Case Report Open Access
A Rare Cause of Intestinal Volvulus: Spontaneous Intramural Hematoma of Small Intestine
Y El Gamrani1*, Z Chahbi2, H Qacif2, S Kaddouri2, A Ait Badi2 and M Zyani21Department of Gastroenterology, Avicenne Military Hospital, Marrakech, Marocco
2Department of Internal Medicine, Avicenne Military Hospital, Marrakech, Marocco
- Corresponding Author:
- Younes El Gamrani
Department of Gastroenterology
Avicenne Military Hospital, Morocco
Tel: 212661246569
E-mail: younes.elga@hotmail.fr
Received Date: September 01, 2015; Accepted Date: April 20, 2017; Published Date: April 27, 2017
Citation: El Gamrani Y, Chahbi Z, Qacif H, Kaddouri S, Badi AA, et al. (2017) A Rare Cause of Intestinal Volvulus: Spontaneous Intramural Hematoma of Small Intestine. J Gastrointest Dig Syst 7:502. doi:10.4172/2161-069X.1000502
Copyright: © 2017 El Gamrani Y, et al. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.
Visit for more related articles at Journal of Gastrointestinal & Digestive System
Abstract
Introduction: Anticoagulation therapy is widely used for curative and prophylactic purposes. The most serious complication is bleeding, which presents as an intramural hematoma of the small intestine; however, it is uncommon, seen in 1 in 2,500 patients. We report an unusual case of a warfarin overdose that resulted in spontaneous intramural hematoma of the small intestine with intestinal volvulus.
Observation: A 60-year-old patient was admitted to the emergency department with diffuse abdominal pain and anuria that had started several hours earlier. The patient had a long history of complicated diabetes, marked by moderate chronic renal failure as well as arterial hypertension and atrial fibrillation, which was managed with the oral anticoagulant acenocoumarol. Respiratory and cardiovascular exams revealed no abnormality except for an irregular rhythm in cardiac auscultation. His abdomen was mildly distended and there was tenderness with Blumberg’s sign in the periumbilical region, which was associated with signs of peritoneal irritation. Laboratory tests showed incoagulable plasma, an inflammatory syndrome, and renal failure. The Computed tomography (CT) scan without intravenous injection revealed a spontaneous intramural hematoma of the small intestine with intestinal volvulus; moderate hemoperitoneum was also documented. Initial patient management consisted of the cessation of oral anticoagulation therapy, gentle gastric aspiration, correction of the coagulopathy with fresh frozen plasma, and the administration of parenteral Vitamin K. The patient’s condition began to decline, marked by a worsening of clinical and laboratory parameters, and the patient ultimately died from acute cardio-circulatory failure while on ventricular fibrillation.
Conclusion: Spontaneous small intestine hematoma is an uncommon clinical complication, but it should be taken into consideration for any patient on long-term anticoagulation therapy who presents with acute abdomen. Abdominal CT is the key for diagnosis. Early diagnosis is crucial because most patients can be treated nonoperatively with a good outcome.
Keywords
Oral anticoagulant; Overdose; Hematoma; Small intestine; Volvulus
Introduction
Anticoagulation therapy is widely used for curative and prophylactic purposes. The most serious complication is bleeding. Many types of bleeding are commonly described as minor, such as ecchymosis, epistaxis, gingival bleeding, and hematuria. However, more serious bleeding can occur in certain organs such as the brain, the pericardium, the pleura, or the abdomen [1].
Bleeding, presenting as an intramural hematoma of the small intestine, is a rare complication, seen in 1 in 2,500 patients [2]. The clinical presentation of the small intestine intramural hematoma can vary from simple abdominal pain to an acute abdomen with intestinal obstruction. CT scan has to be performed in emergency and usually confirms diagnosis. Most patients without complications can be treated medically. We report an unusual case of a warfarin overdose that resulted in spontaneous intramural hematoma of the small intestine with intestinal volvulus.
Case Report
A 60-year-old patient was admitted to the emergency department with diffuse abdominal pain and anuria that had started several hours earlier. The patient had a long history of complicated diabetes, marked by moderate chronic renal failure as well as arterial hypertension and atrial fibrillation, which was managed with the oral anticoagulant acenocoumarol (Sintrom). The patient has no surgical history.
His vital signs were normal, with arterial blood pressure at 150/80 mmHg. Respiratory and cardiovascular exams revealed no abnormality except for an irregular rhythm in cardiac auscultation. His abdomen was mildly distended and there was tenderness was tenderness with Blumberg’s sign in the periumbilical region, which was associated with signs of peritoneal irritation.
