A Retrospective Review of Ebola Outbreak in West Africa: Social Determinants and Control Measures
Received: 08-Nov-2018 / Accepted Date: 12-Nov-2018 / Published Date: 20-Nov-2018 DOI: 10.4172/2161-1165.1000360
Abstract
Ebola Viral Disease (EVD) is a fatal hemorrhagic disease of Public health importance caused by Ebola virus. It has only been recorded in low-income countries of sub-Saharan African countries, particularly in West Africa, where the poverty level is high and the environmental sanitation is very poor. The West African outbreak of this deadly disease has been described as the most complex outbreak pattern since its inception in 1976. It was declared a bioterrorism against West Africa at the time of its outbreak in 2014-2016 when over 27,000 people were infected. This retrospective study is a historical survey of the outbreak of EVD in West Africa between 2014 and 2016, the location and mapping of the first and subsequent outbreaks, the morbidity and mortality reports in the countries involved the Social determinants of EVD outbreak in the region and the recommended control/preventive measures. A literature search strategy was by translating two major terms (‘Ebola Outbreak’ and ‘Retrospective study’) to the controlled vocabulary of database. This was conducted using Google search machine, MEDLINE, Embase, AJOL, PubMed, Cochrane Database Systematic Review (CDSR) and WHO Ebola viral disease report database, with the aim of identifying relevant population-based studies with information on the prevalence and Case Fatality Rates of EVD in various locations in the West African regions.
EVD outbreak in Africa is a public health emergency and a threat to the global community. Therefore, proactive measures are required by the government and other international health donor agencies to curb this ravaging menace, not only in West African region, but globally. This is achievable by breaking the epidemiologic chains of the viral transmission and provision of prophylactic and therapeutic interventions to the target population in the Ebola virus high pressure zones.
Keywords: EVD; West Africa; Outbreak; Retrospective review; Social determinants
Introduction
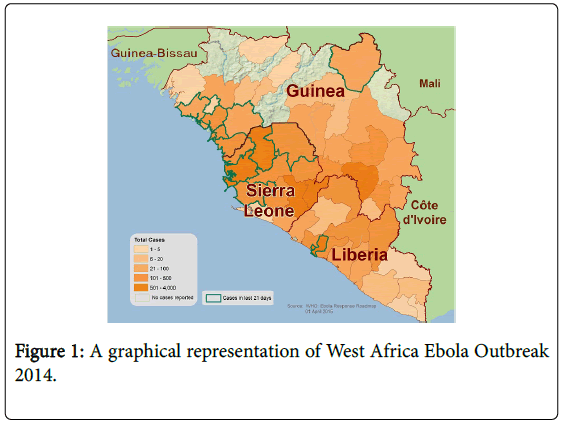
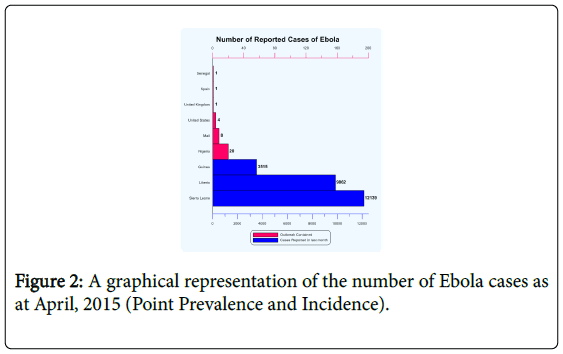
EVD is a severe and often fatal disease caused by one of the Ebola virus species. It causes diseases in humans and nonhuman primates such as monkeys, gorillas and chimpanzees. The disease is caused by negative sense single-stranded RNA virus classified by the International Committee on Taxonomy of Viruses as belonging to genus Ebola virus in the family of Filoviridae . These particles are 80 nm in diameter and form twisted filament of about 1.1 μm in length, hence the name. There are five identified species of Ebola virus, four of which caused disease in humans. They are Zaire ebolavirus , Sudan ebolavirus , Tai Forest (formerly Cote d’Ivoire ebolavirus ) and Bundibugyo ebolavirus . The fifth, Reston ebolavirus , has caused disease only in non human primates. EVD is a highly infectious, fatal organism with a case fatality rate approaching 90% in some outbreaks especially those that occurred in the Democratic Republic of Congo [1,2]. Based on the case fatality, members of the family of Filoviridae have been classified as Category A bioterrorism agents by Center for Disease Control and Prevention. The major reservoir in the transmission chain of Ebola virus is the fruit bat, specifically, Hypsignathus monstrosus (the hammer-headed fruit bat) and the Myonycterius torquata (the littlecollared fruit bat), which are reservoirs of the Zaire ebolavirus . EVD is therefore, a zoonotic disease. It may spread by direct contact with body fluids like blood, saliva, vomitus, sweat, stool, urine, semen and secretion from wounds of a person suffering from Ebola infection; contact with cloths or bed linen from a patient with Ebola infection; handling of infected chimpanzees, gorillas, bats and forest antelopes, both dead or alive; burial rituals of EVD victims, and use of unsterilized injections and other medical equipment. The West African Ebola outbreak was described as the largest, most complex outbreak of the disease since its inception in 1976 with multiple countries affected. At a time during the outbreak, it was almost declared as a bioterrorism against West Africa (and the world at large), leading to CDC activating its Emergency Operations Center to co-ordinate technical assistance and control activities, together with other agencies such as World Health Organization, domestic and international partners, to wage the war against EVD in the region. By the ending of March 2015, the World Health Organization (WHO) situation report showed a total of 27,401 and 10,194 confirmed cases and deaths respectively, giving a Case Fatality Rate of 37% (Figure 1 and 2). About two in every five confirmed cases died (average case fatality rate of 40%) [3]. On the 29th of March, 2016, WHO terminated the Public Health Emergency of International Concern (PHEIC) for Ebola outbreak in West Africa based on CDC certification of the countries with former widespread transmission of Ebola virus as free from the disease (based on 42 days of no active disease) (Table 1).
| Year | Country | Cases (n) | Deaths (n) | Case fatality (%) |
|---|---|---|---|---|
| 2014 | Gu/Li/SL/NGA/Sen/Ma | 27,401 | 10,194 | 40 |
| 2007-2008 | DRC | 296 | 201 | 68 |
| 2005 | DRC | 12 | 10 | 83 |
| 2003 | DRC | 178 | 157 | 88 |
| 2001-2002 | DRC and Gabon | 125 | 98 | 78 |
| 1996 | Gabon | 91 | 66 | 73 |
| 1995 | DRC | 315 | 254 | 81 |
| 1994 | Gabon | 52 | 31 | 60 |
| 1976-1977 | DRC | 319 | 281 | 88 |
Abbreviations: Gu- Guinea; Li- Liberia; SL- Sierra Leone; NGA- Nigeria; Sen- Senegal; Ma- Mali; DRC- Democratic Republic of Congo
Table 1: The Case fatality rate of Ebola outbreak from 1976-2016.
