Research Article Open Access
A Qualitative Evaluation of the Impact of Palliative Care among Women Cancer Patients in Eastern India
Datta A1*, Aditya C2, Chakraborty A3, Das P3 and Mukhopadhyay A3
1Department of Psychology, Netaji Subhas Bose National Cancer Research Institute, Kolkata, India
2Department of Psychology, Bijoykrishna Girls' College, Howrah, India
3Department of Oncology, Netaji Subhas Bose National Cancer Research Institute, Kolkata, India
- *Corresponding Author:
- Datta A
Department of Psychology
Netaji Subhas Bose National Cancer Research Institute
16A Park Lane, Kolkata, 700016, India
E-mail: arunima.datta8@gmail.com
Received date: Feb 29, 2016; Accepted date: Apr 23, 2016; Published date: Apr 27, 2016
Citation: Datta A, Aditya C, Chakraborty A, Das P, Mukhopadhyay A (2016) A Qualitative Evaluation of the Impact of Palliative Care among Women Cancer Patients in Eastern India. J Palliat Care Med 6:259. doi:10.4172/2165-7386.1000259
Copyright: © 2016 Datta A, et al. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.
Visit for more related articles at Journal of Palliative Care & Medicine
Abstract
Background: Many women diagnosed with cancer in low and middle income in Eastern countries present with advance stage with disease. While cure is not a realistic outcome, palliative care can achieve meaningful outcomes and improved quality of life. Objective: This study illustrates understanding the effects of cancer among patients and increase in quality of life by optimal management and care. Explore intra correlation among the techniques of palliative care along with, association between sociodemographic factors and rate of participation in palliative care clinic. Methods: We randomly selected 73 female patients who received early PC. Four techniques were used, including ice breaking, personal history, gain knowledge regarding disease, psychological support. Each session had taken 40-45 minutes. Quality of life was measured by using Warwick-Edinburgh Mental Well-being Scale (WEMWBS) at baseline and after giving all techniques at 2 months of post-treatment. Results: A total of 73 cancer patients competed the study with 75% was female type cancer, 4.2% lung cancer, 5.6% blood cancer and 15.3% other type of cancer. In the WEMWBS, improvement was observed at 2 months follow-up after giving PC among follow-up patients. Conclusion: Early PC clinic visits emphasize managing symptoms, improving quality of life, and cultivating illness understanding and prognostic awareness in a responsive and time-sensitive model.
Keywords
Palliative care; Cancer; Quality of life; Ice breaking; Personal history; Psychological support
Introduction
The majority of cancer patients experience a number of distressful physical and psychosocial symptoms during the course of their illness that significantly affect their quality of life [1-6]. The goal of palliative care is to prevent and relieve suffering, and to improve the quality of life of patients and their families diagnosed with life-threatening or serious debilitating illnesses [7]. Previous studies have suggested that late referrals to palliative care are inadequate to alter the quality and delivery of care provided to patients with cancer [8,9]. To have a meaningful effect on patients’ quality of life (QOL) and end-of-life care, palliative care services can be provided earlier in the course of the disease.
The goal of palliative care is to improve patients’ QOL. A critical component in improving QOL is aggressive management of physical symptoms. Physical symptoms most commonly experienced by cancer patients are reported to include fatigue, dyspnoea, pain and constipation [10,11]. Constipation causes some degree of distress and has a negative effect on the patient’s overall QOL. In a study of 393 patients with cancer, patients ranked constipation control as sixth in importance out of 25 items related to overall QOL [12]. Uncontrolled symptoms clearly have a negative impact on all aspects of QOL, including emotional and spiritual well-being, social relationships, and functional ability [13,14]. Most clinicians and researchers agree that improvement in the patient's QOL is the ultimate goal in care of cancer patients near the end of life, and this is consistent with the approach of the World Health Organization (WHO). New days cancer care for the requires palliative care at the same time with focused treatments. Francis Peabody said best in 1927: “the reward is to be found in that personal bond which forms the greatest satisfaction of the practice of medicine. One of the essential qualities of the clinician is interest in humanity, for the secret of the care of the patient is in caring for the patient [15]. The expected outcome of palliative and hospice care is to control patients’ symptoms to ensure a high level of QOL in all its dimensions. Divya Pal Singh in his study focused over palliative care services is to improve the patient’s quality of life (QOL), which is defined as the subjective evaluation of life as a whole or the patient’s appraisal and satisfaction with their current level of functioning compared with what they perceive to be possible or ideal [16]. Gupta et al. elicited scenario of palliative care for cancer patients in India.