Laboratory tests showed a hemostasis disorder with incoagulable plasma (an international normalized ratio (INR) >10), renal failure with creatinine at 279 umol/l, hyperkalemia at 5.9 mmol/l, and an inflammatory syndrome: C-reactive protein to 98 mg/l, hemoglobin at 12.3 g/dl, white cell count at 18,000 cells /mm3, and a platelet count at 230,000 cells/mm3.
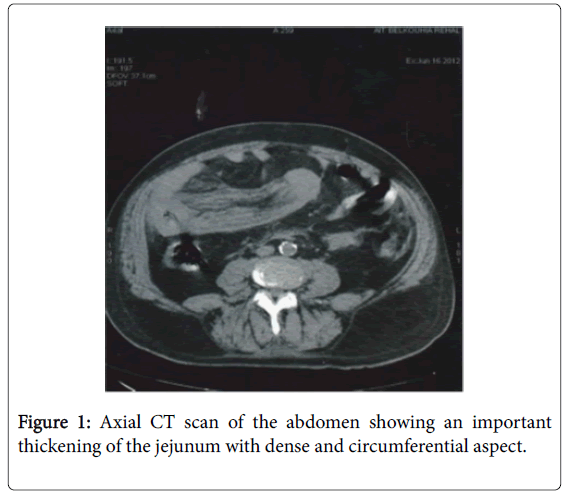
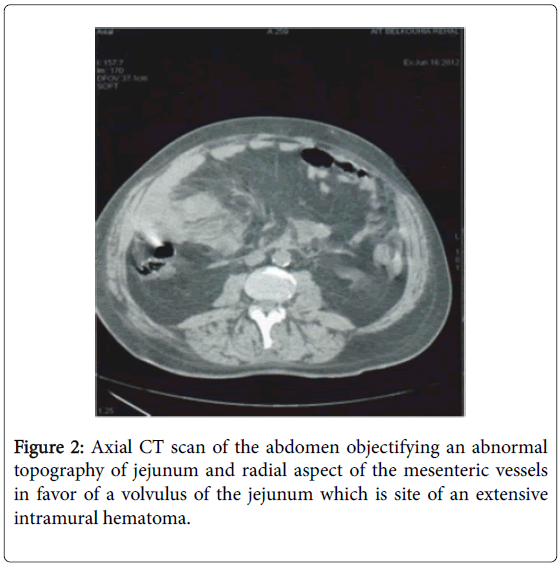
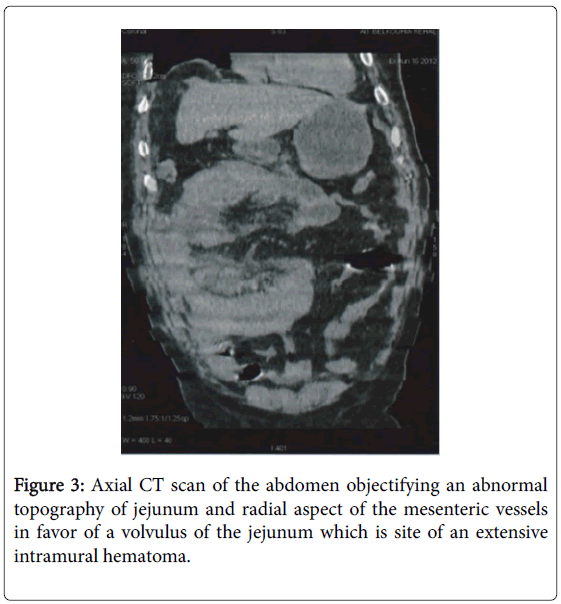
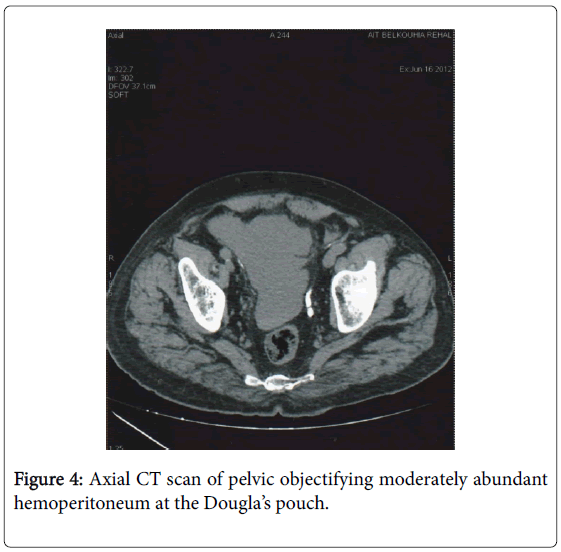
The CT scan showed a significant dense, circumferential thickening of the jejunum wall (Figure 1), abnormal jejunum topography, and Whirlpool sign (Figures 2 and 3). Based on these CT findings, spontaneous intramural hematoma of the small intestine with intestinal volvulus was diagnosed. A moderate hemoperitoneum was also documented (Figure 4).
