A Severe Alkaline Gastritis in Type 1 Diabetes Gastroparesis: A Case Report
Received: 27-Jan-2017 / Accepted Date: 08-Dec-2017 / Published Date: 15-Dec-2017 DOI: 10.4172/2161-069X.1000540
Abstract
The incidence of Diabetes is increasing all over the world. In Brazil according to the Ministery of Health are expected 30,000,000 cases for 2030 meaning almost a 50% raise in incidence. This paper reports a case of a 32 years old type 1 diabetic female patient with Gastroparesis due to the disease. This patient had a severe abdominal pain and vomiting for 3 weeks. She had already diagnosed with diabetic gastroparesis and usually took metoclopramide and omeprazole. The patient underwent a gastroendoscopy revealing a severe alkaline gastritis due to a duodenum-gastric reflux.
Keywords: Diabetes; Gastroparesis; Alkaline gastritis
Introduction
Diabetes Mellitus is a disease facing an increasing incidence all over the world. According to the Brazilian Ministery of Health 30% of adult population is expected to have the diagnosis in 15 years from now [1]. Many authors linked gastrointestinal disorders with diabetes and the gastroparesis is one of the most frequent condition specially associated with type 1 diabetes as we show in this case-report. As a consequence the patient developed a severe alkaline gastritis caused by a duodenogastric bile reflux due to a gastric paresis.
Case Report
The case is about a 32 year female patient diagnosed with type 1 diabetes for 10 years. She used NPH Insulin regularly. She developed a gastrointestinal symptoms for 1 year most of it nausea, vomiting and abdominal distension. An abdominal X-ray was done e showed a severe gastric distension. A medical treatment was indicated with metoclopramide 30 mg a day orally associated with omperazol 40 mg a day.
She improved with the medical treatment and was able to have a nearly normal quality of life for some months. For 3 weeks’ time she started with severe abdominal pain, nausea and daily vomiting. She was medicated with omperazol, hyoscine and ondansetron intravenously but was not able to improve with the medication.
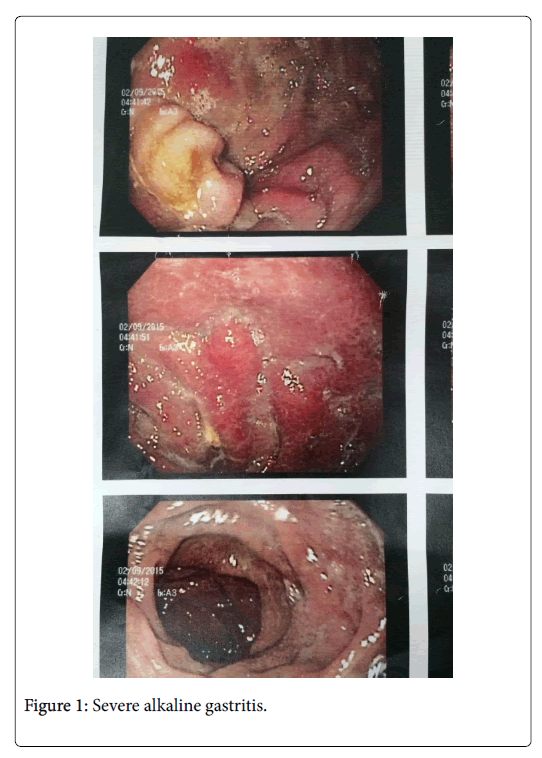
She was referred to the hospital and underwent a gastroendoscopy that revealed a severe alkaline gastritis with duodenogastric reflux as shows Figure 1. The patient stayed for 7 days in the hospital and needed an intravenous infusion of fluids and electrolytes associated with a medical treatment based on intravenous omeprazol, Ondansetron and oral eritomycin in order to improve the gastric motility. The treatment was well succeeded and she was discharged from the hospital with a few symptoms remaining.
Context
The references use to refer diabetic gastroparesis as a consequence of diabetic specially type 1 as we describe above.
Cipriani et al. says that cellular injury and development of delayed gastric emptying in diabetes requires the presence of muscle layer macrophages. Targeting macrophages may be an effective therapeutic option to prevent cellular damage and development of delayed gastric emptying in diabetes [2].
Halland at al. concludes that while acute severe and chronic hyperglycemia can delay gastric emptying, there is limited evidence that delayed gastric emptying is an independent risk factor for impaired glycemic control or hypoglycemia in diabetes. The impact of improved glycemic control on gastric emptying and vice versa in diabetes is unknown [3].
Tornblom at al. says the relationship between gastric emptying and postprandial glycaemia is complex and inter-dependent. Short-acting glucagon-like peptide-1 agonists, that slow gastric emptying, can be used to reduce postprandial glycaemic excursions and, in combination with basal insulin, result in substantial reductions in glycated haemoglobin in type 2 patients [4].
Zhao and cols shows that gastroparesis likely involves various pathophysiological disorders and is increasingly prevalent as complications of surgeries, medications, and chronic diabetes. Key to diagnosis is evidence of delayed gastric emptying, generally based on standardized scintigraphy, and ruling out distal obstruction or other dysmotilities. Initial medical management includes reviewing potentially exacerbating medications and ruling out other reversible causes, achieving tighter glucose control in diabetics, and implementing dietary and lifestyle changes.
Conclusion
The case shows a peculiar complication of a diabetic gastroparesis non demonstrated regularly by the medical literature and very rarely with the intensity seen in this case. An alkaline gastritis can occur as a consequence of the diabetic gastroparesis.
References
- Brazilian Society of Bariatric and Metabolic Surgery (2015) Incidence of diabetes in Brazil.
- Cipriani G, Gibbons SJ, Verhulst PJ, Choi KM, Eisenman ST, et al. (2016) Diabetic Csf1op/op mice lacking macrophages are protected against the development of delayed gastric emptying. Cell Mol Gastroenterol Hepatol 1: 40-47.
- Halland M, Bharucha AE (2015) Relationship between Control of Glycemia and Gastric Emptying Disturbances in Diabetes Mellitus. Clin Gastroenterol Hepatol 14: 929-936.
- Törnblom H (2015) Treatment of gastrointestinal autonomic neuropathy. Diabetologia 59: 409-413.
Citation: Weston A, Menguer R, Giordani D, Cereser C (2017) A Severe Alkaline Gastritis in Type 1 Diabetes Gastroparesis: A Case Report. J Gastrointest Dig Syst 7: 540. DOI: 10.4172/2161-069X.1000540
Copyright: © 2017 Weston A. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.
Share This Article
Recommended Journals
Open Access Journals
Article Tools
Article Usage
- Total views: 5696
- [From(publication date): 0-2017 - Apr 19, 2025]
- Breakdown by view type
- HTML page views: 4904
- PDF downloads: 792