There they concluded that in India, every hour more than 60 patients die from cancer. More than 80% of cancers in India present in advanced stages. This shows the need of palliative care and pain relief for the cancer patients in India [17]. Khosla et al. had prominent current progress and future needs of palliative care in India. They made decision that current palliative care knowledge into care of patients includes multidisciplinary educational initiatives, research endeavors, and clinician resources. Still, a lot needs to be done for creating awareness and training in Palliative Care [18].
The objectives of this study were to determine the positive effects of palliative care in quality of life of affected people and comparison with sub-techniques on patient referral and to determine whether there was an association between demographic factors and the perceptions of different sub techniques by the psychologist.
Methods
Design
A prospective, follow-up study with the overall aim to examine the effectiveness of psychological intervention over diagnosed with women cancer patients. A dropout analysis was performed and results from this analysis were presented in this paper with focus on the difference in QoL between effect of pre and post treatment of palliative care therapy among participated patients.
Patient selection
A total of 136 consecutive advanced cancer patients were invited to participate in the questionnaire study between July and September 2015 at Netaji Subhas Chandra Bose Caner Research Institute, Kolkata. To enter the study, patients should be diagnosed with advanced cancer, be over 20 years, and be able to communicate effectively with the psychologist.
Patients with primary and secondary tumours of the central nervous system were excluded from the study.
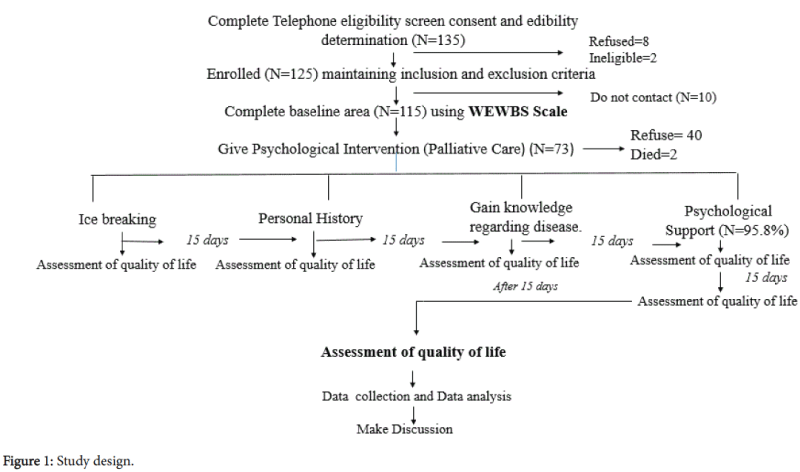
The study was introduced as a training session and people who interested in participating in the research were enrolled. Maintaining exclusion and inclusion criteria Palliative Care was applied over 73 patients (Figure 1).
Intervention
Palliative care is a type of individual based psychological intervention given to improve the quality of life of patients who have been diagnosed with cancer. The goal of palliative care is to prevent or treat, as early as possible, the symptoms and side effects of the disease and its treatment, in addition to the related psychological, social problems. It should begin at diagnosis and continue through treatment, follow-up care, and the end of life. Addressing the side effects and emotional issues of cancer, some have a particular focus on this type of care.
A palliative care is managed the symptoms, side effects, and emotional problems experienced by patients. The goal is to maintain the best possible quality of life. Palliative care was applied only in 6 sessions and each session had taken 40-45 minutes with 15 days interval.
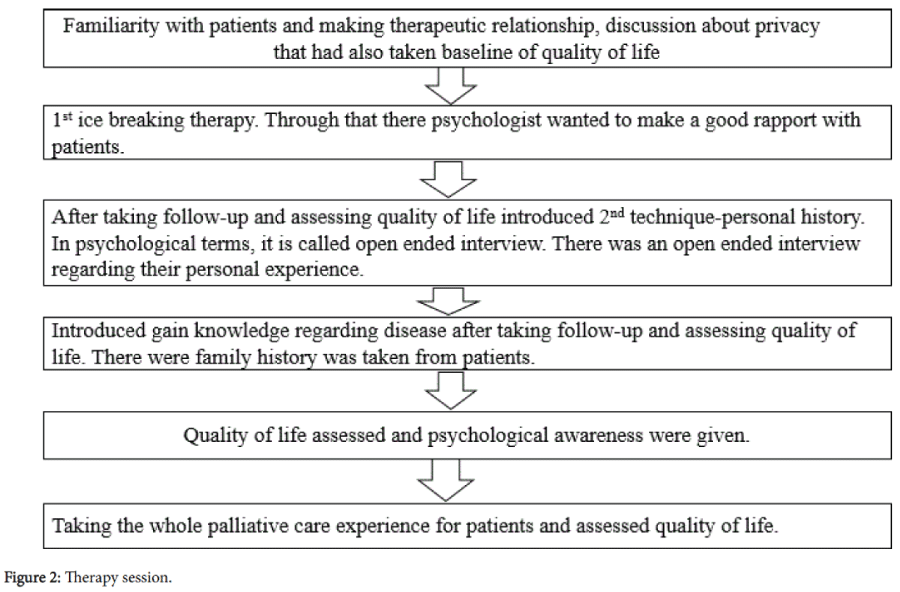
In the study; there four techniques were used, including ice breaking, personal history, gain knowledge regarding disease, psychological support. Each session had taken 40-45 minutes. Session details had been given in Figure 2.
