Research Article Open Access
A Retrospective, Single Center, Observational Study, Comparing the Direct Cost of End-Of-Life Care Patients with Advanced Cancer Care: Palliative Care versus Usual Care
Sinsuwan W1*, Pairojkul S1, Gomutbutra P2, Kongkum K1 and Kosuwon W31Karunrak Palliative Care Unit, Faculty of Medicine, Khon Kaen University, Thailand
2Department of Family Medicine, Faculty of Medicine, Chiangmai University, Thailand
3Department of Orthopedics, Faculty of Medicine, Khon Kaen University, Thailand
- *Corresponding Author:
- Woraporn Sinsuwan
MD, Medical Oncologist
Palliative Care Unit, Faculty of Medicine
Khon Kaen University, Khon Kaen, Thailand
Tel: +6643466655
Fax: +6643466657
E-mail: doc.mil59@gmail.com
Received date: November 23, 2015; Accepted date: January 05, 2016; Published date: January 08, 2016
Citation: Sinsuwan W, Pairojkul S, Gomutbutra P, Kongkum K, Kosuwon W (2016) A Retrospective, Single Center, Observational Study, Comparing the Direct Cost of End-Of-Life Care Patients with Advanced Cancer Care: Palliative Care versus Usual Care. J Palliat Care Med 6:243. doi:10.4172/2165-7386.1000243
Copyright: © 2016 Sinsuwan W, et al. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.
Visit for more related articles at Journal of Palliative Care & Medicine
Abstract
Background: Palliative care focuses on relieving and preventing the suffering of terminal ill patients. There are evidences from western countries of approved benefit of hospital palliative care consultation. They have been shown that it improves quality of care and associates with hospital cost savings. Objectives: We examined whether elected palliative care was associated with any significant cost differences for the hospital. Methods: We performed single institution (Srinagarind Hospital, Northeast Thailand), retrospective (between October 1, 2011 and September 30, 2012), observational, direct cost analysis. The sample included 52 (29.4%) hospitalized patients receiving palliative care and 125 (70.6%) under usual care. Three advanced types of cancers were included: hepatocellular carcinoma, cholangiocarcinoma and lung cancer. We adjusted cost with Diagnosis- Related Group (DRG), age, sex, length of hospital stay and comorbidity score and then compared the direct cost per admission. Results: There was no difference in the overall demographic data between the two study groups. Whilst palliative care patients with hepatocellular carcinoma undergone endotracheal intubation significantly less often (P=0.025) than usual care patients and less likely to be admitted to ICU (P=0.001). Palliative care patients with lung cancer were also most unlikely to be intubated (P<0.001) when compared to usual care patients. After adjusting for age, sex, length of hospital stay and the comorbidity scores, the adjusted net savings for the care of palliative patients was 16,669 baht per person (P=0.035) compared to usual care patients. Conclusion: The cost analysis of terminal ill patients demonstrated that hospital-based palliative care over against usual care had lower costs and utilized intensive care less.
Keywords
Cost comparison; Palliative; Curative; Hospital care
Introduction
Palliative care is an area of healthcare that focuses on relieving and preventing the suffering of terminal ill patients. The goal is to improve the quality of life for both the patient and the family as they are the central system for care. Palliative care specialists found that approximately 50% of adult deaths occurred in hospital and most of these patients did not received adequate symptom control and treatment [1,2].
The Palliative Care Service (PCS) at Srinagarind Hospital comprises an interdisciplinary consultation team of physicians, nurses, rehabilitation specialists, pharmacists, nutritionists, social workers and volunteered religious ministers. Between October 1, 2011 and September 30, 2012, the team provided more than 300 consultations for both cancer (82%) and non-cancer cases (18%). The service operated an inpatient consultation available to any inpatient and worked closely with many local hospitals. Services provided are primarily available upon request by the patient’s primary care physician. The team aims to provide: (a) relief from suffering; (b) improved quality of life for the patient with advanced terminal illness (and his/her family/caregivers); (c) pain and symptom management; (d) facilitated, patient-centered communication and decision-making; and, (e) coordinated care across settings through the disease to the end of life.
Despite these potential benefits, a major issue for health care system is whether or not this hospital-based palliative care teams can provide resource saving that will justify their costs. Many studies suggest that palliative care team may reduce hospital expenditures [3-11]. A report in Thailand showed that the hospital expenditures in the last year of life was approximately one-third of total health expenditure. The expenditure in the last admission, averaged 30 days before death, accounted for two-third of the last year expenditures [12].
