Research Article Open Access
A Population-based Anaemia Screening using Point-of-care in Estimating Prevalence of Anaemia in Malaysian Adults: Findings from a Nationwide Survey
Awaluddin SM*, Ahmad NA, Naidu BM, Mohamad MS, Yusof M, Razak MA, Salleh R, Mohd Yusoff MF and Aris TInstitut Kesihatan Umum, Kuala Lumpur, Malaysia
- *Corresponding Author:
- S Maria Awaluddin, MD
Medical Officer, Institute for Public Health
National Institutes of Health, Ministry of Health Malaysia
Jalan Bangsar, 50590, Kuala Lumpur, Malaysia
Tel: +603-22979580
Fax: +603-22823114
E-mail: smaria@moh.gov.my
Received date: March 11, 2017; Accepted date: March 27, 2017; Published date: March 29, 2017
Citation: Awaluddin SM, Ahmad NA, Naidu BM, Mohamad MS, Yusof M, et al. (2017) A Population-based Anaemia Screening using Point-ofcare in Estimating Prevalence of Anaemia in Malaysian Adults: Findings from a Nationwide Survey. J Community Med Health Educ 7:513. doi: 10.4172/2161-0711.1000513
Copyright: © 2017 Awaluddin SM, et al. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.
Visit for more related articles at Journal of Community Medicine & Health Education
Abstract
Background: Anaemia is one of the most common public health problems. Globally, the most affected group is women of reproductive age. This study aims to describe the prevalence of anaemia among Malaysian adults.
Methods: Data were obtained from the National Health and Morbidity Survey 2015, a population-based study. This study used a cross-sectional design with a nationally representative sample. Respondents aged 15 years and above from the selected livings quarters and who gave their consent, were recruited in this study. Haemoglobin level was measured using HemoCue® Hb 201+ System© point-of-care testing based on capillary blood sample. Data analysis was conducted using IBM SPSS software version 21 taking into consideration the complex sampling design.
Results: There were 19,908 out of 21,445 respondents who participated in this study. The response rate towards point-of-care screening method was good except for those of young age and Chinese ethnicity. The overall prevalence of anaemia was 24.16% (95% CI: 23.16-25.19) with an estimated projection to 4,858,646 people. The prevalence of anaemia for the specific groups were 34.75% (95% CI: 33.09-36.46), 34.67% (95% CI: 33.02-36.37), 35.27% (95% CI 33.15-37.45) for non-pregnant women (15-49), women of reproductive age and older adults (≥ 60) respectively. Anaemia was positively associated with female sex (aOR=2.84; 95% CI: 2.62-3.07), Indian ethnicity (aOR=1.54; 95% CI: 1.31-1.80), those who were currently not working (aOR=1.11; 95% CI: 1.02-1.20) and age (aOR: 1.01; 95% CI: 1.00-1.01).
Conclusion: Anaemia is a significant health problem that should be monitored periodically especially among women of reproductive age and the elderly. Preventive measures such as iron supplementation should thus be started from the younger population.
Keywords
Prevalence; Anaemia; Point-of-care testing; Populationbased study; Malaysia
Introduction
Anaemia has been recognized as one of the significant public health concerns as it is associated with many other complications or health problems among the population and contributes to the economic burden by virtue of high healthcare cost [1,2]. The commonest type of anemia is due to iron deficiency while other nutritional deficiencies such as vitamin B12, folate and vitamin A contribute much lesser compared to iron. Other causes for anaemia are chronic diseases, parasitic infections and inherited disorders [3]. By definition, anaemia is a condition where there is insufficiency of normal red blood cells to meet the human body needs [4]. It may present with general symptoms such as fatigue, weakness and poor concentration. The condition of anemia could be recognized clinically by trained staff. However, symptomatic patients usually present to healthcare clinics with very severe anaemia status as mild anaemia is usually asymptomatic. Mild anaemia is frequently detected accidently following laboratory investigation for other diseases [5]. Almost all of the population age groups are affected by anaemia from newborn to older age. In pregnant mothers, anaemia increases risk of maternal morbidity in which it presents with adverse pregnancy outcomes such as preterm labour and low birth weight among newborns [6]. Nonetheless, elderly are also affected by anaemia and the majority is due to nutritional deficiencies and anaemia of chronic disease while one third remains unexplained [7].
