A Rare Case of Infected Retropharyngeal Haematoma in a 2-Year-Old Child with Coagulopathy
Received: 25-Nov-2019 / Accepted Date: 19-Dec-2019 / Published Date: 26-Dec-2019 DOI: 10.4172/2161-119X.1000390
Abstract
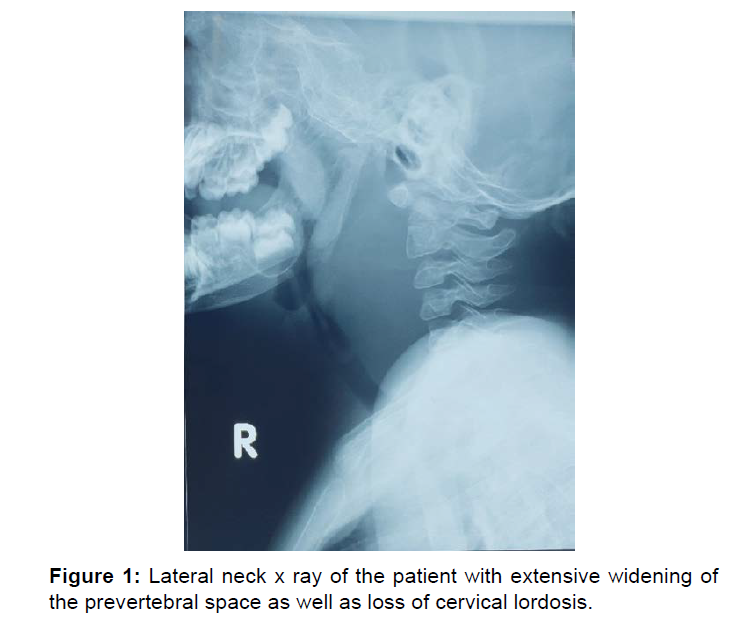
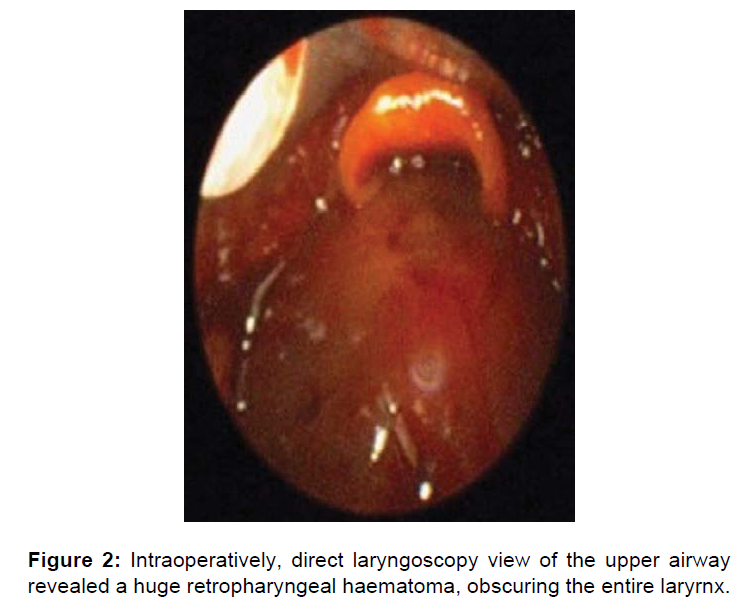
Spontaneous retropharyngeal haematoma is a rare, life-threatening condition which is difficult to diagnose, especially in pediatric age group. We encountered a case of infected spontaneous retropharyngeal haematoma who presented with acute respiratory compromise. We present a case of a 2-year-old child with alagille syndrome who presented with fever, poor oral intake and left neck swelling for 3 days, worsening with acute respiratory compromise for 1 day. There was obvious widening of the prevertebral soft tissue on the lateral neck x radiograph. Tracheostomy under local anesthesia was done, and direct laryngoscopy revealed huge collection over the posterior pharyngeal wall covering almost the entire larynx. Upon incision and drainage, there was very minimal pus with blood clots. Child was subsequently treated with intravenous antibiotics and managed to wean off tracheostomy tube. Lateral neck x ray could be a valuable tool in diagnosing retropharyngeal haematoma/abscess. In a child with coagulopathy, who presented with acute shortness of breath with dysphagia, spontaneous retropharyngeal haematoma should be considered.
