Case Report Open Access
A Rare Case Report - Primary Pulmonary Artery Sarcoma
Chudasama B*, Parmar Z, Desai S, Rajpura H, Jetly D and Nilkanthe RDepartment of Radiology, Gujarat Cancer and Research Institute, Vejalpur, Ahmedabad, Gujarat, India
- *Corresponding Author:
- Chudasama B
Department of Radiodiagnosis, Gujarat Cancer and Research Institute
Vejalpur, Ahmedabad, Gujarat, India
Tel: +919426359236
E-mail: bhadresh4192@gmail.com
Received date: November 10, 2016; Accepted date: November 23, 2016; Published date: November 28, 2016
Citation: Chudasama B, Parmar Z, Desai S, Rajpura H, Jetly D, et al. (2016) A Rare Case Report - Primary Pulmonary Artery Sarcoma. OMICS J Radiol 5:241. doi: 10.4172/2167-7964.1000241
Copyright: © 2016 Chudasama B, et al. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.
Visit for more related articles at Journal of Radiology
Abstract
The primary pulmonary artery sarcomas are rarely seen, can imitate pulmonary thromboembolism. The prognosis of patients with pulmonary artery sarcomas is dependent on its early and accurate diagnosis. Placed below is a description of a case of a 51-year-old man presented with dry cough and breathlessness was initially thought to have a Koch's lesion. AKT was given but the patient did not improve. Then on CT pulmonary angiography patient was suspected of having pulmonary embolus or hypo attenuating mass lesion and was given anticoagulation with unfractionated heparin, which was ineffective. CT guided biopsy of an enlarged right hilar nodal mass led to the diagnosis of primary pulmonary artery sarcoma.
Keywords
CT pulmonary angiography; Radiology/pathology; Primary pulmonary artery; Sarcoma diagnosis; Differential vascular neoplasm
Introduction
Around 200 cases of primary pulmonary artery sarcomas have been reported by Mandelstamm [1,2]. The pulmonary artery sarcomas are often confused with chronic pulmonary thromboembolism [3]. Over a period of time, it is learnt that timely diagnosis, though challenging, but is essential for its treatment [4]. The patients of primary pulmonary artery sarcoma do not have risk factors for venous thromboembolism.
Case Report
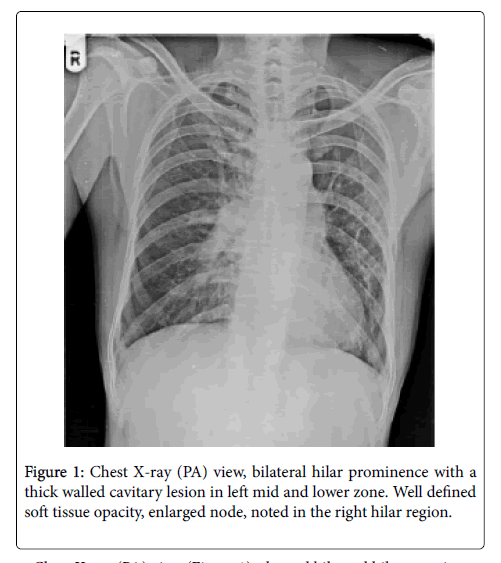
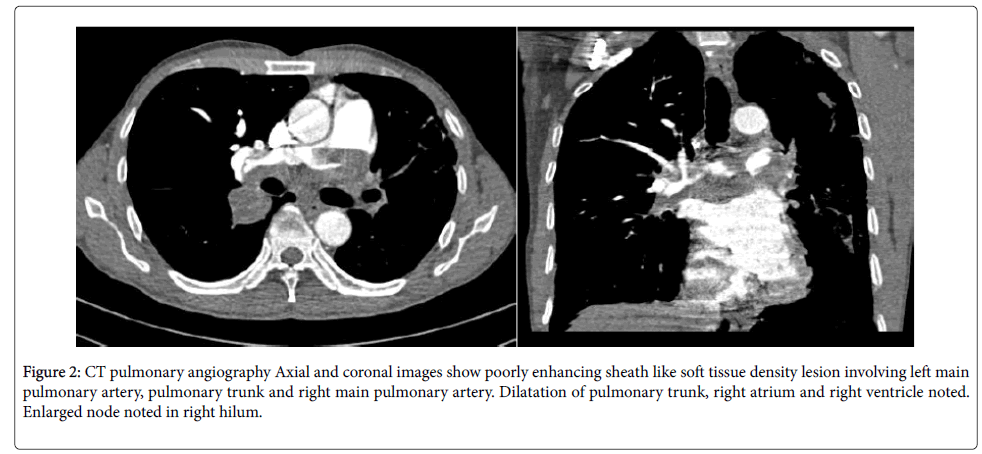