A previous study conducted by the World Health Organization (WHO) estimating global anaemia prevalence from 1993 to 2005 as a part of the Vitamin and Mineral Nutrition Information System observed that a quarter of the world’s populations were affected, involving 1.6 billion people [8]. Although the most affected group was non-pregnant women of reproductive age, the younger age group and elderly were also affected. The highest prevalence of anemia in nonpregnant women was observed in Africa (47.5%) and in South-East Asia (35.7%) while the lowest was 17.8% in the Americas [8]. Malaysia was also included in the project and the anaemia prevalence among pregnant women and non-pregnant women was 38.3% and 30.1% respectively [8]. The WHO has defined the standardized hemoglobin cut-off point to diagnose anaemia which can be used globally (4). As most of the anaemia causes are treatable conditions, early detection can help stakeholders provide a prompt intervention. Mass screening is one of the methods to detect more cases of anaemia in the population. Point-of-care has been established as a screening tool with minimally invasive procedure that can generate more data on global estimation in worldwide surveys like the Demographic Health Survey Program conducted by the United States Agency for International Development (USAID) [9].
Anaemia routine screening in the local setting is only conducted during blood donation programs and antenatal check-ups for pregnant mothers. Most of the time, the blood investigation for hemoglobin concentration is opportunistic, conducted when patients come to health clinics for other problems or during voluntary annual check-ups for those who are covered with health care schemes at the work place or through personal insurance services. Thus, there were limited data to explain on the anaemia situation in Malaysia as previous studies were more focused towards pregnant women [10,11]. This study aimed to present the current prevalence of anaemia in Malaysian adults. It also estimated the number of persons affected in specific age groups and the socio-demographic factors that are associated with anaemia. To the best of our knowledge, this is the first population-based survey using a point-of care screening method to detect anaemia.
Materials and Methods
Data were obtained from the National Health and Morbidity Survey (NHMS) 2015. NHMS is conducted regularly to provide populationbased data on the pattern of common diseases, health needs and expenditure in Malaysia. In the year 2015, the NHMS cycle focused on non-communicable diseases and its risk factors besides other topics, including anaemia. This survey obtained approval from the Medical Research and Ethics Committee (MREC), Ministry of Health and was registered with the National Medical Research Registration with the NMRR ID–14-1064-21877. Further details of the methodology of this study have been described in the technical report [12].
Population and sampling
This survey used a stratified multistage random sampling based on the national census to ensure national representativeness. The primary sampling units were the enumeration blocks, arbitrarily defined geographically contiguous areas, and the secondary sampling units were the living quarters (LQs). Respondents aged 15 years and above from the selected LQs, who gave their consent, were recruited in this study.
Instruments and training
The socio-demographic data were collected using validated questionnaires including pregnancy status for female respondents although this survey was not targeting pregnant women. Haemoglobin level was measured using the HemoCue haemoglobinometer (HemoCue® Hb 201+ System, Angelhom, Sweden), a point-of-care testing on capillary blood samples by trained health staff. HemoCue® Hb 201+ System has been widely used in the local primary care setting. Practical sessions had been conducted during five days of data collection training including the right technique in obtaining capillary samples. Health staff was taught that respondents should be seated appropriately and explanation on finger prick procedure should be given before conducting the procedure. Health staff was advised to adhere to the safety procedure and standard clinical waste disposal during the data collection period.