Keywords: Retropharyngeal haematoma; Coagulopathy; Dysphagia; Abscess
Introduction
Retropharyngeal haematoma is a rare, life-threatening condition which is difficult to diagnose, especially in paediatric age group [1]. We encountered a case of infected retropharyngeal haematoma in a 2-yearold child with coagulopathy, who presented with acute respiratory compromise requiring life-saving emergency tracheostomy.
Case Report
A 2-year-old child with alagille syndrome presented with fever, poor oral intake and left neck swelling for 3 days, worsening with acute respiratory compromise for 1 day. The child was diagnosed with alagille syndrome, which is an autosomal dominant disorder, associated with abnormalities of the liver, heart, kidneys, eye, skeleton, with characteristic facial features. As a consequence of the syndrome, he was not thriving well and was suffering from tetralogy of fallot awaiting cardiac operation, bile cholestasis with absent bile ductules, as well as bilateral renal parenchymal disease. He also had been having thrombocytopenia, with mildly deranged coagulation profile but had not had any bleeding tendencies. His immunization was up till 12 months of age. The child was the 3rd out of 4 siblings, and was solely taken care by his mother.
He presented to the emergency department, with fever, poor oral intake, and mild upper respiratory tract infection together with left neck swelling for 3 days. Mother noted that child also had a change of voice, but she was unable to describe further, claiming that there was no noisy breathing, or difficulty in breathing. She denied any bleeding tendencies, history of trauma, nor any recent sick contact.
Upon admission, he was noted to be febrile, consolable and was not in respiratory distress. There were bilateral shotty cervical lymph nodes, with the largest over the left posterior cervical chain, measuring 4 cm by 3 cm. He was admitted under peadiatric team and was treated for cervical lymphadenitis. After commencement of intravenous antibiotics, left neck swelling markedly reduced in size, but child was unwell. He was not able to tolerate feeding, and started having drooling of saliva. Blood stained secretions were noted during oral suctioning and attempts to insert nasogastric tube for feeding were futile.
His condition worsened, and he subsequently developed respiratory acidosis, requiring nasal BiPAP. He was then referred to ENT team for assessment. As there were copious amount of secretions and blood from the oropharynx, there were difficulties examining his oropharynx. A lateral neck radiograph was done and shockingly, there was obvious widening of the prevertebral soft tissue. He was brought to the operating theatre for stabilization of the airway. Endotracheal intubation was attempted, but larynx was unable to be visualised. Tracheostomy under local anesthesia was done eventually, followed by direct laryngoscopy which revealed a huge collection over the posterior pharyngeal wall obscuring almost the entire larynx. Upon incision and drainage, there were mainly blood clots with very minimal pus. Child was continued on intraveneous antibiotics. Pus drained from the retropharyngeal bulge grew extended spectrum beta-lactamase Escherichia coli sensitive to imipenem, and Pseudomona aeruginosa sensitive to meropenem. He was given intravenous imipenem for 2 weeks. Contrasted computed tomography of the neck was done 1 week post operatively and it revealed oedema of the retropharyngeal space, with no enhancing collection or obvious haematoma. He was able to wean off tracheostomy tube around 3 weeks post operatively and tolerated oral feeding well (Figures 1 and 2).
Discussion
Retropharyngeal haematoma is an unusual cause of acute upper airway obstruction which is difficult to diagnose, especially in the paediatric age group [1]. There are numerous aetiologies leading to this condition, namely anti-coagulant therapy, trauma, infection, foreign body ingestion, bleeding from paraesophageal veins, rupture of carotid artery, or even angiographic procedures [2]. When there is no identifiable cause, it is deemed as a spontaneous retropharyngeal haematoma [3].
Bleeding into the retropharyngeal space could be dangerous, as the anatomic property of the pharyngeal muscles offers no resistance to the expansion of the haematoma, which would eventually lead to obstruction of the airway [2].
Retropharyngeal abscess is an important differential diagnosis as it could develop as a sequela of upper respiratory tract infections [4], with similar presentations such as acute respiratory compromise and neck swelling.