Assessment
Quality of life is a major goal in the care of those types of patients. In addition addressing symptoms and quality of life were the most prevalent components of the PC clinic visits. Health-related quality of life was measured with the use of the Warwick-Edinburgh Mental Well-being Scale (WEMWBS) [19], which assesses dimensions of the quality of life during the previous week.
There is a 9 different types of questions were pointed from none of the time=1 to all of the time=5. These types of questions regarding what a patient thinks regarding their wellbeing life during the period of treatment.
Data collection
Data reported in this paper are all from the prospective follow-up study (baseline measurement) after having identified those, who were newly diagnosed. Structured interviews, based on the questionnaire developed for the follow-up study, were conducted by the psychologist six months after the diagnosis.
All data were reported by participants, except for age, sex, and type of cancer, which were collected from the referral list of the oncology clinic. Quality of life was measure in two way, one was on fifteen days interval to observe the effect of each technique or to observe which technique was too appropriate to a patient to evoke a better quality of life and another one was after 2 months post treatment of palliative care therapy to predict the whole treatment effect among participated patients.
Statistical analysis
WEMWBS was scored as a single item following the procedures of the scoring manual. Data was analysed with IBM SPSS package (Statistical Program for the Social Sciences, Chicago, IL), version 20 for Windows.
Ethical approved
This was approved by the Ethical Committee of our Institute, which follow the guidelines given by the Indian Council of Medical Research (ICMR).
Results
Baseline characteristics of the patients
A total of 73 patients were enrolled in the study (Figure 1). Table 1 describes the different socio demographic features of all the individuals. We found that the most of the patients were married and coming from rural areas.
| Demographic Factor | Number of participants | Quality of life before treatment | Quality of life aftertreatment | p-value (Before and after effect of Palliative care) | |||
|---|---|---|---|---|---|---|---|
| Age | |||||||
| <30 | 7% | 21.00 ± 0.00 | 23.66 ± 0.33 | 0.05 | |||
| 30-50 | 40% | 16.05 ± 0.76 | 17.57 ± 0.70 | 0.00* | |||
| 50-60 | 53% | 16.58 ± 1.28 | 19.25 ± 1.28 | 0.00* | |||
| Education | |||||||
| Below high school | 40.3% | 15.48 ± 0.82 | 17.31 ± 0.74 | 0.00* | |||
| High school | 55.6% | 16.21 ± 1.36 | 18.39 ± 1.32 | 0.00* | |||
| Graduate | |||||||
| Democracy | 50.3% | 18.73 ± 1.31 | 20.73 ± 1.34 | 00* | |||
| Rural | 6.9% | 16.50 ± 1.06 | 19.16 ± 0.98 | 0.00* | |||
| Sub urban | 43.1% | 16.62 ± 0.89 | 18.20 ± 0.88 | 0.00* | |||
| Relationship Status | |||||||
| Married | 63% | 15.91 ± 0.70 | 17.53 ± 0.64 | 0.00* | |||
| Unmarried | 7% | 15.50 ± 1.6 | 17.75 ± 1.81 | 0.05 | |||
| Widow | 30% | 18.15 ± 1.75 | 21.00 ± 1.69 | 0.00* | |||
| Occupation | |||||||
| Unemployed | 6.9% | 16.39 ± 0.78 | 18.37 ± 0.73 | 0.00* | |||
| Employed | 93.1 | 16.84 ± 0.78 | 18.82 ± 0.75 | 0.00* | |||
| Family Structure | |||||||
| Joint Family | 9.7% | 16.05 ± 0.88 | 18.00 ± 0.91 | 0.00* | |||
| Nuclear Family | 4.2% | 16.80 ± 0.88 | 18.80 ± 0.83 | 0.00* | |||
| Diagnosis | |||||||
| Female Cancer | 75% | ||||||
| Blood Cancer | 4.2% | --- | --- | --- | |||
| Lung Cancer | 5.6% | ||||||
| Other type of cancer | 15.3% | ||||||
| Values given are mean ± SD *pvalue<0.05 (compare with quality of life after giving palliative care therapy on 2months follow-up) |
|||||||
Table 1: Baseline characteristics of the study participants.