Variables definition
The socio-demographic variables included in this study were age group, strata, ethnicity, education level, marital status, working status and household income quintile. Anaemia status and level of severity were determined according to the WHO guidelines on definition of haemoglobin cut-off point [4]. Haemoglobin level below 12 g/dl was considered anaemia for non-pregnant women while for men age 15 years and above, it was below 13 g/dl whereas pregnant women were subjected to a cut-off point of below 11 g/dl.
Statistical analysis
Data analysis was conducted using IBM SPSS Statistics for Windows, Version 21.0 software taking into consideration the complex sampling design for population estimation. Multivariate logistic regression was used to investigate the association between anaemia status and socio-demographic variables. The findings are presented as adjusted odd ratios (aORs) with 95% confidence intervals (CI), and a p-value <0.05 was considered significant.
Results
A total of 10,428 LQs were selected and 9433 were the eligible LQs for this survey. Out of the eligible LQs, 8411 heads of households completed the Household Survey yielding a 89.2% response rate. There were 19,908 out of 21,455 adult respondents who participated in this anaemia study which further gave a 92.8% response rate at the individual level. Based on the ethnicity breakdown as Malaysia is a multi-ethnic country, the three major ethnicities were Malays, Chinese and Indians. Further breakdown of the response rate according to the specific socio-demographic groups are shown in Table 1. Eligible
| Eligible Respondents in Successful LQs (n) | Responded to Anaemia Screening (n) | Individual Response Rate (%) | EstimatedPopulation | n | Prevalence (%)* | (95% CI)# | |
| Overall individual | 21,455 | 19,908 | 92.8 | 4,858,646 | 5,331 | 24.2 | (23.2-25.2) |
| Age Group | |||||||
| 15-19 | 2,291 | 2,026 | 88.4 | 497,745 | 469 | 21.4 | (19.3-23.7) |
| 20-59 | 15,360 | 14,327 | 93.3 | 3,509,512 | 3,551 | 22.8 | (21.7-23.9) |
| 60 and above | 3,794 | 3,556 | 93.7 | 851,389 | 1,311 | 35.3 | (33.2-37.5) |
| Gender | |||||||
| Male | 10,220 | 9,433 | 92.3 | 1,496,556 | 1,646 | 14.4 | (13.4-15.5) |
| Female | 11,225 | 10,475 | 93.3 | 3,362,090 | 3,685 | 34.5 | (33.1-36.0) |
| Ethnicity | |||||||
| Malays | 13,345 | 12,476 | 93.5 | 2,540,886 | 3,368 | 25.3 | (24.0-26.6) |
| Chinese | 3,407 | 2,983 | 87.6 | 1,002,533 | 747 | 22.8 | (20.8-24.9) |
| Indians | 1,519 | 1,401 | 92.2 | 422,352 | 478 | 30.8 | (28.0-33.8) |
| Other Bumi’s | 1,891 | 1,833 | 96.9 | 543,160 | 479 | 23.4 | (20.4-26.6) |
| Others(non-citizen) | 1,283 | 1,215 | 94.7 | 349,715 | 259 | 17.7 | (15.5-20.8) |
| Working status | |||||||
