A Simple Minimally Invasive Technique to Reduce the Size of Pneumatized Middle Turbinate (Concha Bullosa)
Received: 25-May-2016 / Accepted Date: 24-Jun-2016 / Published Date: 30-Jun-2016 DOI: 10.4172/2161-119X.1000242
Abstract
Pneumatized middle turbinate, concha bullosa, is a common anatomic variant. In the vast majority of cases it is asymptomatic. In some patients it may cause contact headache or secondary sinusitis. It may also hamper access to the middle meatus during endoscopic sinus surgery. In this paper we describe a simple minimally invasive turbinoplasty technique to reduce the size of concha bullosa. The technique was used in 42 patients. The patients were followed up for 12-18 months. The turbinates retained their reduced size and stability at the end of the follow up period. Also, we did not observe any mucocele formation or adhesions between the turbinates and the surrounding structures. The technique is best used when the air cells within the turbinates are large. Resective techniques, on the other hand, may be used when enlargement of the turbinates is due to hypertrophy of its tissues rather than the presence of air cells.
Keywords: Concha; Bullosa; Middle turbinate, Turbinoplasty
252097Introduction
Pneumatization of the middle turbinate is a common anatomic variant, which has been named “Concha Bullosa” by Zuckerkandl in 1893. Three types of middle turbinate pneumatization: lamellar, bulbous and extensive, have been described based on the site and extent of pneumatisation [1]. The reported incidence of concha bullosa varies between 14-53% in various studies [2]. In the vast majority of cases concha bullosa is asymptomatic. However, Excessive enlargement of the middle turbinate can result in contact headache [3] and narrowing of the drainage pathway of the anterior group of paranasal sinuses. It may also impair intraoperative endoscopic access to the osteomeatal complex.
Several techniques have been described for management of concha bullosa including some technically challenging turbinoplasty procedures [4]. We describe, herein, a simple non-technically demanding procedure to reduce the size of symptomatic pneumatized middle turbinates.
Materials and Methods
The procedure was performed on Forty-two patients (26 males and 16 females), with CT evidence of pneumatized middle turbinate, during the period from January 2012 and December 2014. The indications for surgery were chronic rhinosinusitis, contact headache, or as an initial step to provide access to the osteomeatal complex during endoscopic nasal surgery. Patients with allergic rhinitis and those who had previous surgeries were excluded from the study. Twenty patients had extensive type of pneumatization (combined lamellar and bulbous), 18 patients had bulbous type, and 4 patients had lamellar type. All patients completed a validated outcomes instrument (SNOT-22) [5] before surgery and at the end of the follow up period. IRB approval was obtained from the Committee of Medical Ethics and Research.
The patients received the routine postoperative care of nasal procedures The patients were followed up postoperatively on weekly basis for one month, monthly for 3 months, and then every 3 months for at least 12-18 months.
Surgical technique
The procedure was performed under general anesthesia. Seven patients, however, requested local anesthesia.