It is difficult to diagnose retropharyngeal haematoma as the symptoms may be non-specific and consistent with upper respiratory tract infections, such as neck swelling, refusal to feed or even respiratory compromise [1]. In this case, child initially presented with upper respiratory tract infections with neck swelling which was treated as cervical lymphadentis. He was seemingly improving on intravenous antibiotics, but his refusal for feed and subsequent development of drooling together with acute respiratory compromise led to the suspicion of retropharyngeal abscess or haematoma. The absence of fever and the normal total white count were more in favour of a haematoma. There were multiple attempts to insert nasogastric tube for feeding but to no avail and there were bloody secretions from his oropharynx. Though the child had no bleeding diathesis thus far, his platelet was low at the level of 85 × 109/L, prothrombin time and the partial thromboplastin time were prolonged, with an INR of 1.52. His liver function test was also deranged, with raised liver enzymes and bilirubin level.
The lateral neck radiograph which was requested in time provided the most important information for the diagnosis of retropharyngeal collection. Prevertebral soft tissue thickness can be assessed from the soft tissue lateral neck radiographs and this is useful to detect prevertebral pathologies such as haematoma or abscesses. Lateral neck radiographs are reported to be about 83% sensitive in children in comparison to computed tomography [5]. Moreover, it is readily available and convenient to perform as children do not need to be sedated. Nonetheless, computed tomography and magnetic resonance would undoubtedly provide better soft-tissue contrast for more accurate diagnoses.
The first step in management of retropharyngeal haematoma is to establish a secured airway [6]. In this case, child was brought to the operating theatre for fibreoptic intubation under sedation. However, the retropharyngeal bulge was covering the entire larynx and we had to proceed with emergency tracheostomy followed by incision and drainage.
Close observation and monitoring under the intensive care unit as well as antibiotic coverage post operatively are essential [6]. Serial radiographs should also be done to ensure resolution of the haematoma.
Conclusion
Timely diagnosis of this life-threatening condition would ensure favourable outcome. Lateral neck x ray could be a valuable tool in diagnosing retropharyngeal haematoma/abscess. In a child with coagulopathy, who presented with acute shortness of breath with dysphagia or drooling, retropharyngeal haematoma should be considered.
Acknowledgement
We would like to thank the Director General of Health Malaysia for his permission to publish this article
Conflict of Interest
There is no conflict of interest.
References
- Mundra RK, Richi Sinha, Sunil Bajoliya (2014) Spontaneous Retropharyngeal Hameatoma in a one-year-old child: A case report. Case Reports Clin Med 3: 272-275.
- Muñoz A, Fischbein NJ, de Vergas J, Crespo J, Alvarez-Vincent J (2001) Spontaneous Retropharyngeal Haematoma: Diagnosis by MR Imaging. Am J Neuroradiol 22: 1209-1211.
- Pokharel A, Basnet P, Mayya NJ, Kandel D (2019) Spontaenous Retropharyngeal Haematoma:Case Report and Literature Overview. J College Med Sci Nepal 15: 153-155.
- Woods CR, Cash ED, Smith AM, Smith MJ, Myers JA, et al. (2016) Retropharyngeal and Parapharyngeal Abscesses Among Children and Adolescents in the United States: Epidemiology and Management Trends, 2003–2012, J Pediatric Infect Dis Soc 5: 259–268.
- Manuelito MR, Rosario RR, Jennifer BT, Concepcion JB (2011) Prevertebral Soft Tissues Thickness among Pediatric Patients. Philippine J Otolaryngol Head Neck Surg 26: 5-9.
- Wei Y, Jahreiß L, Zhang Z, Albers AE (2015) Acute airway obstruction due to retropharyngeal haematoma caused by a large fish bone in a patient with hypertension caused by a pheochromocytoma. BMJ Case Rep 2015: 1-4.
Citation: Ong HY, Ng JJ, Baiduri ZAPN, Santhi K, Ng WSJ (2020) A Rare Case of Infected Retropharyngeal Haematoma in a 2-Year-Old Child with Coagulopathy. Otolaryngol (Sunnyvale) 10: 390. DOI: 10.4172/2161-119X.1000390
Copyright: © 2020 Ong HY, et al. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.
Share This Article
Recommended Journals
Open Access Journals
Article Tools
Article Usage
- Total views: 2321
- [From(publication date): 0-2020 - Apr 07, 2025]
- Breakdown by view type
- HTML page views: 1567
- PDF downloads: 754