| Currently working | 12312 | 11476 | 93.2 | 2,559,659 | 2,567 | 20.5 | (19.4-21.6) |
| Currently not working | 5783 | 5360 | 92.7 | 1,477,029 | 1,673 | 29.4 | (27.5-31.3) |
| Level of education | |||||||
| No Formal Education | 1,694 | 1,580 | 93.3 | 421,020 | 536 | 29.0 | (26.0-32.2) |
| Primary | 5,015 | 4,740 | 94.5 | 1,035,991 | 1,395 | 25.3 | (23.5-27.1) |
| Secondary | 10,294 | 9,551 | 92.8 | 2,282,959 | 2,405 | 23.3 | (22.0-24.7) |
| Tertiary | 4,403 | 4,027 | 91.5 | 1,117,633 | 992 | 23.5 | (21.8-25.3) |
| Marital status | |||||||
| Never married | 5,645 | 5,092 | 90.2 | 1,251,795 | 1,081 | 19.2 | (17.7-20.7) |
| Married | 13,845 | 12,993 | 93.8 | 3,137,627 | 3,539 | 25.6 | (24.4-26.7) |
| Widow/Widower/Divorcee | 1,941 | 1,823 | 93.9 | 469,225 | 711 | 36.1 | (33.0-39.4) |
| HH income group | |||||||
| Q1 (lowest) | 2,978 | 2,748 | 92.3 | 659,730 | 903 | 28.2 | (25.9-30.6) |
| Q2 | 4,008 | 3,756 | 93.7 | 838,966 | 1,008 | 24.1 | (22.1-26.3) |
| Q3 | 4,661 | 4,325 | 92.8 | 930,898 | 1,108 | 22.3 | (20.5-24.2) |
| Q4 | 4,431 | 4,095 | 92.4 | 1,074,784 | 1,091 | 24.6 | (22.8-26.5) |
| Q5 (highest) | 5,367 | 4,984 | 92.9 | 1,354,267 | 1,221 | 23.6 | (21.8-25.5) |
| Strata | |||||||
| Urban | 12,369 | 11,307 | 91.4 | 3,652,347 | 2,931 | 24.2 | (23.0-25.5) |
| Rural | 9,076 | 8,601 | 94.8 | 1,206,299 | 2,400 | 23.9 | (22.5-25.5) |
| *Prevalence was calculated with considering for complex sample design; #95% Confidence Interval; Subtotal are not consistent because of missing data | |||||||
Table 1: Individual response rate for the haemoglobin point-of-care testing in a household setting and the prevalence of anaemia in Malaysian adults according to socio-demographic characteristic: NHMS 2015.
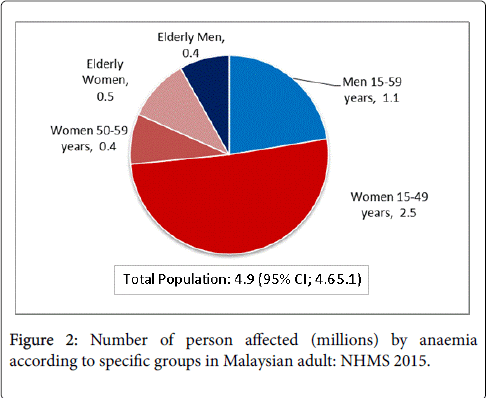
The national prevalence of anaemia was 24.16% (95% CI: 23.16-25.19) which can be estimated further to nearly 5 million people. In terms of level of severity of anaemia according to the WHO classification, the prevalence is divided further into three categories which were mild anaemia (15.57%; 95% CI: 14.83-16.33), moderate anemia (7.63%; 95% CI: 7.091-8.21) and severe anaemia (0.97%; 95% CI: 0.78-1.20).
The estimation of anaemia prevalence according to sociodemographic groups is also shown in Table 1.
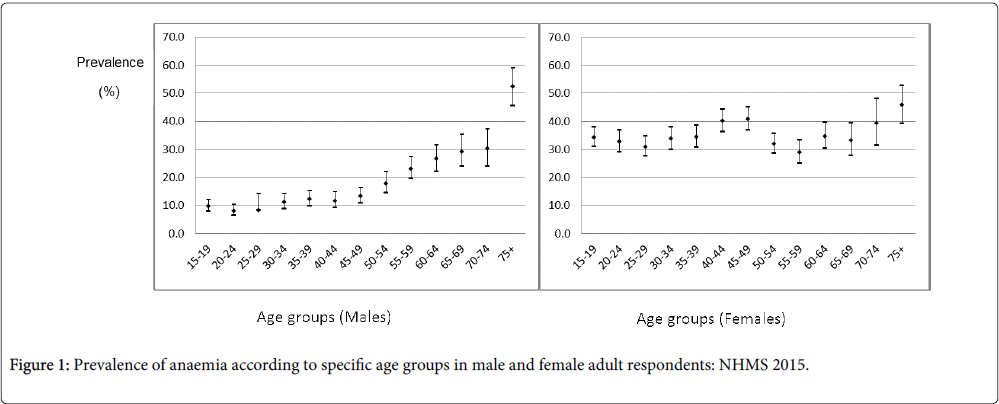
Elderly had the highest prevalence of anaemia of 35.27% (95% CI 33.15-37.45) among the age groups. Females (34.50%; 95% CI: 33.08-35.96) had a significantly higher prevalence of anaemia compared to males (14.44%; 95% CI: 13.42-15.52). Figure 1 shows the pattern of anaemia prevalence between the specific age groups and gender. The prevalence of anaemia among women aged 15 to 49 years was 34.67% (95% CI: 33.02-36.37) and for the non-pregnant women was 34.75% (95% CI: 33.09-36.46).