Initial patient management consisted of the cessation of oral anticoagulation therapy, gentle gastric aspiration, correction of the coagulopathy with fresh frozen plasma, and the administration of parenteral vitamin K. The patient’s condition began to decline, marked by a worsening of clinical and laboratory parameters: a drop in blood pressure to 80/50 mmHg, creatinine at 301 umol/l, development of anemia with hemoglobin at 9.5 g/dl, and potassium at 5.6 mmol/l with anuria. Due to this progression, the patient was taken for emergency hemodialysis. During his transfer, the patient died from acute cardiocirculatory failure in ventricular fibrillation.
Discussion
Spontaneous intramural hematoma of the small intestine is a rare complication of long-term anticoagulation therapy, seen in 1 in 2,500 patients [2]. The mean age at presentation in a recent series of 13 patients was 64 years; 15% of the patients in this series had multiple hematomas [2]. The jejunum is the most affected location, unlike the duodenum, which is much more affected by post-traumatic intramural hematoma [3]. A rupture of the terminal arteries as they leave the mesentery and penetrate the muscularis layer of the intestinal wall would be the most probable physiopathology of spontaneous intramural hematoma of the small intestine. Consequently, the hemorrhage dissects the bowel wall between the muscularis mucosa and the muscularis layers. Unlike mesenteric vascular occlusion, the viability of the mucosa is preserved [4,5]. Intra-peritoneal hemorrhagic effusion, when present, is related to the leakage of blood from an enlarged, thickened and inflamed bowel wall with submucosal bleeding into all layers [3-5]. Clinical presentation can vary from mild, vague abdominal pain to intestinal obstruction and an acute abdomen [6,7]. Our patient displayed an acute abdomen with widespread abdominal defense. In contrast to small bowel trauma, which commonly affects the duodenum and tends to be focal, spontaneous small bowel hematomas are more extensive and most commonly involve the jejunum, followed by the ileum and colon [3,6]. Once spontaneous intramural hematoma of the small intestine is suspected, the patient’s past medical history and current medication should be carefully reviewed in order to establish the correct diagnosis and management. Co-morbidities such as hypertension [8-11], atrial fibrillation [10], and renal failure [9] also appear to be risk factors for hemorrhagic complications. Oral anticoagulation therapy with warfarin was reported to be the most common predisposing factor for spontaneous intramural hematoma of the small intestine [3,12]. Routine laboratory tests in cases suspected for SIHSI should include complete blood count, routine biochemical analysis, coagulation parameters, and bleeding time. INR is used as an indicator of the anticoagulant effect, and values greater than 3 are associated with an increased risk of bleeding. In the absence of other already known lesions, the inability to measure the Prothrombin ratio with incoagulated plasma suggested an Anti-vitamin Koverdose in our patient. Some studies have shown that the risk of major bleeding was significantly increased when the INR is above 5 [13,14], and mortality was closely linked to the level of INR in patients on anticoagulation [14].
An abdominal CT is key for diagnosis, with characteristics including circumferential wall thickening, Intramural spontaneous hematic density, luminal narrowing, intestinal obstruction, and hematic density effusion [3]. These characteristics were found in our patient. Where CT is unavailable, US in combination with abdominal radiography may be sufficient to diagnose intramural hematoma. Indicative findings are tubular or circular images with the absence of peristalsis and mucous compression enveloped by an anechoic halo corresponding to the thickened intestinal wall. Echogenicity varies according to the stage of maturation of the hematoma [15,16]. The appearance as acute obstructive abdomen may lead to operative treatment, although the use of US and CT in diagnosis has contributed to changes in conduct. Surgical exploration, which was previously used as a diagnostic method, has now primarily become a treatment method reserved for cases with complications that include intra-abdominal hemorrhage, suspected ischemia with or without perforation, and peritonitis due to diagnosis doubt or to late complications. Clinical treatment should be instituted in the absolute majority of cases.
The first treatment steps are discontinuation of the anticoagulant medication, gastric decompression in the presence of vomiting, the correction of electrolyte disturbances, administration of vitamin K, and the transfusion of fresh frozen plasma and blood when indicated. Total parenteral nutrition may be necessary. In cases where there are no complications and surgery is unnecessary, resolution tends to occur within a few days. The recurrence of bleeding, as well as late sequelae such as stenosis, is unusual. In the presence of an intramural hematoma, death has occurred as a result of secondary complications such as digestive hemorrhage due to ulcer [16].