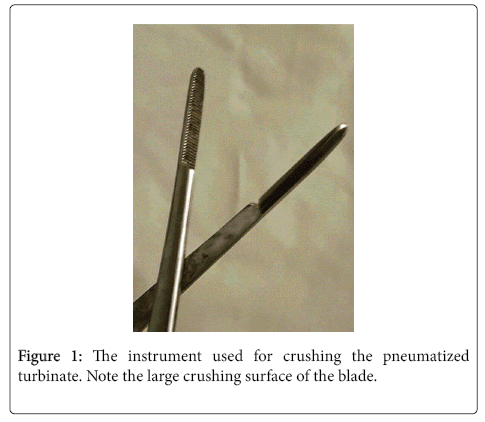
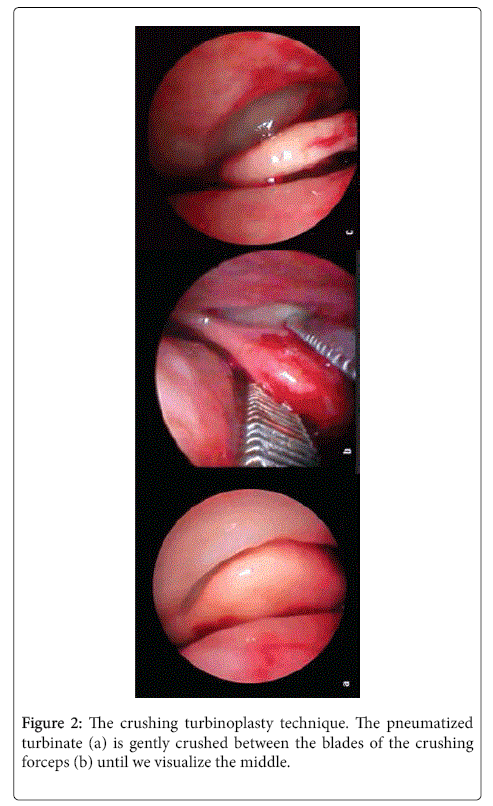
The enlarged pneumatized portion of the middle turbinate was gently crushed between the blades of Kressner turbinate crushing forceps (4 mm wide, 21 cm, InkaTM Surgical Instruments) that has a relatively large crushing surface area (Figure 1). The crushing was continued inferiorly and posteriorly until adequate visualization of the middle meatus was achieved and the middle turbinate is no longer in contact with the nasal septum (Figure 2).
Results
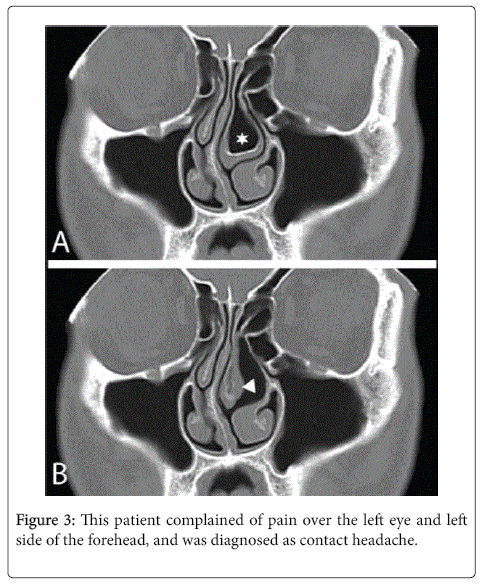
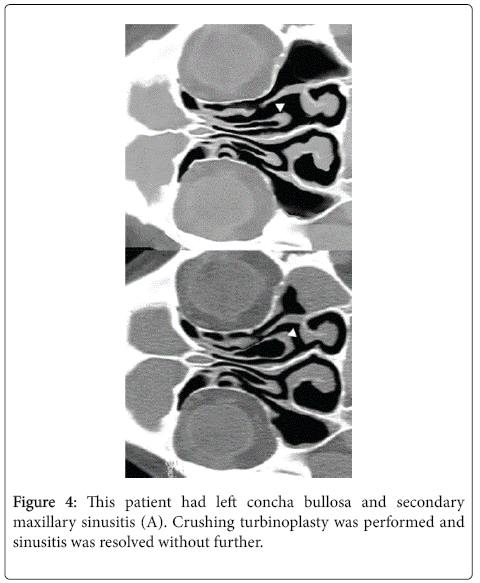
The present study included Forty-two patients (26 males and 16 females), with CT evidence of pneumatized middle turbinate, and who were underwent crusginf turbinoplasty. All crushed turbinates retained their postoperative size 12-18 months after surgery (Figures 3 and 4), and none of them developed mucocele or showed evidence of instability. Also, we did not recognize adhesions between the turbinates and the lateral nasal wall and/or the septum. The SNOT-22 tool was used to assess disease specific Quality Of Life (QOL) (Table 1). Snot-22 scores decreased significantly at the end of follow up period.
| Variable | Preoperative score | Postoperative Score | Significance (p) |
|---|---|---|---|
| SNOT-22 | 58 (5) | 21 (2) | 0.01* |
Table 1: SNOT-22 Quality of life score–Mean/SD, *Mann-Whitney U Test. Level of significance p<0.05.