The prevalence of anaemia among females 15 to 19 years was significantly higher compared to males in the same age (34.14%; 95% CI: 30.71-37.75 vs. 9.62%; 95% CI: 7.74-11.89). In terms of ethnicity, Indians (30.84%, 95% CI: 28.03-33.79) had the highest prevalence of anaemia compared to other ethnicities.
Table 2 shows the association between the socio-demographic variables and prevalence of anaemia in Malaysian adults after adjustment for age, gender, ethnicity, working status, level of education, household income quintile and strata. Anaemia was positively associated with females (adjusted odds ratio [aOR]=2.84; 95% CI: 2.62-3.07), Indian ethnicity (aOR=1.54; 95% CI: 1.31-1.80), those who were currently not working (aOR=1.11; 95% CI: 1.02-1.20) and age (aOR=1.01; 95% CI: 1.00-1.01).
| Variables | Crude OR | (95% CI) | Wald Test | df | Adjusted OR# | (95% CI) | p- value | ||
| Lower | Upper | Lower | Upper | ||||||
| Age | 1.02 | 1.01 | 1.02 | 44.63 | 1 | 1.01 | 1.00 | 1.01 | 0.000 |
| Gender | |||||||||
| MaleRef | 1.00 | - | - | - | - | 1.00 | - | - | |
| Female | 2.57 | 2.40 | 2.74 | 643.19 | 1 | 2.84 | 2.62 | 3.07 | 0.000 |
| Ethnicity | |||||||||
| ChineseRef | 1.00 | - | - | - | - | 1.00 | - | - | |
| Malays | 1.11 | 1.01 | 1.21 | 2.61 | 1 | 1.09 | 0.98 | 1.22 | 0.106 |
| Indians | 1.55 | 1.35 | 1.78 | 27.95 | 1 | 1.54 | 1.31 | 1.80 | 0.000 |
| Other bumi’s | 1.06 | 0.93 | 1.21 | 0.03 | 1 | 1.02 | 0.86 | 1.19 | 0.855 |
| Others | 0.81 | 0.69 | 0.95 | 0.98 | 1 | 0.91 | 0.75 | 1.10 | 0.321 |
| Working status | |||||||||
| Currently workingRef | 1.00 | - | - | - | - | 1.00 | - | - | |
| Currently not working | 1.57 | 1.46 | 1.69 | 6.07 | 1 | 1.11 | 1.02 | 1.20 | 0.014 |
| Level of education | |||||||||
| No formal education | 0.81 | 0.72 | 0.92 | 0.39 | 1 | 0.94 | 0.78 | 1.13 | 0.531 |
| Primary | 0.66 | 0.58 | 0.73 | 2.41 | 1 | 0.91 | 0.80 | 1.03 | 0.120 |
| Secondary | 0.64 | 0.56 | 0.72 | 2.63 | 1 | 0.92 | 0.84 | 1.02 | 0.105 |
| TertiaryRef | 1.00 | - | - | - | - | 1.00 | - | - | |
| Marital Status | |||||||||
| Never marriedRef | 1.00 | - | - | - | - | 1.00 | - | - | |
| Currently married | 1.39 | 1.29 | 1.50 | 0.25 | 1 | 1.03 | 0.92 | 1.15 | 0.618 |
| Widow/Widower/Divorcee | 2.37 | 2.11 | 2.66 | 3.58 | 1 | 1.19 | 0.99 | 1.43 | 0.058 |
| HH income group | |||||||||
| Q1(lowest) | 0.75 | 0.67 | 0.83 | 0.18 | 1 | 1.03 | 0.90 | 1.19 | 0.671 |
| Q2 | 0.70 | 0.63 | 0.78 | 0.02 | 1 | 0.99 | 0.88 | 1.12 | 0.900 |
| Q3 | 0.74 | 0.67 | 0.82 | 0.28 | 1 | 1.03 | 0.92 | 1.15 | 0.594 |
| Q4 | 0.66 | 0.60 | 0.73 | 3.01 | 1 | 1.10 | 0.99 | 1.22 | 0.083 |
| Q5( highest)Ref | 1.00 | - | - | - | - | 1.00 | - | - | |
| Strata | |||||||||
| UrbanRef | 1.00 | - | - | - | - | 1.00 | - | - | |
| Rural | 1.11 | 1.04 | 1.18 | 3.52 | 1 | 1.08 | 1.00 | 1.16 | 0.060 |
| Ref,1.00: Reference group;#adjusted for all other variable | |||||||||
Table 2: Multivariate analysis of socio-demographic factors associated with anaemia in Malaysian adults: NHMS 2015.