Conclusion
Spontaneous small intestine hematoma is a rare clinical entity. It should be considered in any patient on long-term anticoagulation therapy who presents with an acute abdomen. Abdominal CT is the key for diagnosis. Non-invasive investigative methods offer high accuracy, permitting the adoption of medical procedures that avoid unnecessary surgery. Complete resolution of the condition within a short period of time occurs in nearly 100% of cases.
References
- Becker A, Berlin Y, Sayfan J (1999) Spontaneous rupture of mesenteric hematoma with hemorrhagic shock as a complication of oral anticoagulant treatment. Isr Med Assoc J 1: 196-197.
- Uzun MA, Koksal N, Gunerhan Y (2007) Intestinal obstruction due to spontaneous intramural haematoma of the small intestine during warfarin use: A report of two cases. Eur J Emerg Med 14: 272-273.
- Abbas MA, Collins JM, Olden KW (2002) Spontaneous intramural small-bowel haematoma: Imaging findings and outcome. AJR Am J Roentgenol179: 1389-1394.
- Hale JE (1975) Intramural intestinal haemorrhage: A complication of anticoagulant therapy. Postgrad Med J 51:107-110.
- Nakayama Y, Fukushima M, Sakai M, Hisano T, Nagata N, et al. (2006) Intramural hematoma of the cecum as the lead point of intussusception in an elderly patient with hemophilia A: Report of a case. Surg Today 36:563-565.
- Hou SW, Chen CC, Chen KC (2008) Sonographic diagnosis of spontaneous intramural small bowel haematoma in a case of warfarin overdose. J Clin Ultrasound 36: 374-376.
- Birla RP, Mahawar KK, Saw EY (2008) Spontaneous intramural jejuna haematoma: A case report. Cases J 1: 389-391.
- Siguret V, Esquirol C,Debray M, Gouin I, Andreux JP, et al. (2003) Excess antivitamin K in elderly hospitalised patients aged over 70. A one-year prospective survey. Presse Med 32: 972-977.
- Oden A, Fahlen M (2002) Oral anticoagulation and risk of death: a medical record linkage study. BMJ 325:1073-1075.
- Gras-Champel V, Pannier M,Tellier V, Voyer A, Roussel B, et al. (2002) Hémorragiesintracrâniennesassociées à un traitement anticoagulant oral: Analyse de 38 observations. Therapie 57: 297-301.
- Constans J, Sampoux F, Jarnier P, Le Métayer P, Midy D, et al. (1999) Complications hémorragiques des antivitaminiques K: A propos de 75 patients hospitalisé. J Mal Vasc 24: 202-207.
- Landefeld CS, Goldman L (1989) Major bleeding in outpatients treated with warfarin: Incidence and prediction by factors known at the start of outpatient therapy. Am J Med 87: 144-152.
- Fingerhut A, Eugene C, Pourcher J, Pelletier JM, Ronat R (1980) Les hématomesintramuraux du duodenum. GastroenterolClinBiol 4: 144-148.
- Abbas MA, Collins JM, Olden KW, Kelly KA (2002) Spontaneous intramural small-bowel hematoma: Clinical presentation and long-term outcome. Arch Surg 137: 306-310.
- Polat C, Dervisoglu A, Guven H, Kaya E, Malazgirt Z, et al. (2003) Anticoagulant-induced intramural intestinal hematoma. Am J Emerg Med 21: 208-211.
- Lorente-Ramos RM, Santiago-Hernando A, Del Valle-Sanz Y, Arjonilla- Lopez A (1999) Sonographic diagnosis of intramural duodenal hematomas. J Clin Ultrasound 27:213-216.
Relevant Topics
- Constipation
- Digestive Enzymes
- Endoscopy
- Epigastric Pain
- Gall Bladder
- Gastric Cancer
- Gastrointestinal Bleeding
- Gastrointestinal Hormones
- Gastrointestinal Infections
- Gastrointestinal Inflammation
- Gastrointestinal Pathology
- Gastrointestinal Pharmacology
- Gastrointestinal Radiology
- Gastrointestinal Surgery
- Gastrointestinal Tuberculosis
- GIST Sarcoma
- Intestinal Blockage
- Pancreas
- Salivary Glands
- Stomach Bloating
- Stomach Cramps
- Stomach Disorders
- Stomach Ulcer
Recommended Journals
Article Tools
Article Usage
- Total views: 4141
- [From(publication date):
April-2017 - Jul 01, 2025] - Breakdown by view type
- HTML page views : 3275
- PDF downloads : 866