All demographic factor including age, education, democracy, occupation and relationship status were the known prognostic factor that evoke a better quality of life among patients who were enrolled in the study (Table 1).
Palliative-care visits
Significance association between demographic factors and quality of life were noticed in both pre and post psychological intervention is described in Table 1.
Table 2 describes the Quality of Life at baseline and after giving different technique of palliative care. From the data we can say that in gynaecological and other cancers increase in quality of life were seen rather than lung cancer.
| Psychological intervention | No. of Participated Patients | Quality of Life | p-value | |
|---|---|---|---|---|
| Female cancer | N= 75% | Before intervention | AfterIntervention | 0 .00* |
| 17.44 ± 5. 74 | 19.33 ± 5.74 | |||
| Lung cancer | N= 4.2% | 12 ± 2.06 | 13 ± 3.24 | 0.30 |
| Blood Cancer | N=5.6% | 16 ± 4.66 | 18.33 ± 4.33 | 0.00* |
| Other type of Cancer | N= 15.3% | 13.33 ± 3.87 | 15.33 ± 3.20 | 0.00* |
| Values given are mean ± SD *p value <0.05 (compare with quality of life after giving palliative care therapy on 2months follow-up) |
||||
Table 2: “t” test analysis of quality of life at baseline and after giving psychological intervention among different type of cancer patients.
Among the techniques of palliative care therapy it has been seen that Ice breaking was significantly associated with personal history (p=0.01), and psychological support (p=0.4) (Table 3).
| Psychological intervention | Total number of Participants | Personal history | Gain knowledge regarding disease | Psychological Support | ||||||
|---|---|---|---|---|---|---|---|---|---|---|
| participate | Not participated | p- value | participate | Not participated | p- value | participate | Not participated | p- value | ||
| Ice breaking | 75% | 81.90% | 18.10% | 0.01* | 88.90% | 11.10% | 0.5 | 95.80% | 4.20% | 0.04* |
| Psychological intervention | Total number of Participants | Gain knowledge regarding disease | Psychological Support | |||||||
| participate | Not participated | p- value | participate | Not participated | p- value | |||||
| Personal History | 81.90% | 88.90% | 11.10% | 0.16 | 95.80% | 4.20% | 0.41 | |||
| Psychological intervention | Total number of Participants | Psychological Support | ||||||||
| Gain knowledge regarding disease | participate | Not participated | p-value | |||||||
| 88.90% | 95.80% | 4.20% | 0.53 | |||||||
Table 3: Intra correlation among techniques of palliative care.
On the basis of the demographic factors among participates in palliative care therapy it can be said that there education plays a significant role especially in the sessions of ice breaking (p=.00), gain knowledge regarding disease (p=.02) and psychological support (p=. 03) (Table 4). Before and after scores of the quality of life was significantly associated with each and every session of palliative care with fifteen days interval (Table 5). In Table 6 we are describing the percentage of participants attending different stages of Palliative Care. Findings suggest that, gynecological cancer and other groups are more responsive than blood cancer or lung cancer.
| Demographic Factor | Number of participants | Ice Breaking | Personal History | Gain Knowledge regarding disease | Psychological support | ||||
|---|---|---|---|---|---|---|---|---|---|
| Age | Participants | p-value | Participants | p-value | Participants | p-value | Participants | p-value | |
| <30 | (7%) | 7% | 7% | 7% | 7% | ||||
| 30-50 | 40 (54.79%) | 30 (75%) | 0.34 | 28 (70%) | 0.138 | 28 (70%) | 0.00* | 26 (65%) | 0.10 |
| 50-60 | 39 (53%) | 36 (92.31%) | 30 (76.92%) | 30 (76.92%) | 24 (61.54%) | ||||
| Education | |||||||||
| Below high school | 30 (40.3%) | 24 (80%) | 0.00* | 27 (90%) | 0.080 | 29 (96.67%) | 0.02* | 28 (93.33%) | 0.03* |
| High school | 41 (55.6%) | 40 (97.16%) | 39 (95.12%) | 38 (92.68%) | 40 (97.16%) | ||||
| Graduate | 3 (4.1%) | 3 (4.1%) | 3 (4.1%) | 3 (4.1%) | 3 (4.1%) | ||||
| Democracy | |||||||||
| Rural | 37(50.3%) | 35 (94.59%) | 0.26 | 36 (97.3%) | 0.075 | 34 (91.89%) | 0.32 | 34 (91.89%) | 0.34 |
| Urban | 36 (50%) | 36 (100%) | 33 (91.67%) | 34 (94.44%) | 36 (100%) | ||||
| Relationship Status | |||||||||
| Married | 46 (63%) | 44 (95.65%) | 43 (93.48%) | 40 (86.96%) | 42 (91.30%) | ||||
| Unmarried | 5 (7%) | 5 (100%) | 0.12 | 5 (100%) | 0.138 | 5 (100%) | 0.00* | 3 (60%) | 0.09 |
| Widow | 22 (30%) | 21 (95.45%) | 19 (86.36%) | 20 (90.90%) | 17 (77.27%) | ||||
| Occupation | |||||||||
| Housewife | 68 (93.1%) | 65 (95.59%) | 65 (95.59%) | 62 (91.18%) | 64 (94.12%) | ||||
| Employed | 5 (6.9%) | 5 (100%) | 0.10 | 5 (100%) | 0.119 | 5 (100%) | 0.49 | 5 (100%) | 0.08 |
| Family Structure | |||||||||
| Joint Family | 7 (9.7%) | 7 (100%) | 0.39 | 5 (71.42%) | 0.246 | 6 (85.71%) | 0.28 | 7 (100%) | 0.31 |
| Nuclear Family | 66 (90.41%) | 65 (98.48%) | 64 (98.46%) | 63 (96.92%) | 64 (98.46%) | ||||
| Values given are mean ± SD *p value <0.05 (compare with quality of life after giving palliative care therapy on 2months follow-up) |
|||||||||
Table 4: Baseline characteristics of participants in the session of psychological intervention.
