA axis, which in turn leads to elevated levels of glucocorticoids [4]. Chronically high levels of these hormones damage tissues and potentially give rise to adrenal axis adaptations. By modifying adrenal hormone response or function, these adaptations shield the body from excessive glucocorticoid exposure. While initially protective, these early-life alterations in adrenocorticoid production may compromise the ability of the organism to adequately modulate stress later in life. The resulting changes in the adrenocorticoid phenotype, often described as an increase in HPA axis activity, predisposes infants and young children to compromised functioning, homeostatic dysregulation, and/or disease throughout their lives [4,5].
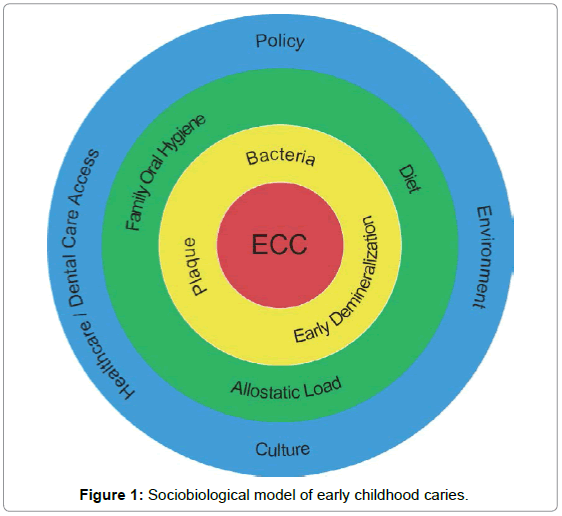
The purpose of this paper is to review the scope, usefulness and applications of the proposed conceptual model in guiding future research of ECC risk as it relates to allostatic load. The proposed sociobiological model of ECC includes, as its primary component, an altered responsiveness to physical or socio-behavioral perturbation of homeostasis that results from the cumulative effects of chronic stress (allostatic load). This altered output may manifest in the form of inadequate behavioral response during acute or chronic stress resulting in poor oral health and early childhood caries.
The Possible Role of Allostasis in ECC
Allostasis is the adaptive process by which the body changes the levels of one or more regulated parameters in order to adjust to new or changing environments. The steady state required for successful adaptation is maintained by an extraordinary repertoire of physical reactions that attempt to counteract the effects of stressors [6]. As part of this homeostatic regulation process, purposeful responses work together to defend bodily parameters critical to an individual’s wellbeing [7].
However, this process is not entirely foolproof. Maladaptive pathophysiology, in the form of allostatic load, can result in vulnerability to new disease or exacerbation of existing disease. Allostatic load may be due to frequent activation, failure to shut-off allostatic activity after stress, or inadequate response of allostatic systems leading to elevated activity of other, normally counter-regulated systems due to stress [4].
Conditions leading to allostatic load include (1) repeated exposure to multiple novel stressors, (2) prolonged response due to delayed shut down (3) inadequate response often leading to compensatory hyperactivity of other mediators, and/or (4) lack of adaptation altogether [4]. Chronic exposure to these factors has the potential to alter the body’s regulatory systems, which in turn increases susceptibility to the negative effects of stresses, including food insecurity, domestic and neighborhood violence, inadequate housing, and unemployment [8,9]. This is especially true in individuals who are at higher risk due to genetic predisposition or stressful early-life events as well [4].
Among predisposed individuals, exposure to both biological and social stressors early in life, in addition to a possible familial contribution, can result in enhancement of the stress response [4]. This in turn increases vulnerability to developing early demineralization of dental enamel and ultimately ECC. Numerous studies have suggested a correlation between the onset or exacerbation of ECC symptoms and exposure to SES-related risk factors, such as household education, financial situation, salivary cortisol secretion, and number of oral cariogenic bacteria [10]. For example, a history of health disparities during childhood has shown to contribute to increased likelihood of developing ECC. These disparities are also present more frequently in patients who already have ECC than in patients with a less prevalent form of caries. This in turn appears to be associated with an increased risk of developing ECC.
Data from a recent National Survey for Child Health reported that undergoing even one adverse childhood event increases the likelihood of having poor dental health in adulthood. Additionally, having multiple adverse childhood events had a cumulative negative effect on the condition of teeth and the presence of dental caries [11]. Risk increases more with each additional adverse childhood event.