In this study, we examined whether palliative care offered as a choice, was associated to any difference in the direct costs borne by the hospital. It was not a direct outcome but could be used as supporting evidence for discussion in the debate on what costs could meaningfully be borne by universal healthcare and how the public could be guided in the consideration of their end-of-life care.
Materials and Methods
Study design and population
We conducted a retrospective, observational direct cost analysis, single institution (Srinagarind Hospital, Thailand) from October 1, 2011 through September 30, 2012. The study site is a medical school in Northeast Thailand.
The sample included all of our latest patients aged 18 years and over admitted to the hospital during the study period with a diagnosis of advanced disease with ICD-10 codes: (1) Hepatocellular carcinoma (HCC), (2) Cholangiocarcinoma (CCA), and (3) Lung cancer; as these cancers are the three most common cancers presenting in our hospital. We used the Elixhauser algorithm to determine the comorbidity score [13]. No curative treatment (i.e. chemotherapy, definite radiation therapy and definite surgery treatment) was given to these patients. The palliative performance scale was not more than 30%, indicating end-of-life [14]. The duration of hospital stay was, therefore, not expected to be more than 30 days. The direct costs of patient’s last admission during study period were estimated. ‘Usual care’ is defined as that from a primary care physician without palliative care involvement. The reasons for a palliative care consultation depended on the decision and preference of the primary care physician.
The clinical data were reviewed from OPD and IPD records by the researcher (WS). We obtained administrative data, DRG, and direct costs of each hospital stay from the administrative department and financial records office of the hospital. The data used to calculate the direct cost of palliative care were obtained from the Dean’s Office, the Financial Records Office and the Division of Building and Facilities.
Costs
The DRG version 5.0 software classifies hospital cases into one of several specified groups before estimating direct costs (those attributable to medications, procedure or services). Currently, the Thai healthcare system does not recognize direct costs for palliative care services; so we initiated a calculation of our service costs using our hospital and palliative care unit data.
Palliative care’s direct costs were estimated from labor, capital and material costs. The calculated labor cost was the sum of office workers (40 hours/week/person) and the cost of healthcare workers (45 hours/ week/person). Our service comprises daily visits by one palliative care physician and one palliative care nurse but does not include dedicated social worker or monks. A single weekly inpatient or home visit requires approximately 3 hours. Material costs include office supplies and utilities. Capitals costs include the building and durable goods (oxygenators, syringe drivers, computers and printers). We used straight line method to calculate depreciation (the building has an expected 20-year life and the durable goods 5 years) [15-17]. The final palliative care direct cost was presented on a per hour basis.
Analysis
The patient data were stratified by disease (hepatocellular carcinoma, cholangiocarcinoma, lung cancer). We obtained the following data for both groups of patients and examined for differences: patient age, sex (male), healthcare system (government reimbursement), principal diagnosis, services received, comorbidity score, length of hospital stay(s), days between consults and death, length of palliative care, status at discharge(s), ICU admission(s), endotracheal tube intubation, cardiopulmonary resuscitation (s), frequency of revisits and pain problems and control. We analysed the cost from the perspective of the care provider institution. The direct cost of production is an accounting cost, and indirect costs were not included.
Statistical analysis
The differences in demographic data were analyzed using the 2 and Mann-Whitney test as appropriate. The treatment data was assessed using the Fisher’s Exact test. A multivariable linear regression adjusted for diagnosis, age, sex, length of hospital stay and comorbidity score.
Results
The study population included 177 hospitalizations; comprising of 52 patients in the palliative care group and 125 in the usual care group. Patient demographics are presented in (Table 1). There were no differences between the two groups according to the distribution of male versus female, age grouping, comorbidity scores or status at discharge. Overall, the mean age was 60 years and mostly was men. More than 50% in each group had a discharge status ‘alive’ and among the patients with cholangiocarcinoma, those receiving palliative care were less frequently discharged alive than those getting usual care patients (P=0.024). On average, patients receiving palliative care received case management for a median of 4 days between consultations and/or discharge for all 3 diseases studied.