Location Mapping Of First Outbreak
The first communiqué issued by WHO on a new outbreak of EVD was on the 24th of March 2014, barely 7 days after the arrival of the disease in Conakry, the capital of Guinea. There were six countries affected by EVD in West Africa; the three significantly affected countries made up of Guinea, Liberia and Sierra Leone and the less significantly affected countries which were Nigeria, Senegal and Mali. The disease was presumed to have started in a village known as Meliandou in Gueckedou prefecture of eastern Guinea [4]. It was traced to a 2-year old boy who fell ill with a mysterious illness characterized by fever, black stool and vomiting, and he later died on the 6th of December, 2013. By February, 2014, it was transmitted to Macenta, a town about 80 km away from Gueckedou, then to Kissidougou (Late February), N’zerekore (March, 2014), Dabola (March, 2014), Conakry (March 17, 2014) and Watagala in Dinguuiraye Prefecture. Gueckedou was the initial outbreak location and it recorded the highest suspected cases of 122 as at April 22, 2014 with a case fatality rate of 71%. The first death in the capital city of Conakry was a business man who came from Dabola [5]. He became ill on the 17th of March 2014 and died the following day. It was believed that he contacted the virus from a visitor in Gueckedou who subsequently died of suspected EBV. However, eight more persons were infected when the corpse of the business man was conveyed from Conakry to his home town, Watagada in Guinea (Table 2). EVD was transmitted from Gueckedou through Foya, a village in Liberia at the boundary between the two countries. A woman arriving from guinea transmitted the virus to her sister, who then travelled to Monrovia (Liberia) capital to visit her husband in Firestone rubber plantation camp. However, she died on the 2nd of April, 2014. The appearance of the EVD in the two capital cities of the countries marked the first large urban setting of EVD transmission [6]. It was this emergence in the densely populated urban cities of Conakry (about 2 million) and Monrovia (about 1 million) that created a justifiable concern of greater risk ahead of possible spread to international air travel. It was at this stage that the international health organizations (CDC and WHO) swung into action. It was at this stage that travelling restrictions at the international borders, especially from the significantly affected countries, were instituted. Screening tests for passengers boarding airlines were scaled up at the airports’ immigration centers. However, these did not stop transmission of the virus.
| Year | Country | Cases (n) | Deaths (n) | Case fatality (%) |
|---|---|---|---|---|
| 2014 | Gu/Li/SL/NGA/Sen/Ma | 27,401 | 10,194 | 40 |
| 2007-2008 | DRC | 296 | 201 | 68 |
| 2005 | DRC | 12 | 10 | 83 |
| 2003 | DRC | 178 | 157 | 88 |
| 2001-2002 | DRC and Gabon | 125 | 98 | 78 |
| 1996 | Gabon | 91 | 66 | 73 |
| 1995 | DRC | 315 | 254 | 81 |
| 1994 | Gabon | 52 | 31 | 60 |
| 1976-1977 | DRC | 319 | 281 | 88 |
Abbreviations: Gu- Guinea; Li- Liberia; SL- Sierra Leone; NGA- Nigeria; Sen- Senegal; Ma- Mali; DRC- Democratic Republic of Congo
Table 2: Case fatality rates of major towns affected by EBOV in Guinea as at 20 April, 2014.
Nigeria Index Case
Nigeria was one of the less significantly affected countries by EVD. It has a population of I60 million people based on the 2006 Census population, with annual growth rate of three per cent per annum. The Nigerian index case was an imported one from the United States-based business man who had a brief stop-over at Monrovia, where he got infected. He arrived on board an aircraft from Liberia to Lagos city. The outbreak lasted for 92 days from the day it was reported (20th July, 2014) till the day the country was declared free from Ebola by WHO (20th October, 2014). Twenty cases (19 confirmed & 1 probable) with 1424 contacts linked to the index case were reported in two major cities in Nigeria – Lagos and Port Harcourt. Eight (7 confirmed and 1 probable) of them died, thereby giving an estimated case fatality rate of EVD in Nigeria as 40.0% [7].
Flare-ups of EVD 2015-2016
There have been flare-ups of EVD in three major countries namely Liberia, Sierra Leone and Guinea following the initial outbreak control of March 2015. About 33 new cases with 3453 contacts were established between March 2015 to June 2016. The flare-up was reported to be caused by possible sexual transmission and poor hygiene among the survivors of EVD [8]. It was speculated that Ebola virus can persist in some survivors for more than 18 months. Interventions put in place by WHO to curb this were infection prevention control, active case search, rapid diagnostic test to increase rate of post-mortem testing for Ebola in outbreaks and vaccination of people at risk.