In April 2016, a 51-year-old male patient was presented with a three-year history of dry cough and breathlessness. Chest X-ray (PA) view (Figure 1) was done, which showed bilateral hilar prominence with a thick walled cavitary lesion in left mid and lower zone. There was well defined soft tissue opacity, enlarged node, noted in the right hilar region. The patient was suspected of having Koch's disease because of the cavitary lesion in left lung and was on AKT since November 2015. Patient’s condition didn’t improve and worsened. CT pulmonary angiography was done as further investigation. On CT pulmonary angiography (Figure 2), poorly enhancing sheath like soft tissue density lesion involving left main pulmonary artery, pulmonary trunk and right main pulmonary artery with dilatation of pulmonary trunk and right sided cardiac chambers and enlarged node in right hilum. CT pulmonary angiography findings suggested either thromboembolism or poorly enhancing mass lesion. Anticoagulation therapy in form of unfractionated heparin was given but it resulted in no improvement. CT guided biopsy of enlarged right hilar node was done from posterior approach in the prone position. Microscopically, section showed malignant high-grade spindle cell tumour consistent with sarcoma. Immunohistochemical stains were performed and were suggestive of primary pulmonary artery sarcoma. The tumor was unrespectable; the patient denied chemotherapy and has not been reported back to the hospital.
Chest X-ray (PA) view (Figure 1), showed bilateral hilar prominence with a thick walled cavitary lesion in left mid and lower zone. Well defined soft tissue opacity, enlarged node, noted in the right hilar region.
On CT pulmonary angiography (Figure 2), poorly enhancing sheath like soft tissue density lesion noted involving left main pulmonary artery, pulmonary trunk, right main pulmonary and lower lobar pulmonary artery with intraluminal extension. Dilatation of pulmonary trunk, right atrium and right ventricle noted with enlarged node in right hilum. The cavitary lesion noted in left lung on lung window images.
Figure 2: CT pulmonary angiography Axial and coronal images show poorly enhancing sheath like soft tissue density lesion involving left main pulmonary artery, pulmonary trunk and right main pulmonary artery. Dilatation of pulmonary trunk, right atrium and right ventricle noted. Enlarged node noted in right hilum.
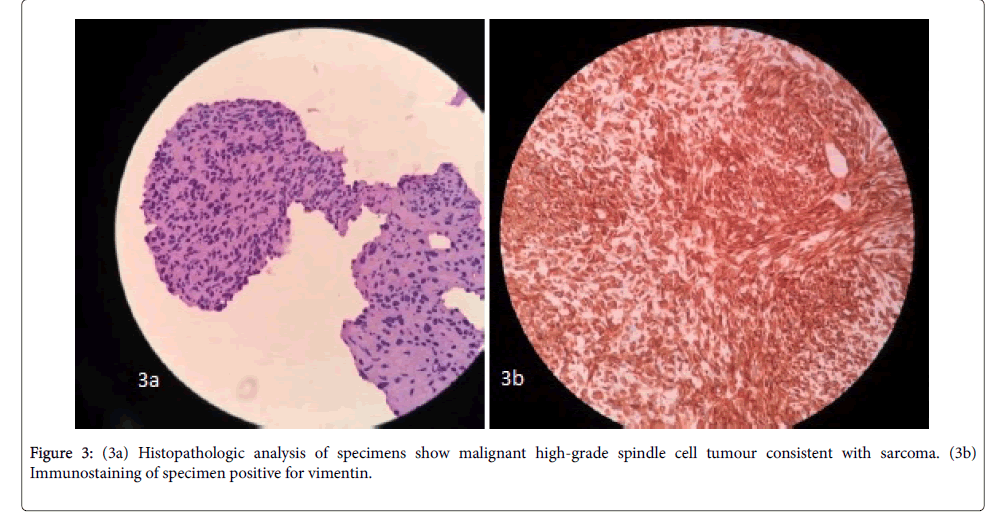
Histopathologic analysis of specimens obtained showed a malignant high-grade spindle cell tumour with necrosis and marked to moderate atypia consistent with sarcoma. Concomitant ribbon-like, twisted fungal hyphae were also seen (Figure 3a). Immunostaining of the specimen was positive for vimentin (Figure 3b), focal positive for pancytokeratin (AE1) and negative for Ck7, TTF1 and P63. Morphologic and immunostaining analysis were consistent with primary pulmonary artery sarcoma.