| Psychological Intervention | Quality of life before treatment | Quality of life after treatment | p-value | ||||
|---|---|---|---|---|---|---|---|
| Mild (%) | Moderate (%) | Severe (%) | Mild (%) | Moderate (%) | Severe (%) | Before after effect of psychological intervention | |
| Ice Breaking | 69.4 | 23.6 | 6.9 | 72.2 | 20.8 | 6.9 | |
| Personal history | 76.4 | 18.1 | 5.6 | 73.6 | 20.8 | 5.6 | 0 .00* |
| Gain knowledge regarding disease | 35.4 | 18.1 | 5.6 | 73.6 | 20.8 | 5.6 | 0 .00* |
| Psychological support | 47.2 | 38.9 | 13.9 | 12.5 | 61.1 | 26.4 | 0.00* |
| Values given are mean±SD *p value <0.05 (compare with quality of life after giving each technique of palliative care therapy on 15 days follow-up) |
|||||||
Table 5: Distribution of psychological treatment and quality of life after treatment of participated.
| Diagnosis | Number of Participates | Palliative Care | |||||||
|---|---|---|---|---|---|---|---|---|---|
| Female type of Cancer | 75% | Ice breaking (75%) | Personal History (81%) | Gain Knowledge Regarding Disease (88%) | Psychological Support (95%) | ||||
| No. of Participants | Giving Follow-up | No. of Participants | Giving Follow-up | No. of Participants | Giving Follow-up | No. of Participants | Giving Follow-up | ||
| 51% | 48% | 46% | 46% | 43% | 42.8% | 40% | 40% | ||
| Blood Cancer | 4.2% | 3% | 3% | 3% | 2.8% | 3% | 2.2% | 3% | 2.2% |
| Lung Cancer | 5.6% | 4.8% | 4.8% | 4% | 4% | 4% | 3.8% | 3.8% | 1.5% |
| Other Type of Cancer | 15.3% | 11% | 10.7% | 7% | 6.8% | 5% | 5% | 5% | 4.3% |
Table 6: Percentage of participants in different sessions of Palliative care.
Quality-of-life outcomes
A comparison of measures of quality of life at 2 months of post treatment showed that the patients assigned to early palliative care had significantly higher scores than pre-treatment did assign to Palliative care (Table 7).
| Quality of Life before giving psychological intervention | After giving psychological intervention Quality of Life | p-value | 95% Confidence Interval ofDifference | ||||
|---|---|---|---|---|---|---|---|
| Mild | Moderate | Severe | Mild | Moderate | Severe | 0.00* | 15.23-17.68 |
| 5(6.9%) | 47 (65.4%) | 20 (27.7%) | 2 (2.8%) | 47 (65.4%) | 24 (32.1%) | ||
| *p value <0.05 (compare with quality of life after giving palliative care therapy on 2months follow-up) | |||||||
Table 7: Before and after effect of Palliative care among follow-up patients.
Discussion
There are different previous research had worked based on palliative care therapy and its effect over quality of life among cancer patients, for example, Jennifer et.al. 2010 had worked over metastatic non– small-cell lung cancer patients to receive either early palliative care integrated with standard oncology care or standard oncology care alone. Quality of life and mood were assessed at baseline and at 12 weeks with the use of the Functional Assessment of Cancer Therapy– Lung (FACT-L) scale and the Hospitalized Anxiety and Depression Scale, respectively. After giving therapy they had predicted the primary outcome was the change in the quality of life at 12 weeks [20]. However, there have not found much study or comparisons of the techniques researchers have followed in the present study.