Social Determinants of EBV Outbreak in West Africa
The population health is determined by the outcome of the interplay between the population and social environment. A social environment, as described by David Satcher, is the place where people are born, grow, live, work and age. The environmental factors could be favorable or unfavorable. A favorable interplay will give rise to good health indices (on the side of the population) while an adverse interplay will result into adverse health condition of the population. Depending on the health outcome, there are several environmental factors that could give rise to poor health indices in a population such as increase in cancer rate, cardiovascular disease, diabetes, chronic diseases, decrease lifespan and increase mortality rates. Examples of such unfavorable environmental factors include low socioeconomic status, discrimination, poverty, infectious agents, natural disaster, air pollution, toxic chemical, poor waste management, poor nutrition, poor sedentary lifestyle, poor accommodation/overcrowding and interpersonal violence just to mention but a few [9]. The favorable environmental factors include high social class, high per capita income, healthy diet, recreation activities, exercise, good hygiene, good accommodation, education, emergency preparedness, good disaster management and access to health care just to mention but a few. These social conditions together with the social policies that impact on the environment in which people live and develop constitute what is known as population health determinants. Health is not necessarily, therefore, something medical or something you fix to the doctor or availability of technology, medicine or high gross national product, rather, it is something that is rooted in our culture, social behaviors and how we allocate our resources and opportunities which will ultimately lead to improved quality of life. However, there are variations in the interplays that determine the health outcomes of a population from country to country. While the favorable social environmental interplay seem to dominate in the High-income (industrialized) countries, the unfavorable social factors tend to dominate in the low- income countries leading to good and bad health indices respectively. Although a combination of the two interplays may be found in both high- and low-income countries, these health disparities could occur by race, ethnicity, sex, socioeconomic status and sexual orientation. Health disparity is brought about by inequities and inequalities. Inequities literally mean lack of fairness and justice in allocation of resources, opportunities, treatments and successes. It is a preventable unfair difference. Inequality means getting what is unfair. It refers to health difference that is reducible but not preventable.
Bringing this down to EVD, most countries in West Africa are lowincome countries. The EVD is a zoonotic disease and therefore can also cause diseases in both humans and animals. The spread of infectious diseases occur through a chain of events that are connected (otherwise known as chain of infection). In traditional epidemiologic triad model (otherwise known as “epidemiologic triangle” or “chain of infection”), there are three vertices (corners) the epidemiologist is interested in. They are: the cause of the disease (the “what” of the triangle, otherwise known as the Ebola virus in this case), the host/reservoir or organism that harbors the disease (the “who” of the triangle, otherwise known as the fruit bat) and the Environment, or those external factors that cause or allow disease transmission (the “where” of the triangle). The unfavorable environmental health determinants in West Africa favor transmission and proliferation of infectious diseases and so EVD will likely thrive better in West Africa than in developed countries [10]. Environmental factors that are unfavorable to healthy living such as low socio-economic status, poverty, poor hygiene, unprotected sexual intercourse, improperly prepared food, consumption of bush meat, unhealthy living, unclean water, and uncleared bushes are contributory social determinants to EVD transmission and proliferation in West Africa.
The social model of health determinant depicts the wide range of multi-level factors that influence our health. EVD transmission can be transmitted by multi-level factors namely the virus, the reservoir, and the social environment. The epidemiologic triad model can be placed under the individual lifestyle factors, social and community network, and socioeconomic, cultural and environmental factors using the Dalghren and Whitehead model. This model can be used to bring modification to behavioral factors that will promote the transmission.