| Variable | Palliative care | Usual care | P value |
|---|---|---|---|
| Overall | |||
| Number | 52 | 125 | |
| Mean age (yr), (SD) | 59.12 (13.06) | 60.02 (11.89) | 0.68 |
| Male, n (%) | 40 (76.92%) | 93 (74.4%) | 0.72 |
| Comorbidities, mean (SD) | 19.13 (13.64) | 21.76 (13.75) | 0.24 |
| Discharge status alive, n (%) | 35 (67.30%) | 95 (76%) | 0.23 |
| Service | |||
| Acute care | 0 (0%) | 1 (0.8%) | |
| Internal medicine | 35 (67.30%) | 53 (42.4%) | |
| OB-GYN | 0 (%) | 2 (1.6%) | |
| Orthopedic | 1 (1.92%) | 4 (3.2%) | |
| RT | 0 (0%) | 3 (2.4%) | |
| Surgery | 16 (30.76%) | 62 (49.6%) | |
| Hepatocellular carcinoma (HCC) | |||
| Number | 19 | 69 | |
| Mean age (yr), (SD) | 54.6 (10.42) | 56.62 (11.45) | 0.50 |
| Male, n (%) | 16 (84.2%) | 58 (84%) | 0.98 |
| LOS hospital, median(range) day | 7 (1-16) | 6 (1-29) | 0.39 |
| Days between consult and discharge, median(range), day | 4 (1-9) | NA | |
| Discharge status alive, n (%) | 14 (73.68%) | 52 (75.36%) | 0.88 |
| Government reimbursement, n (%) | 12 (63.15%) | 27 (39.13%) | 0.06 |
| Cholangiocarcinoma (CCA) | |||
| Number | 19 | 37 | |
| Mean age (yr), (SD) | 58.89 (14.74) | 64.89 (10.46) | 0.08 |
| Male, n (%) | 12 (63.15%) | 20 (54.05%) | 0.51 |
| LOS hospital, median(range), day | 9 (1-27) | 5 (1-30) | 0.08 |
| Days between consult and discharge, median(range), day | 4 (1-23) | NA | |
| Discharge status alive, n (%) | 13 (68.42%) | 34 (91.89%) | 0.02 |
| Government reimbursement, n (%) | 14 (73.68%) | 20 (54.05%) | 0.15 |
| Lung cancer | |||
| Number | 14 | 19 | |
| Mean age (yr), (SD) | 65.43 (12.09) | 62.89(12.27) | 0.56 |
| Male, n (%) | 12 (85.71%) | 15 (78.94%) | 0.61 |
| LOS hospital, median(range), day | 14 (2-26) | 8 (2-21) | 0.08 |
| Days between consult and discharge, median(range), day | 4 (1-12) | NA | |
| Discharge status alive, n (%) | 8 (57.14%) | 9 (47.36%) | 0.57 |
| Government reimbursement, n (%) | 9 (64.28%) | 11 (57.89%) | 0.71 |
LOS: Length of Stay; NA: Nonapplicable; OB-GYN: Obstretric/Gynecology; SD: Standard Deviation; RT: Radiation Oncology; yr: Year.
Table 1: Base line characteristic and comparison of PCS and Usual care patients.
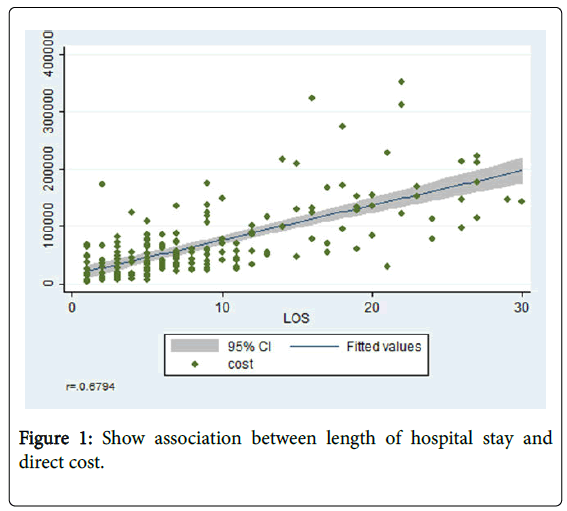
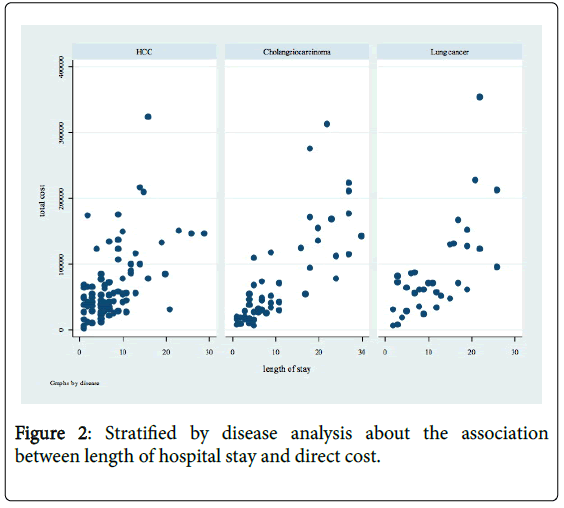
For treatment data (Table 2), hepatocellular carcinoma patients receiving palliative care underwent a less intensive procedures requiring endotracheal tube intubation (P=0.025) and were less likely to be admitted to ICU (P=0.001). Similarly, patients with lung cancer receiving palliative care undergone endotracheal intubation less frequently than usual care patients (P<0.001). Only one lung cancer patient was intubated and transferred to ICU after the palliative care team started their management. For all three types of terminal cancer Figure 1 shows Show association between length of hospital stay and direct cost. We found that longer length of stay resulted in higher cost (r=0.67), analysis by overall cases. The mean direct cost of overall cases is 71,527 Bath (SD=67,508). Figure 2 indicates Stratified by disease analysis about the association between length of hospital stay and direct cost.