Life stress
Early pre- and postnatal experiences have the potential to alter the responsiveness of the sympathetic and parasympathetic components of the autonomic nervous system (ANS) and hence the HPA axis [4]. Studies investigating the effects of prenatal stress have been performed in rodents and humans and provide evidence that exposure to social stresses during pregnancy has detrimental effects on the pregnancy as well as the offspring [12].
Research suggests that adverse early-life events, including maternal exposure to stress during pregnancy may result in persistent changes in physiological systems and behaviors likely via epigenetic mechanisms [13]. Prenatal stress experienced by the mother increases the production of maternal immune factors (cytokines) and endocrine factors (corticotropin-releasing hormone, adrenocorticotropic hormone, and cortisol) [14]. Findings support the hypothesis that exposure to physical or psychological stress during pregnancy in women can adversely affect their offspring as well. Increased level of these physiologic factors predispose infants to reduced neurocognitive function and developmental delays that manifest in modified regulatory systems in the fetus [14]. These changes have the capacity to ultimately increase the likelihood of developing ECC.
Biological stressors
The organism’s response to stress is generated by a network composed of integrative brain structures [4]. Changes in central stress circuits procured by aversive life events or traumatic stress can be seen as long-term alterations in frontal-limbic connections that ultimately affect feedback to the central nervous system. It is known that certain brain structures, including the ralphe nuclei and the locus coeruleus, play important roles in modulating the stress response [15]. Further, regions of the amygdala are involved in anticipation of negative events. Chronic anticipation of negative events leads to allostatic load, known as arousal pathology, which is signified by the release of CRF and glucocorticoids.
Physiological stress mediators are associated with both adaptation and pathophysiology. Both cortisol and catecholamines mediate the adaptation response of many systems of the body to acute challenges, while, at the same time, these same mediators also participate in pathological changes over long periods of time ranging from immunosuppression, hypertension, obesity, atherosclerosis and possibly ECC. Stress mediators also vary in their basal secretion according to the diurnal rhythm that is coordinated by the light-dark cycle and sleep-wake patterns. Perturbations in this pattern are also linked to pathophysiological outcomes. Nevertheless, it has been shown that the subjective experience of stress does not always predict the elevation of the physiological stress mediators, particularly cortisol and catecholamines [16].
Genetic and familial predisposition
Vulnerability to stress and disease is influenced not only by early-life stress but genetic factors as well [17]. High concordance and heritability between monozygotic and dizygotic twins demonstrates a genetic component in developing ECC [18]. Furthermore, genomic studies have identified genes that confer differences in saliva composition, diet preferences, and host immune responses that increase the susceptibility to dental enamel demineralization [19]. For this reason, dental caries has been shown to aggregate in families.
Familial predisposition may also contribute to the development of ECC, with decay being more common in children whose primary caretakers are carriers of mutans streptococci. Studies have shown that mutans streptococci is transmitted between mother and child primarily by vertical transmission and thus is a major risk factor in early and future caries ECC with similar bacterial genotypes being common within a family [20]. Whether the familial associations are due to exposures in a shared environment, parental culture, awareness (health literacy), familial (genetic) factors or whether this liability is related to the disorder itself remains to be determined. Furthermore, evidence supports a link between caregivers’ health literacy and use of oral health services, a reality that ultimately affects their children’s health [21]. Together, these data suggest that familial predisposition may contribute to the development of ECC in many patients. Therefore, understanding the genetic and/or familial basis of caries has the potential to provide clinicians with an additional dimension to screen for when identifying susceptible individuals, who require immediate attention.
Social stressors
Sustaining socio-behavioral and biological stressors plays a causal role in triggering and/or exacerbating ECC perpetuation [11,21,22]. In predisposed children, SES-related social stressors such as food insecurity, exposure to domestic or neighborhood violence, inadequate day care, transportation, and maternal education level and associated dental health literacy all play a role in ECC exacerbation [11,21,22]. For example, findings have shown that food-insecure children are more likely to have inadequate nutritional outcomes and thus poorer general health [22]. Additionally, malnutrition or improper diet due to poverty may lead to poor dental health. This is partially due to the fact that sugary food options are more affordable and thus accessible to lowincome families [23]. The result is an increased risk of dental enamel erosion early in life.