Recommendations of Possible Future Control Measures
The mission of the epidemiologist is to break the connectivity of the vertices of EVD transmission, hence, bringing a halt to the spread of diseases. This mechanism of epidemiology has enabled public health to bring about the desired positive changes in curbing the spread of diseases globally over the years. It is possible to defeat Ebola with domestic and international collaborative efforts. This was as typified in the collaborative efforts of the CDC and WHO in the curbing of Ebola outbreak in West Africa. This becomes more important when we do away with disparities, inequities and inequalities that create gaps among us. Although the epidemic is slowing down in West African, there is a need for individual country’s emergency response plan to be sustained and effort made to strengthen it [11]. There should be high level of surveillance of associated risk factors. The level of hygiene and sanitary practices should be at their peak. Subsequent response should incorporate psychological support and rehabilitation of families affected. Effort should be made to make the antiviral agent and vaccines available in all the vulnerable areas as part of emergency preparation strategy.
Every country in West Africa should set up a local Ebola Emergency Operations Center (EOC). The center should have response team to co-ordinate Ebola response. Their roles should include Epidemiology/ surveillance, Case Management/infection control, social mobilization, laboratory services and point of entry and management/coordination.
Before an outbreak, the team should establish a functional incidence management system and mobilize resources to facilitate emergency response through dissemination of National EVD Emergency Preparedness Plan. They should conduct high-level advocacy and engagement of with state institutions to ensure strong buy-in from all stakeholders. They should also provide technical support to states in term of strategy and technical support to strengthen EVD outbreak preparedness.
The surveillance team should ensure adequate staffing in line with the national infectious diseases surveillance guidelines. They should manage the collection and distribution of data and information to relevant stakeholders for decision-making and resource mobilization.
In case management, they should establish and maintain designated treatment facilities for management of the infection. They should collaborate with the commissioner of health to designate potential isolation facilities and treatment centers in strategic locations including the provision of ambulance and burial services.
The standard infection control precaution measure must be strictly adhered to. The use of Personal Protective Equipment while collection of specimen or handling the patient is mandatory. The three category transmission-based precautions include: contact, droplet and airborne precautions.
Environment control of possible reservoir such as the fruit bats has been advocated. The government has now banned the sale of bats for culinary purpose and prohibited weekly market where they are sold in some areas [12]. However, this recommendation is controversial as there is likelihood of increasing the number of bats available as viral vectors. It is strongly recommended that better cooking rather than removal of the bats as food items may be more rewarding. Another approach may be deforestation of some of the forests where the fruit bats breed.
Ebola outbreak in West Africa (2014-2016) was a Public Health Emergency and requires emergency preparedness to forestall future occurrence. Emergency conditions in Public Health are sudden unplanned mishaps with minimal or no notification of their occurrences. Emergency occurrence could be naturally- or artificiallymediated. Most emergency occurrences encountered in public health are naturally-mediated. Emergency occurrence in public health could also be akin to "Disaster". The aftermath of every disaster is usually consequential. Emergency preparedness in public health is the proactive measures put in place to respond to any foreseen or unforeseen emergency occurrence or Disaster in order to contain it [13]. Emergency preparedness could also connote Emergency or Disaster Management. EVD in West Africa which occurred between 2014-2016 represents an example of public health disaster of global significance that requires emergency preparedness. It has claimed so many lives in West Africa and in the Diaspora (i.e. Unites States, Spain and Italy). Irrespective of the magnitude prior to occurrence, every disaster requires a large scale of public health response. The environmental health professionals have a role to play with regards to its management to mitigate the consequences following the outcome of the outbreak. Some of the strategies of mitigation include food security, health care, accommodation and clothing. These strategies together with the CDC's public health emergency response guide and Schneider’s 12 points to public health management of disaster are the panaceas for building confidence in the Ebola affected populace. These are the acid-test of environmental preparedness.
The African continent has suffered great significant set-backs as a result of inadequate waste management with environment pollution, infectious diseases and vector-borne diseases (such as malaria, trypanosomiasis and the index case Ebola viral disease) taken much toll on the health of its citizens. The impact of improper refuse disposal on the health and socio-economic development of Nigeria is so substantial that it has contributed to decrease in life expectancy and developmental milestones in the country. Unfortunately, the management of wastes has received less attention and the priority it deserves [14]. It is therefore recommended that member countries affected by EVD in West Africa should devise a better and safer ways of management of environmental waste because refuse dumps contribute significantly to the chain of EVD transmission.