| Palliative care | Usual care | P value | |
|---|---|---|---|
| Hepatocellular carcinoma (HCC) | |||
| ETT, n (%) | 2 (10.52%) | 27 (39.13%) | 0.02 |
| CPR, n (%) | 0 (0%) | 6 (8.69%) | 0.33 |
| ICU, n (%) | 0 (0%) | 26 (37.68%) | 0.001 |
| Readmission, n (%) | 0 (0%) | 7 (10.14%) | 0.33 |
| Pain score <3/Pain problem, n (%) | 5/5 (100%) | 8/15 (53.33%) | 0.11 |
| Cholangiocarcinoma (CCA) | |||
| ETT, n (%) | 3 (15.78%) | 14 (37.83%) | 0.12 |
| CPR, n (%) | 1 (5.26%) | 1 (2.70%) | 1 |
| ICU, n (%) | 0 (0%) | 7 (18.91%) | 0.08 |
| Readmission, n (%) | 0 (0%) | 4 (10.81%) | 0.28 |
| Pain score <3/Pain problem, n (%) | 3/4 (75%) | 6/6 (100%) | 0.4 |
| Lung cancer | |||
| ETT, n (%) | 5 (35.71%) | 19 (100%) | <0.001 |
| CPR, n (%) | 0 (0%) | 3 (15.78%) | 0.24 |
| ICU, n (%) | 5 (35.71%) | 9 (47.36%) | 0.72 |
| Readmission, n (%) | 0 (0%) | 1 (5.26%) | 1 |
| Pain score <3/Pain problem, n (%) | 4/5 (80%) | 4/6 (66.67%) | 1 |
ETT: Endotracheal Tube Intubation; CPR: Cardiopulmonary Resuscitation; ICU: Intensive Care Unit
Table 2: Treatment data.
HCC’s mean direct cost is 66,344 baht (SD=53,583). CCA’s mean direct cost is 69,382 Baht (SD=70,844). Lung cancer’s mean direct cost is 87,377 Baht (SD=71,956).
The adjusted direct costs per person for hospitalization of a palliative care patient with advanced cancer were significantly lower than the direct costs for hospitalizations for usual care patients (P=0.035). The putative cost savings was potentially 16,669 baht per person per admission (Table 4). Comorbidity scores (P=0.036) and length of stay (P<0.01) were correlated with a higher cost of hospitalization.
| Direct cost | Per 1 year (Baht) |
|---|---|
| 1. Labor cost | 1,389,333 |
| 2. Material cost | |
| Office supplies | 40,000 |
| Cost of utilities | 57,930 |
| 3. Capital cost | |
| Building | 39,375 |
| Durable goods | 18,000 |
| Total | 1,544,638 |
| Palliative care direct cost per hour (Baht) | 614.66 |
Table 3: Calculated of palliative care program direct cost.
| Variables | Estimated effect | P value | [95% Conf. Interval] | |
|---|---|---|---|---|
| Cost | ||||
| Palliative care | -16669.65 | 0.035 | -32183.55 | -1155.74 |
| Disease* | ||||
| CCA | -2807.52 | 0.75 | -20561.13 | 14946.07 |
| Lung cancer | 6328.24 | 0.55 | -14545.51 | 27202 |
| Age | -201.03 | 0.50 | -796.71 | 394.64 |
| Sex | 3140.98 | 0.70 | -13433.63 | 19715.61 |
| LOS | 6078.38 | <0.01 | 5048.42 | 7108.35 |
| Comorbidity scores | 601.25 | 0.036 | 39.94 | 1162.56 |
*Comparing with HCC
Table 4: Multivariate linear regression analysis.