Discussion
Most primary pulmonary artery sarcomas are highly aggressive malignant tumour, with a mean survival of 23 months from the presentation time [5]. Primary pulmonary artery sarcomas are very rare with an incidence of 0.001–0.03% [2]. It usually presents in adults, with median age of presentation of 50 years [3]. One study has reported female predominance [2].
The patients usually present with progressive pulmonary artery occlusion and right sided heart failure, clinically almost indistinguishable from pulmonary thromboembolic disease [3-5].
Yi et al. have described that CT can help differentiate pulmonary artery sarcoma from pulmonary embolism by indicating a lowattenuation filling defect occupying the entire luminal diameter of the proximal or main pulmonary artery, expansion of the involved arteries, or extraluminal tumor extension [6].
Vascular sarcomas are classified as mural or intimal [5]. Intimal sarcomas originate from pleuripotent intimal cells and commonly show intraluminal growth in the pulmonary arteries. On microscopy they appear as poorly differentiated malignant mesenchymal tumours. Mural sarcomas of the pulmonary artery are leiomyosarcomas arising from the vascular media.
Treatment involves combinations of chemotherapy, radiation therapy and surgery with surgical resection being mainstay treatment option for patients with intimal sarcoma involving the pulmonary artery. Even with combined treatment including surgery, the prognosis for patients with pulmonary artery sarcoma is poor [3].
In conclusion, primary pulmonary artery sarcoma imitating pulmonary thromboembolism clinically can be differentiated with CT pulmonary angiography by above mentioned characteristics and should be included as the differential in such cases.
References
- Mandelstamm M (1923) Über primäre neubildungen des herzens Virchows Archiv 245:43-54.
- Levy E, Korach A, Amir G, Milgalter E (2006) Undifferentiated sarcoma of the pulmonary artery mimicking pulmonary thromboembolic disease. Heart Lung Circ 15:62-63.
- Cox JE, Chiles C, Aquino SL, Savage P, Oaks T (1997) Pulmonary artery sarcomas: a review of clinical and radiologic features. J Comput Assist Tomogr 21:750-755.
- Hsing JM, Thakkar SG, Borden EC, Budd GT (2007) Intimal pulmonary artery sarcoma presenting as dyspnea: case report. IntSeminSurgOncol4:14.
- Burke AP, Virmani R (1993) Sarcomas of the great vessels: A clinicopathologic study. Cancer 71:1761-1773.
- Chin AY, Lee KS, Choe YH, Han D, Kwon OJ, et al. (2004) Computed tomography in pulmonary artery sarcoma: distinguishing features from pulmonary embolic disease. J Comput Assist Tomogr 28: 34-39.
Relevant Topics
- Abdominal Radiology
- AI in Radiology
- Breast Imaging
- Cardiovascular Radiology
- Chest Radiology
- Clinical Radiology
- CT Imaging
- Diagnostic Radiology
- Emergency Radiology
- Fluoroscopy Radiology
- General Radiology
- Genitourinary Radiology
- Interventional Radiology Techniques
- Mammography
- Minimal Invasive surgery
- Musculoskeletal Radiology
- Neuroradiology
- Neuroradiology Advances
- Oral and Maxillofacial Radiology
- Radiography
- Radiology Imaging
- Surgical Radiology
- Tele Radiology
- Therapeutic Radiology
Recommended Journals
Article Tools
Article Usage
- Total views: 3568
- [From(publication date):
December-2016 - Mar 30, 2025] - Breakdown by view type
- HTML page views : 2783
- PDF downloads : 785