Discussion
The global estimation on anaemia prevalence is important for monitoring the health status of the world population. The WHO estimates that a quarter of the world population is having anaemia based on 1993 to 2005 global data where the anaemia problem in Malaysia generally was considered to be of moderate level of public health significance [13]. The finding of national anaemia prevalence in this study was similar to the global estimation.
Most of the cases were considered as mild anaemia and only a small proportion of respondents were reported as having severe anaemia as found in many studies [14-16]. In the year 2011, the WHO repeated the project but focused on preschool age children (6-59 months) and women of reproductive age (15-49) as both groups are considered the at-risk population. The prevalence estimates among women of reproductive age (15-49) was 21% using data from 1995 to 2011 [17]. The prevalence estimate is much lower compared to the current findings which observed 34.67% women of reproductive age as having anaemia although the level of public health significance is still the same. Even though this study did not estimate the prevalence specifically for pregnant women, the Figure 1 shown for women of reproductive age is alarming as the prevalence of anaemia is much higher in pregnant women as estimated by the WHO in 2008 [13]. A previous local study conducted in clinical settings among pregnant women observed that the prevalence of anaemia in pregnancy was 35.0% using either capillary or venous sample with the HemoCue® Hemoglobinometer [15].
Various studies examine age and gender in further data analysis for anaemia [14,18]. Generally, the prevalence of anaemia in females is significantly higher compared to males as observed in the WHO study [13]. Females are more affected than males mainly due to physiological menstrual loss, increased demand during pregnancy, inadequate nutrient intake and parasitic infestations [19,20]. A previous study observed that the overall prevalence of anaemia in females is double the prevalence of anaemia in males [14]. The trend of anaemia prevalence is increasing from mild to severe levels of public health significance with the increasing age for males, while for females, the anaemia problem has started early in teenage age and continued further in child bearing age and elderly age. Both genders at the age of 75 years and above showed highest prevalence compared to the younger groups. This finding is similar to the findings in rural China; the prevalence was much higher in older age in both genders [21]. When comparing the prevalence between genders in adolescent groups, the prevalence of anaemia in female adolescents was three times higher than male adolescents in this study. A study conducted among adolescent groups in another country observed the prevalence of anaemia among female adolescents was double of male adolescents [22].