Income is associated with striking disparities in dental disease as well. Of fourteen million American children, one out of four is born into poverty, living below the poverty line (annual income of $22.050 for a family of four) and experiencing more severe and untreated tooth decay. Poor children suffer from dental caries twice as much as their more affluent peers. The disparities associated with income are further exemplified by the difference in the extent of untreated dental decay between rural and urban children [24]. Urban children were approximately three times as likely to show signs of dental caries when compared to their rural counterparts. This can be explained by the unique SES-related risk factors experienced by each group.
Behavioral stressors
In those that develop ECC, there has been a significant association between caries risk level, lack of fluoride, and dietary habits and ultimately the subsequent development of ECC. This suggests that certain behaviors and other causes of demineralization of dental enamel can precipitate ongoing ECC in addition to mutans streptococci infection. In this way, ECC has the potential to persist long after original bacterial exposure and infection. Studies have found an association between the frequency of sugar intake and caries whereas the total amount of sugar consumed has not been shown to be as predictive of caries [25]. Routine tooth brushing demonstrates few associations with caries status, but this behavior may counteract the negative outcomes resulting from a high-sugar diet [2]. Furthermore, certain high-risk behaviors, including not flossing, stress-inducing parenting styles, and inadequate coping strategies for stress, have the potential to worsen already existing demineralization of dental enamel. Therefore, developing ECC exists in a complex web of sociobehavioral factors in addition to the biological realities experienced by affected individuals.
Family and culture
Children from racial and ethnic minorities are more likely to be poor and to experience disparities in health outcomes and access to care. Immigrant families often face additional cultural, linguistic, and educational barriers to accessing healthcare and social services [26]. Community and cultural factors may be key drivers of oral health and ECC burden. In one multiethnic Los Angeles County neighborhood, there were ninety-two fast-food vendors in a four square mile areamany near schools. By contrast, grocery markets were mostly small stores, with few stocking fresh produce, and larger markets were not conveniently located for the population of this neighborhood. Geospatial mapping also revealed few parks and safe spaces for exercise and play in many low-income areas. Cultural dietary preferences as well as limited access to affordable healthy food and safe places to exercise are some of the community-level barriers children and families may face in trying to make healthy choices. These factors impact many health conditions including obesity, diabetes, and dental caries, all of which are more prevalent among lower socioeconomic groups [26].
Access to dental insurance
Dental disease among poorer children is more likely to be untreated due to a lack of access to dental care, with such disparities continuing into adolescence [27]. It has been reported that access to dental care is predicted by medical insurance. Uninsured children are two and a half times less likely than insured children to receive dental care and children from families without dental insurance are three times more likely to have dental needs that require attention than children with either public or private insurance. Similarly, not all health providers may be aware of the services needed to improve oral health, a reality that increases risk even when care is available [28]. Given these realities, lack of access to insurance has the capacity to amplify the negative outcomes associated with the biological, social, and behavior stressors and hence increases the risk of developing ECC.
The Affordable Care Act (ACA) mandates offering dental benefits to nearly 8.7 million children [29]. However, not all consumers are expected to purchase these benefits, and dental care utilization will not necessarily increase by the projected margin. If anything, the ACA has surely improved primary care coverage, whereas dental coverage remains limited. This gives primary care physicians a crucial role in screening, risk stratifying, and supporting self-care in primary care settings with utilization management to prioritize higher risk cases to occupy the limited capacity of dental chairs.
Implications for policy and practice
Given the prevalence of ECC among children who grow up in more adverse circumstances, access to early and periodic screening and intervention should be a priority for policy makers and clinicians committed to building healthy communities. Although dental coverage significantly limits access for these at-risk children, the ACA has resulted in expanded Medicaid and commercial medical coverage through state Health Exchanges. As long as this provision of the ACA is preserved, access to primary care for these vulnerable children will not be an issue. For example, in Los Angeles County it is estimated that 500,000 children have access to primary care but not to dental care [30]. Dentists, physicians, and nurses are now demonstrating that oral health screening, risk stratification, parent anticipatory guidance, and application of varnish can be integrated into the Well Child medical visit without disruption of work flow [31]. This collaborative interprofessional strategy is aligned with the provisions of the ACA and optimizes utilization management whereby higher risk kids are moved up in the cue for restorative dental care while lower risk kid’s oral health needs are met within the primary care practice between annual dental cleaning visits. Clearly there is a role for population-based strategies to screen defined populations of children in the primary care setting, risk stratify all children within registries, and improve the reliability of delivery of evidence-based oral health care to both low and higher risk children.