Discussion
Srinagarind Hospital is the first medical school to implement an interdisciplinary team for palliative care of hospitalized terminal ill patients. After completing 2 years of consultations, the current report represents a retrospective analysis of direct costs of palliative care at Srinagarind Hospital, Khon Kaen, Thailand.
From the methodology about our direct cost analysis, we studied patients who had PPS<30%, which meant that this group of patients were terminal ill, so the cost of their last admission represented the cost before death. We found that all patients died after being discharged from the hospital except twelve patients in the usual care group who were readmitted to the emergency room. These readmissions were beyond the study period and all patients in this group died shortly. So the estimated cost saving for last admission before death was the aim of our study and palliative care service has shown to save about 16,600 Baht per person per admission in patients with advanced hepatocellular carcinoma, cholangiocarcinoma and lung cancer. One explanation was that palliative care team discussed the goal of care, improved communication among the patients and their families. This resulted in a reduction of treatment in the period leading to death such as invasive procedure of endotracheal tube intubation and in turns in ICU admission. Because of a good coordination of care between Srinakarind hospital and local hospitals, there were no readmissions of palliative care patient compared to twelve of usual care patients.
From the result of study, we found that length of stay were correlated with direct cost significantly (P<0.01). But between palliative care and usual care patients, the answer for non-significance of length of hospital stay could be explained by the palliative care being consulted too late especially in lung cancer that duration of palliative care management was only 28% of total length of stay (57% in HCC and 44% in CCA). Status discharge ‘alive’ was also non-significant in both HCC and lung cancer patients which may be explained by the preference of Thai people to die at home as shown from data in 2007. Before the palliative care started in Thailand, about 62% of Thai cancer patients died at home [12]. Therefore discharge status ‘alive’ from hospital should not be a good indicator for evaluating the efficacy of palliative care in Thailand. Nevertheless, our team has just started offering the service in our hospital so we have to accept that there are few primary physicians who really understand the concept of palliative care. Currently, primary physicians make a consultation earlier so we can expect more cost-saving from shorter length of hospital stay, shorter stay in intensive care unit, more support outside hospital, and lower emergency readmission. As supported by Figure 1, there was an association between length of hospital stay and direct cost.
Limitations
This was a retrospective, single center study and the results cannot be generalized. The data were reviewed by only one researcher. The available data limited the analysis of pain treatment. Other indicators (e.g. Patient’s quality of life and family satisfaction) were needed to measure the quality of care. The non-randomized nature of the comparison meant that cost differences could be the result of unobserved differences. For example, palliative care patients might have lower costs because at that stage the case was less complicated and there was little to be done. However, this research controlled for the sickness by measuring comorbidities.
Conclusion
In summary, in comparison with normal inpatient care of terminal ill patients, the palliative care service at Srinagarind Hospital met the medical needs with a conservative approach with special attention paid to adequate oxygenation, pain relief and psychosocial supports for the patient and family. An observational aspect was that our care was associated with a reduction in direct costs per person per admission. Further objective and comparative reports of palliative care are supported and needed.
Declarations
The authors are implementing palliative care for the first time ever at this institution. There is much political debate about medical costs so great care is needed in interpreting these results.
Acknowledgements
We thank the patients and the families, the palliative care nurses, the Faculty of Medicine at Khon Kaen University, the Oncology Unit in Internal Medicine, Chaisiri Angkurawaranon, MD, MSc.(Faculty of Family medicine, Chiang Mai University).
References
- Field MJ, Cassel CK (2011) Approaching death: improving care at the end of life. Heal Prog St Louis Mo 92: 25.
- (1998) Cancer care during the last phase of life. J Clin Oncol Off J Am Soc Clin Oncol 16: 1986-1996.