The pattern of anaemia according to specific age groups should alert program managers in targeting interventions for anaemia promptly. As mentioned earlier, older age groups are also susceptible to anaemia and the WHO global data estimated prevalence for anaemia in older persons aged 60 and above was 23.9% [13]. The prevalence of anemia in older persons aged 60 and above is much higher than the WHO global estimation in this study [13]. Other previous studies including systematic reviews revealed the prevalence of anaemia in those aged 65 years and above were within 7.0% to 40.0%, with a wide range being observed according to the location of the survey being conducted, as the prevalence was much lower in community settings compared to hospital settings [23-25]. Anaemia in elderly is most probably due to the anaemia of chronic diseases such as chronic kidney disease, nutritional deficiencies while one third still remained due to unexplained causes [7].
In Malaysia, ethnicity plays a strong determinant as it relates to certain cultural and religious beliefs especially towards food choice. For example, vegetarian food has lower iron nutrients compared to meat which may contribute to nutritional deficiency anaemia [26]. A study conducted among pregnant women observed ethnicity variation in hemoglobin concentration during antenatal check-up where Indian ethnicity had the significantly highest prevalence compared to other ethnicities as observed in this population-based study [16]. Indian ethnicity was associated with less intake of meat in their daily food consumption, concurring with a study that found those who partake of less meat were more likely to have anaemia [27]. A study conducted in rural China revealed an increase of anaemia prevalence within two years and one of the associated factors was a diet consisting of mainly vegetables [21].
Most of the previous studies are concentrating on determinants of anaemia among women of reproductive age, children or elderly and do not focus on determinants for the general population per se. Among the socio-demographic determinants for women of reproductive age, anaemia is associated with illiteracy and low economic status [28]. However, in this study, level of education, geographical distribution and household income were not associated with the prevalence of anaemia in the general population as observed in Eastern Sudan [29].
Anaemia continues to contribute to the global burden of disease as it affects all population groups if no intervention or action is taken promptly. The intervention plan has been included in the National Plan of Action for Nutrition of Malaysia (NPANM) III, 2016-2025 and the haemoglobin level is the indicator that is being monitored especially among women of reproductive age [30]. The target is to reduce the prevalence of anaemia in women of reproductive age by fifty percent in 2025. Anaemia also has a significant impact towards the quality of life among older persons where early identification among older persons will reduce the anaemia problem later and subsequently reduce complications from other co-morbidities.
This survey was the first population-based screening using point-ofcare for anaemia screening. A population-based survey in estimating anaemia prevalence is very costly and almost difficult to do successfully if using laboratory methods for haemoglobin measurement. Many studies have discussed the validity and reliability of HemoCue® Hemoglononometer on estimating hemoglobin concentration [31]. When using venous samples in both the HemoCue® Hb 201+ System and laboratory method, the hemoglobin readings are almost comparable [32]. Caution should be exercised while interpreting haemoglobin readings if capillary samples are used, as the reading might be higher compared to venous samples and may give a false negative result [31]. HemoCue® Hb 201+ System has been used as a recognized screening method in various surveys in multiple settings such as among blood donors and the worldwide survey in Demographic Health Surveys (DHS) for estimating hemoglobin level immediately after blood sampling [33].
The use of point of care testing should encourage more respondent participation as it utilizes minimal amounts of blood with minimally invasive procedure and portable analyzer with rapid results. However, a slightly lower response rate was detected from the teenage group and those of Chinese ethnicity. The response rate problem in any epidemiological study globally has been discussed in a previous study and many reasons for non-participation were observed [34]. In this survey, the younger population was observed to have higher numbers of refusal compared to the older group due to perceived selfsatisfaction on their own health. Ethnic Chinese respondents also revealed lower response rates compared to other ethnicities possibly due to either communication barrier with the data collector and higher self-satisfaction on their own health which contributed to unwillingness to join the national survey. Nevertheless, the overall response rate is considered acceptable and representative of the population.