Parental attitudes towards oral health related behaviors do influence whether these behaviors are reported to occur in children and that the strength of attitudes varies between diverse ethnic groups and sites around the world [32]. Children experience profound impacts from their environment and family circumstances. Thus, for disadvantaged children, outreach is necessary to ensure they receive services, including dental care. Oral health advocates should partner with others in child and family advocacy to work towards the larger vision of family and community wellness, while ensuring oral health is integrated into these efforts. To succeed in alleviating health disparities, we must deliberately embrace new paradigms that emphasize 1) oral health as part of overall health at the level of the individual child, family, community, and society; 2) health promotion and wellness, not just absence of disease; 3) family and community empowerment as critical to improving children’s health and future lives; and 4) health professional efforts that include access to care but also reach beyond access to care to embrace a multifactorial model of health determinants [26], including oral health and its determinants.
In this paper, we have proposed a conceptual model of the role of allostatic load in promoting ECC (Figure 1). The most effective response on the part of both dental and medical professionals caring for children is a population-based interprofessional collaboration strategy which will create capacity for the reliable delivery of preventive and restorative care to defined populations of children in order to reduce the burden of preventable ECC among children in the US. This model provides a conceptual framework to support the work of change leaders in dentistry and primary care who are now demonstrating that quality improvement methods may be leveraged to accomplish this goal. More research should now be focused on the translational strategies which will most effectively contribute to a reduction in ECC and the medical, developmental, and psychosocial sequelae suffered by children who are affected.
References
- Featherstone JD (2008) Dental caries: a dynamic disease process. Aust Dent J 53: 286-291.
- Reisine S and Douglass JM (1998) Douglass, Psychosocial and behavioral issues in early childhood caries. Community Dent Oral Epidemiol 26: 32-44.
- http://www.cdc.gov/healthywater/hygiene/disease/dental_caries.html
- McEwen BS (2007) Physiology and neurobiology of stress and adaptation: central role of the brain. Physiol Rev 87: 873-904.
- Gunnar MR, Frenn K, Wewerka SS, Van Ryzin MJ (2009) Moderate versus severe early life stress: associations with stress reactivity and regulation in 10-12-year-old children. Psychoneuroendocrinology 34: 62-75.
- Johnson EO, Brady L, Gold PW, Chrousos GP (1996) Distribution of hippocampal mineralocorticoid and glucocorticoid receptor mRNA in a glucocorticoid resistant nonhuman primate. Steroids 61: 69-73.
- Sterling P (2014) Homeostasis vs allostasis: implications for brain function and mental disorders. JAMA Psychiatry 71: 1192-1193.
- Hilmers A, Hilmers DC, Dave J (2012) Neighborhood disparities in access to healthy foods and their effects on environmental justice. Am J Public Health 102: 1644-1654.
- Weitzman M (2013) Housing and child health. Curr Probl Pediatr Adolesc Health Care 43: 187-224.
- Boyce WT, Den Besten PK, Stamperdahl J, Zhan L, Jiang Y, et al. (2010) Social inequalities in childhood dental caries: the convergent roles of stress, bacteria and disadvantage. Soc Sci Med 71: 1644-1652.
- Bright MA, Alford SM, Hinojosa MS, Knapp C, Fernandez-Baca DE (2015) Adverse childhood experiences and dental health in children and adolescents. Community Dent Oral Epidemiol 43: 193-199.
- Brunton PJ (2013) Effects of maternal exposure to social stress during pregnancy: consequences for mother and offspring. Reproduction 146: R175-189.
- Meaney MJ, Szyf M, Seckl JR (2007) Epigenetic mechanisms of perinatal programming of hypothalamic-pituitary-adrenal function and health. Trends Mol Med 13: 269-277.
- Ruiz RJ, Avant KC (2005) Effects of maternal prenatal stress on infant outcomes: a synthesis of the literature. ANS Adv Nurs Sci 28: 345-355.
- Curtis AL, Pavcovich LA, Valentino RJ (1999) Long-term regulation of locus ceruleus sensitivity to corticotropin-releasing factor by swim stress. J Pharmacol Exp Ther 289: 1211-1219.