- Smith TJ, Coyne P, Cassel B, Penberthy L, Hopson A, et al. (2003) A high-volume specialist palliative care unit and team may reduce in-hospital end-of-life care costs. J Palliat Med 6: 699-705.
- Youngwerth JM, Bartley JB, Yamashita TE, Kutner JS (2011) Characteristics associated with higher cost per day or longer length of stay in hospitalized patients who died during the hospitalization or were discharged to hospice. J Hosp Med Off Publ Soc Hosp Med 6: 338-343.
- Hanson LC, Usher B, Spragens L, Bernard S (2008) Clinical and economic impact of palliative care consultation. J Pain Symptom Manage 35:340-346.
- Penrod JD, Deb P, Luhrs C, Dellenbaugh C, Zhu CW, et al. (2006) Cost and utilization outcomes of patients receiving hospital-based palliative care consultation. J Palliat Med 9: 855-860.
- Morrison RS, Penrod JD, Cassel JB, Caust-Ellenbogen M, Litke A, et al. (2008) Cost savings associated with US hospital palliative care consultation programs. Arch Intern Med 168: 1783-1790.
- Penrod JD, Deb P, Dellenbaugh C, Burgess JF, Zhu CW, et al. (2010) Hospital-based palliative care consultation: effects on hospital cost. J Palliat Med 13: 973-979.
- Back AL, Li Y-F, Sales AE (2005) Impact of palliative care case management on resource use by patients dying of cancer at a Veterans Affairs medical center. J Palliat Med 8: 26-35.
- Elsayem A, Swint K, Fisch MJ, Palmer JL, Reddy S, et al. (2008) Palliative care inpatient service in a comprehensive cancer center: clinical and financial outcomes. J Clin Oncol Off J Am Soc Clin Oncol 22: 2008-2014.
- Bruera E, Neumann CM, Gagnon B, Brenneis C, Quan H, et al. (2000) The impact of a regional palliative care program on the cost of palliative care delivery. J Palliat Med 3:181-186.
- https://ueaeprints.uea.ac.uk/id/eprint/32217.
- Elixhauser A, Steiner C, Harris DR, Coffey RM (1998) Comorbidity measures for use with administrative data. Med Care 36: 8-27.
- Anderson F, Downing GM, Hill J, Casorso L, Lerch N (1996) Palliative performance scale (PPS): a new tool. J Palliat Care 12: 5-11.
- Hospital WS, Charoensak S, Chantarujikapong S, Cherdsuwan S, Ontale K (2005) Unit Cost of Major Depressive Disorder in Psychiatric Ward, Siriraj Hospital. Siriraj Med J 57:178-181.
- http://kb.hsri.or.th/dspace/handle/11228/1963.
- http://kb.hsri.or.th/dspace/handle/11228/1330.
Relevant Topics
- Caregiver Support Programs
- End of Life Care
- End-of-Life Communication
- Ethics in Palliative
- Euthanasia
- Family Caregiver
- Geriatric Care
- Holistic Care
- Home Care
- Hospice Care
- Hospice Palliative Care
- Old Age Care
- Palliative Care
- Palliative Care and Euthanasia
- Palliative Care Drugs
- Palliative Care in Oncology
- Palliative Care Medications
- Palliative Care Nursing
- Palliative Medicare
- Palliative Neurology
- Palliative Oncology
- Palliative Psychology
- Palliative Sedation
- Palliative Surgery
- Palliative Treatment
- Pediatric Palliative Care
- Volunteer Palliative Care
Recommended Journals
- Journal of Cardiac and Pulmonary Rehabilitation
- Journal of Community & Public Health Nursing
- Journal of Community & Public Health Nursing
- Journal of Health Care and Prevention
- Journal of Health Care and Prevention
- Journal of Paediatric Medicine & Surgery
- Journal of Paediatric Medicine & Surgery
- Journal of Pain & Relief
- Palliative Care & Medicine
- Journal of Pain & Relief
- Journal of Pediatric Neurological Disorders
- Neonatal and Pediatric Medicine
- Neonatal and Pediatric Medicine
- Neuroscience and Psychiatry: Open Access
- OMICS Journal of Radiology
- The Psychiatrist: Clinical and Therapeutic Journal
Article Tools
Article Usage
- Total views: 11504
- [From(publication date):
January-2016 - Apr 02, 2025] - Breakdown by view type
- HTML page views : 10517
- PDF downloads : 987