The major goal of the study was to clarify difference between the effect of palliative care on scores of quality of life and participants’ demographic status. Sociodemographically it had been seen that 30-50 years age group of participants’ frequency were higher rather than other age group. From that, means those age groups of patients more convinced to participate in this psychological intervention and that’s why among them quality of life was more significantly improved after two months of post reatment.55.6% patients, those were high school educated, they themselves want to attain this psychological intervention, but sometime their physical condition did not support them to follow the session. In residential graph can be said urban people were more interested to attain this intervention and more concerned regarding psychological counselling. Those were married there had been seen an unexpected strong wish to live not for herself, but for their family and they themselves want to share their experience which got throughout the treatment. Family structure did not make any effect over participation among patients. Though there participated patients were mainly female, the number of housewives was higher than other type of occupation. The In case of type of cancer, there had been seen that gynaecological cancer patients’ frequency was higher rather than another type of cancer patients. From that point of view it could be said one of the strong findings of the study is that it considered demographic variables as separate variables (participants’ educational level, marital status, residence and occupational status) that evokes patients’ quality of life. Also their participation in psychological intervention significantly varies with these factors.
Palliative care was applied only in 6 sessions and each session had taken 40-45 minutes with 15 days interval. In our country, people with less information, relates 'psychology' with mental problems. That is why, if the psychologist introduced psychological treatment in a different way, like saying that, "we have come here to spend quality time with you that you won't feel boring" gives more encouragement to them. For that reason participation among cancer patients were high in this study. Ice breaking was a short game which was used as a 1st technique. This game was about solving a puzzle as soon as possible. Patients enjoyed this game and their response was "O my God! It’s a baby's game!" On the other hand, this technique was used to make a good rapport with patients that evoke a better quality of life. Next was Personal history. Here patients share their experience of both positive and negative shades of life. Patients were asked if they have any relative or friend being diagnosed with cancer. This question was asked as it impacts the patient's life. The negative sides of 'cancer' come into their thought repetitively and as a result patients become more anxious. They share these experiences during personal history technique and we get a chance to interpret those experiences in a right direction. As a result patient's quality of life improves to a degree (Table 5). One of the factors which hinder the improvement of the patient's life is social factor. They say," I haven't informed anyone yet. You know that its village area and I have a daughter to get married, if I won't be able to arrange it, what will happen?" Third one was gaining knowledge regarding the disease. Here each and every patient was given a brief explanation of the type of cancer they had been diagnosed with, especially the side effects of chemotherapy, treatment plan, and treatment duration. Last one was psychological support. In this technique patient's history of anxiety and depression was taken. For example-how many times patients feel more irritable or not, how do they feel in daily life, cause of tension, what is type of thoughts is going on in their mind, etc. patients got each and every information starting from a type of cancer diagnosis to clarification of the causes and symptoms of anxiety and depression during treatment. Even if they feel anxious at that moment, they got instructions to overcome the situation, though many times patients could not follow this due to physiological deterioration. They said," We know, nothing is going to change even if we think too much it affect our physical condition. Many people advise not to think continuously, but it comes automatically". Patients’ quality of life was shown much improvement after applying this technique.
In subtypes of Palliative care, it was seen that personal history and psychological support had significant association with ice breaking. However, a patient will explain all of his/her problems, if there is a good relation and rapport establish (happen) in ice breaking technique. From that point of view, it might be said that if there is no good rapport establishment between patient and psychologist, psychological treatment won't be successful.
From the statistical analysis it had been found that all the techniques of the palliative care helped a patient to live in a better quality of life (Table 5) as well as percentage of follow-up patients were high (Table 6). This result proved that during the period of this therapy all patients enjoyed very much as well as they was able to follow all the session of this psychological intervention. For that reason quality of life was improved among all age group of cancer patients (Table 4). But, diagnostically if it had been pointed out after giving psychological intervention quality of life was not improved among lung cancer patients (Table 2) due to their physical condition, because those type of patients came to hospital at last stage an in that condition it was too difficult to them to follow this therapy. It had been found that a patient’s quality of life depends over how much they know regarding their disease. So, it can be said that if patients were given the proper knowledge regarding disease, e.g. what type of disease, treatment plan, duration and side effects of treatment, then it would be easier to cope up with symptoms that leads to decrease anxiety.