Discussion
Pneumatized middle turbinates sometimes encroach upon the middle meatus, narrow the osteomeatal complex, hinder intraoperative endoscopic access to the middle meatus, and hamper postoperative control of the postoperative bed.
Excision of the lateral lamella of the concha bullosa, which is a commonly performed procedure, is associated with reported postoperative adhesions in 15% of patients especially if the procedure was combined with surgery of the paranasal sinuses [3]. In an attempt to decrease the rate of postoperative adhesions and improve the postoperative outcomes, several authors described more technically demanding procedures that were associated with a smaller incidence of postoperative adhesions.
None of our patients developed mucocele within the crushed turbinate. Mucocele is believed to develop secondary to osteal obstruction. In approximately 55% of cases the concha bullosa represents an extension of anterior ethmoid pneumatization and its ostium thus opens in the middle meatus. Posterior ethmoid air cells account for pneumatization of the remaining 45% which therefore drain into the superior meatus [6]. The ostium of the conchal cell is always present in the highest level of the cavity of the concha bullosa regardless the size and location of the conchal cell [5] This, apparently, shielded the ostium from traumatic injury during the crushing procedure.
In our series the turbinates retained their reduced postoperative size. We believe that crushing of the conchal walls results in microfractures that, upon healing, result into permanent remodeling of the turbinate to its new size and shape.
Excessive surgical manipulation of the concha bullosa in the form of dissection of its mucosa or bony lamella can potentially destabilize the middle turbinate. The described technique does not entail undue manipulations of the middle turbinate and was not associated with destabilization of the middle turbinate in any of our cases.
Conclusion
Our technique is a simple procedure that can result in predictable outcomes. The technique is not associated with the risk of destabilization of the middle turbinate, and does not increase the risk for mucocele formation within the middle turbinate. It also reduces the risk of postoperative adhesions. The technique is best used when the air cells within the turbinates are large. Resective techniques, on the other hand, may be used when enlargement of the turbinates is due to hypertrophy of its tissues rather than the presence of air cells.
References
- Hatipoğlu HG, Cetin MA, Yüksel E (2005) Concha bullosa types: Their relationship with sinusitis, ostiomeatal and frontal recess disease.DiagnIntervRadiol 11: 145-149.
- Stallman JS, Lobo JN, Som PM (2004) The incidence of concha bullosa and its relationship to nasal septal deviation and paranasal sinus disease.AJNR Am J Neuroradiol 25: 1613-1618.
- Shihada R, Luntz M (2012) A concha bullosamucopyocele manifesting as migraine headaches: A case report and literature review.Ear Nose Throat J 91: E16-18.
- Har-el G, Slavit DH (1996) Turbinoplasty for concha bullosa: A non-synechiae-forming alternative to middle turbinectomy.Rhinology 34: 54-56.
- Marambaia PP, Lima MG, Santos KP, Gomes Ade M, de Sousa MM, et al. (2013) Evaluation of the quality of life of patients with chronic rhinosinusitis by means of the SNOT-22 questionnaire.Braz J Otorhinolaryngol 79: 54-58.
- Doğru H, Döner F, Uygur K, Gedikli O, Cetin M (1999) Pneumatized inferior turbinate.Am J Otolaryngol 20: 139-141.
Citation: Mandour Z, Kalza R, Elwany S (2016) A Simple Minimally Invasive Technique to Reduce the Size of Pneumatized Middle Turbinate (Concha Bullosa). Otolaryngol (Sunnyvale) 6:242. DOI: 10.4172/2161-119X.1000242
Copyright: © 2016 Mandour Z, et al. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.
Share This Article
Recommended Journals
Open Access Journals
Article Tools
Article Usage
- Total views: 15351
- [From(publication date): 6-2016 - Apr 05, 2025]
- Breakdown by view type
- HTML page views: 14384
- PDF downloads: 967