Conclusion
EVD outbreak in West Africa is a bioterrorism of public health importance. There is therefore, a need for emergency preparedness policy on EVD to be institutionalized in all health institutions in West Africa. In addition, we need to create conducive environment to break the epidemiologic triad chain of its transmission from the primary to the secondary reservoirs. The ministry of health in collaboration with other international stakeholders has a role to play to prevent future occurrences by putting all proactive measures in place in the region. Measures such as ensuring the sustainability of the health protecting policies geared towards eradication or curbing the ravaging menace of Ebola viral hemorrhagic disease to the barest minimum in the region should be upheld. Others include public health awareness campaign on EVD, proper waste management, hygiene therapy, definitive therapeutic and prophylactic (immunization) interventions in the targeted population.
References
- Abah SO, Ohimain EI (2010) Assessment of Dumpsite Rehabilitation Potential using the Integrated Risk Based Approach: A case study of Eneka, Nigeria. World Appl Sci J 8: 436-442.
- Centers for Disease Control and Protection (2012) Principles of Epidemiology in Public Health Practice, Third Edition. An Introduction to Applied Epidemiology and Biostatistics.
- Centers for Disease Control and Prevention (2014) Understanding the Epidemiologic Triangle through Infectious Disease. U.S. Department of Health & Human Services.
- Center for Disease Control and Protection (2014) Bioterrorism agents/diseases. U.S. Department of Health & Human Services.
- Center for Disease Control and Protection (2017) Ebola outbreak in West Africa 2014-2016. U.S. Department of Health & Human Services.
- Dahlgren G, Whitehead M (1991) Policies and Strategies to Promote Social Equity in Health. Stockholm: Institute for Futures Studies.
- Fasina FO, Shittu A, Lazarus D, Tomori O, Simonsen L, et al. (2014) Transmission dynamics and control of Ebola virus disease outbreak in Nigeria, July to September 2014. Euro Surveill 19: 20920.
- Leroy EM, Kumulungui B, Pourrut X, Rouquet P, Hassanin A, et al. (2005) Fruit bats are reservoirs of Ebola virus. Nature 438: 575-576.
- Mary-Jane Schneider (2011) Introduction to Public Health. Navigate 2 Advantage Access.
- Modebe IA, Onyeonoro UU, Ezeama NN, Ogbuagu CN, Agam NE (2009) Public Health Implication of Household Solid Waste Management in Awka, South East Nigeria. The Internet Journal of Public Health 1: 1-6.
- Nwachukwu NC, Orji FA, Ugbogu OC (2013) Health Care Waste Management- Public Health Benefits, and the Need for Effective Environmental Regulatory Surveillance in Federal Republic of Nigeria. Current Topics in Public Health.
- Onyeonoro UU, Ekpemiro UC, Abali C, Nwokeukwu HI (2015) Ebola epidemic - the Nigerian experience. Pan Afr Med J 22: 17.
- World Health Organization (2014) Ebola virus disease, West Africa – update. Disease Outbreak News.
Citation: Nwabuko OC, Nwamoh UN, Chikezie JA (2018) A Retrospective Review of Ebola Outbreak in West Africa: Social Determinants and Control Measures. Epidemiology (Sunnyvale) 8: 360. DOI: 10.4172/2161-1165.1000360
Copyright: © 2018 Nwabuko OC, et al. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.
Share This Article
Recommended Journals
Open Access Journals
Article Tools
Article Usage
- Total views: 5414
- [From(publication date): 0-2018 - Apr 03, 2025]
- Breakdown by view type
- HTML page views: 4568
- PDF downloads: 846