As a whole patient was reported quality of life significantly improved on 2 months of post treatment (Table 7). From that point of result it had been said that patients accepted palliative care more easily that might be reflected in the pre and post assessment scores of quality of life. This finding is supported by the study of Jennifer S. et.al. They had presented that among patients with metastatic non–small cell lung cancer, early palliative care led to significant improvements in both quality of life and mood. As compared with patients receiving standard care, patients receiving early palliative care had less aggressive care at the end of life but longer survival [20]. Improving quality of life in patients with cancer is a formidable challenge, given the progressive nature of the illness [21]. The improvement we observed in the quality of life among patients assigned to early palliative care as indicated by a mean change on 2 monthsfollowup is similar to the improvement in the quality of life that has been reflected among patients who have a response to cisplatin-based chemotherapy [22]. Most studies show that there is deterioration in the quality of life over time, which is consistent with the results in our study [23-25]. One study with sufficient power to examine quality-of-life outcomes showed that among patients receiving chemotherapy as well as radiation therapy, a multidisciplinary intervention focused on education, psychological support, resulted in improvements in the quality of life [26]. A recent study showed that Project ENABLE (Educate, Nurture, Advise, Before Life Ends), a telephone-based, psychoeducational program for patients with advanced cancer, significantly improved both quality of life and mood [27]. However, the percentage of patients who completed the study assessments was somewhat low, and the study did not use a traditional palliative care model.
Conclusion
Early integration of palliative care for patients with cancer is a clinically meaningful and feasible care model that has effects on quality of life. As compared with the study participants who received gain knowledge regarding disease had improved quality of life. Although study findings must be replicated in a variety of care settings and cancer populations, the results nonetheless offer great promise for alleviating distress in patients with cancer and addressing critical concerns regarding the use of health care services at the end of life.
Acknowledgements
We wish to acknowledge patients and their family members for their extensive cooperation and participation in the study. We would also like to thank all the staff at our hospital that helped to accomplish the study successfully. We are also most grateful to Miss Moupiya Ghosh and Mrs. Nabamita Paul for the help and support given by the academic leads.
Conflict of Interest
There is no conflict of interest.
References
- Kim HN, Bruera E, Jenkins R (2004) Symptom control and palliative care. In:Cavalli F, Hanse HH, Kaye SB. Textbook of Medical Oncology. Third Edition. Oxfordshire, UK: Taylor & Francis Group pp: 353-370.
- Wilson KG, Graham ID, Viola RA, Chater S, de Faye BJ, et al. (2004) Structured interview assessment of symptoms and concerns in palliative care.Can J Psychiatry 49: 350-358.
- Zhukovsky DS, Abdullah O, Richardson M, Walsh D (2000) Clinical evaluation in advanced cancer.SeminOncol 27: 14-23.
- Jenkins CA, Schulz M, Hanson J, Bruera E (2000) Demographic, symptom, and medication profiles of cancer patients seen by a palliative care consult team in a tertiary referral hospital. J Pain Symptom Manage 19: 174-184.
- Vachon ML, Kristjanson L, Higginson I (1995) Psychosocial issues in palliative care: the patient, the family, and the process and outcome of care.J Pain Symptom Manage 10: 142-150.
- Bruera E, Neumann C, Brenneis C, Quan H (2000) Frequency of symptom distress and poor prognostic indicators in palliative cancer patients admitted to a tertiary palliative care unit, hospices, and acute care hospitals.J Palliat Care 16: 16-21.
- Morrison RS, Penrod JD, Cassel JB, Caust-Ellenbogen M, Litke A, et al. (2008) Palliative Care Leadership Centers' Outcomes Group8. Cost savings associated with US hospital palliative care consultation programs. Arch Intern Med 168:1783-1790.
- Morita T, Akechi T, Ikenaga M, Kizawa Y, Kohara H, et al. (2005) Late referrals to specialized palliative care service in Japan.J ClinOncol 23: 2637-2644.
- Zimmermann C, Riechelmann R, Krzyzanowska M, Rodin G, Tannock I (2008) Effectiveness of specialized palliative care: a systematic review.JAMA 299: 1698-1709.
- Donnelly S, Walsh D (1995) The symptoms of advanced cancer.SeminOncol 22: 67-72.
- Weitzner MA, Moody LN, McMillan SC (1997) Symptom management issues in hospice care.Am J HospPalliat Care 14: 190-195.
- Stark L, Tofthagen C, Visovsky C, McMillan SC (2012) The Symptom Experience of Patients with Cancer.J HospPalliatNurs 14: 61-70.
- Kurtz ME, Kurtz JC, Given CW, Given B (1993) Loss of physical functioning among patients with cancer: a longitudinal view.Cancer Pract 1: 275-281.
- McMillan SC, Weitzner M (1998) Quality of life in cancer patients: use of a revised Hospice Index.Cancer Pract 6: 282-288.