- Kudielka BM, Schmidt-Reinwald AK, Hellhammer DH, Schürmeyer T, Kirschbaum C (2000) Psychosocial stress and HPA functioning: no evidence for a reduced resilience in healthy elderly men. Stress 3: 229-240.
- Brinks V, van der Mark M, de Kloet R, Oitzl M (2007) Emotion and cognition in high and low stress sensitive mouse strains: a combined neuroendocrine and behavioral study in BALB/c and C57BL/6J mice. Front Behav Neurosci 1: 8.
- Bretz WA, Corby PM, Schork NJ, Robinson MT, Coelho M, et al. (2005) Longitudinal analysis of heritability for dental caries traits. J Dent Res 84: 1047-1051.
- Vieira AR, Marazita ML, Goldstein-McHenry T (2008) Genome-wide scan finds suggestive caries loci. J Dent Res 87: 435-439.
- HameĊ?-KocabaĊ? EE, Uçar F, KocataĊ? Ersin N, Uzel A, Alpöz AR (2008) Colonization and vertical transmission of Streptococcus mutans in Turkish children. Microbiol Res 163: 168-172.
- Lee JY , Divaris K, DeWalt DA, Baker AD, Gizlice Z, et al. (2014) Caregivers' health literacy and gaps in children's Medicaid enrollment: findings from the Carolina Oral Health Literacy Study. PLoS One 9: e110178.
- Chi DL, Masterson EE, Carle AC, Mancl LA, Coldwell SE (2014) Socioeconomic status, food security, and dental caries in US children: mediation analyses of data from the National Health and Nutrition Examination Survey, 2007-2008. Am J Public Health 104: 860-864.
- da Fonseca MA (2012) The effects of poverty on children's development and oral health. Pediatr Dent 34: 32-38.
- Maserejian NN, Tavares MA, Hayes C, Soncini JA, Trachtenberg FL (2008) Rural and urban disparities in caries prevalence in children with unmet dental needs: the New England Children's Amalgam Trial. J Public Health Dent 68: 7-13.
- Gussy MG, Waters EG, Walsh O, Kilpatrick NM (2006) Early childhood caries: current evidence for aetiology and prevention. J Paediatr Child Health 42: 37-43.
- Mouradian WE, Huebner CE, Ramos-Gomez F, Slavkin HC (2007) beyond access: the role of family and community in children's oral health. J Dent Educ 71: 619-631.
- Chankanka O, Cavanaugh JE, Levy SM, Marshall TA, Warren JJ, et al. (2011) Longitudinal associations between children's dental caries and risk factors. J Public Health Dent 71: 289-300.
- http://www.nidcr.nih.gov/DataStatistics/SurgeonGeneral/sgr/chap10.htm
- Nasseh K, Vujicic M (2013) Health reform in Massachusetts increased adult dental care use, particularly among the poor. Health Aff (Millwood) 32: 1639-1645.
- (2011) A Cities and Communities Health Report. Obesity
- Bahceci M, Gokalp D, Bahceci A, Tuzcu S, Atmaca S, et al. (2007) The correlation between adiposity and adiponectin, tumor necrosis factor?, interleukin-6 and high sensitivity C-reactive protein levels. Is adipocyte size associated with inflammation in adults? J Endocrinol Invest 3: 210-214.
- Adair PM, Pine CM, Burnside G, Nicoll AD, Gillett A, et al. (2004) Familial and cultural perceptions and beliefs of oral hygiene and dietary practices among ethnically and socio-economicall diverse groups. Community Dent Health 21:102-111.
Relevant Topics
- About the Journal
- Birth Complications
- Breastfeeding
- Bronchopulmonary Dysplasia
- Feeding Disorders
- Gestational diabetes
- Neonatal Anemia
- Neonatal Breastfeeding
- Neonatal Care
- Neonatal Disease
- Neonatal Drugs
- Neonatal Health
- Neonatal Infections
- Neonatal Intensive Care
- Neonatal Seizure
- Neonatal Sepsis
- Neonatal Stroke
- Newborn Jaundice
- Newborns Screening
- Premature Infants
- Sepsis in Neonatal
- Vaccines and Immunity for Newborns
Recommended Journals
Article Tools
Article Usage
- Total views: 4840
- [From(publication date):
specialissue-2017 - Apr 02, 2025] - Breakdown by view type
- HTML page views : 3835
- PDF downloads : 1005