- Berger AM, Shuster JL,Von Roenn JH (2006) Principles and practice of palliative care and supportive oncology: Lippincott Williams & Wilkins.
- Singh DP (2010) Quality of life in cancer patients receiving palliative care.Indian J Palliat Care 16: 36-43.
- Gupta S, Goel S (2014) Present scenario of palliative care for cancer patients in India. J of Case Repin Oncol& Therapy 1:01016.
- Khosla D, Patel FD, Sharma SC (2012) Palliative care in India: current progress and future needs.Indian J Palliat Care 18: 149-154.
- Feros DL, Lane L, Ciarrochi J, Blackledge JT (2013) Acceptance and Commitment Therapy (ACT) for improving the lives of cancer patients: a preliminary study.Psychooncology 22: 459-464.
- Temel JS, Greer JA, Muzikansky A, Gallagher ER, Admane S (2010) Early Palliative Care for Patients with Metastatic Non–Small-Cell Lung Cancer. N Engl J Med 363:733-742.
- Brown J, Thorpe H, Napp V, Fairlamb DJ, Gower NH, et al. (2005) Assessment of quality of life in the supportive care setting of the big lung trial in non-small-cell lung cancer.J ClinOncol 23: 7417-7427.
- Cella D, Eton DT, Fairclough DL, Bonomi P, Heyes AE, et al. (2002) What is a clinically meaningful change on the Functional Assessment of Cancer Therapy-Lung (FACT-L) Questionnaire? Results from Eastern Cooperative Oncology Group (ECOG) Study 5592. J ClinEpidemiol55:285-295.
- Bonomi P, Kim K, Fairclough D, Cella D, Kugler J, et al. (2000) Comparison of survival and quality of life in advanced non-small-cell lung cancer patients treated with two dose levels of paclitaxel combined with cisplatin versus etoposide with cisplatin: results of an Eastern Cooperative Oncology Group trial. J ClinOncol18:623-631.
- Langer CJ, Manola J, Bernardo P, Kugler JW, Bonomi P (2002) Cisplatin-based therapy for elderly patients with advanced non-small-cell lung cancer: implications of Eastern Cooperative Oncology Group 5592, a randomized trial. J Natl Cancer Inst94:173-181.
- Sandler AB, Nemunaitis J, Denham C, von Pawel J, Cormier Y, et al. (2000) Phase III trial of gemcitabine plus cisplatin versus cisplatin alone in patients with locally advanced or metastatic non-small-cell lung cancer.J ClinOncol 18: 122-130.
- Rummans TA, Clark MM, Sloan JA, Frost MH, Bostwick JM, et al. (2006)Impacting quality of life for patients with advanced cancer with a structured multidisciplinary intervention: a randomized controlled trial. J ClinOncol24:635-642.
- Bakitas M, Lyons KD, Hegel MT, Balan S, Brokaw FC, et al. (2009) Effects of a palliative care intervention on clinical outcomes in patients with advanced cancer: the Project ENABLE II randomized controlled trial.JAMA 302: 741-749.
Relevant Topics
- Caregiver Support Programs
- End of Life Care
- End-of-Life Communication
- Ethics in Palliative
- Euthanasia
- Family Caregiver
- Geriatric Care
- Holistic Care
- Home Care
- Hospice Care
- Hospice Palliative Care
- Old Age Care
- Palliative Care
- Palliative Care and Euthanasia
- Palliative Care Drugs
- Palliative Care in Oncology
- Palliative Care Medications
- Palliative Care Nursing
- Palliative Medicare
- Palliative Neurology
- Palliative Oncology
- Palliative Psychology
- Palliative Sedation
- Palliative Surgery
- Palliative Treatment
- Pediatric Palliative Care
- Volunteer Palliative Care
Recommended Journals
- Journal of Cardiac and Pulmonary Rehabilitation
- Journal of Community & Public Health Nursing
- Journal of Community & Public Health Nursing
- Journal of Health Care and Prevention
- Journal of Health Care and Prevention
- Journal of Paediatric Medicine & Surgery
- Journal of Paediatric Medicine & Surgery
- Journal of Pain & Relief
- Palliative Care & Medicine
- Journal of Pain & Relief
- Journal of Pediatric Neurological Disorders
- Neonatal and Pediatric Medicine
- Neonatal and Pediatric Medicine
- Neuroscience and Psychiatry: Open Access
- OMICS Journal of Radiology
- The Psychiatrist: Clinical and Therapeutic Journal
Article Tools
Article Usage
- Total views: 10567
- [From(publication date):
June-2016 - Apr 02, 2025] - Breakdown by view type
- HTML page views : 9657
- PDF downloads : 910