Limitation
This study is based on HemoCue® Hb 201+ System using capillary sampling for the hemoglobin measurement which needs further confirmation from standard methods in the laboratory. However, HemoCue® Hb 201+ System has acceptable sensitivity and high specificity in detecting anaemia. This study also lacks data for those below 15 years as they were not included in this study. This study also is unable to identify the cause of anaemia, although the most common cause is due to iron deficiency anaemia. Identifying the anaemia cause is important in providing effective strategies to treat the condition in order to reduce the national prevalence of anaemia. Furthermore, this study only examined the association between socio-demographic variables and anaemia and does not include other factors associated with anaemia such as pattern of dietary intake, menstrual history for women and chronic diseases in elderly which were out of the scope of this study.
Conclusion
Anaemia is a significant public health problem that should be focused on especially among women of reproductive age and the elderly. Periodic screening using point-of care is essential and acceptable in population settings. The anaemia problem has been detected in respondents as young as 15 years and continues till elderly age in females. In males, the problem is mild in the young but sharply increases in the elderly. Anaemia in the general population is observed to be associated with female sex, elderly, Indian ethnicity, and those who are married, widower/widow and divorcee. Preventive measures such as iron supplementation, food fortification and encouraging food diversification should thus be started from the younger age group in the population.
Acknowledgements
The authors would like to thank all the respondents who volunteered to join this survey. The appreciation is further extended to all the staffs involved throughout the study.
Research Grant
This survey was funded by Ministry of Health Malaysia
References
- World Health Organization (2016) Health topics: Anaemia. Geneva.
- Ershler WB, Chen K, Reyes EB, Dubois R (2005) Economic burden of patients with anemia in selected diseases. Value Health 8: 629-638.
- World Health Organization (2016) Micronutrient deficiencies: Iron deficiency anaemia.
- World Health Organization (2011) Haemoglobin concentrations for the diagnosis of anaemia and assessment of severity. Vitamin and Mineral Nutrition Information System.
- Riva E, Tettamanti M, Mosconi P, Apolone G, Gandini F, et al. (2009) Association of mild anemia with hospitalization and mortality in the elderly: The Health and anemia population-based study. Haematologica 94: 22-28.
- Rani K, Gupta J, Gupta R, Aggarwal K (2014) Maternal anaemia and its severity: An independent risk factor for preterm delivery and adverse neonatal outcome. Int J ReprodContraceptObstetGynecol 3: 325-329.
- Patel KV (2008) Epidemiology of anemia in older adults. SeminHematol 45: 210-217.
- World Health Organization (2008) Worldwide prevalence of anaemia 1993-2005 of WHO global database of anaemia.
- The DHS Program (2016) Anaemia. Demographic and Health Surveys.
- Hassan R, Abdullah WZ, NikHussain NH (2005) Anemia and iron status of Malay women attending an antenatal clinic in KubangKerian, Kelantan, Malaysia. Southeast Asian J Trop Med Public Health 36: 1304-1307.
- NikNHR, MohdSN (2012) The rate and risk factors for anemia among pregnant mothers in Jerteh Terengganu, Malaysia. J Community Med Health Educ 2:150.
- Institute for Public Health (IPH) (2015) National health and morbidity survey 2015: Vol i: Methodology and general findings; 2015. Ministry of Health Malaysia, Malaysia.
- McLean E, Cogswell M, Egli I, Wojdyla D, de Benoist B (2008) Worldwide prevalence of anaemia, WHO vitamin and mineral nutrition information system, 1993–2005. Public Health Nutr 12: 444.
- Eftekharzadeh-Mashhadi I, Hedayati-Moghaddam MR, Fathimoghadam F, Bidkhori HR, Shamsian SK (2015) Anemia as a public health issue in Mashhad, Iran: Evidence from the first population-based study. Acta Med Iran 53: 186-190.
- Haniff J, Das A, Onn LT, Sun CW, Nordin NM, et al. (2006) Anemia in pregnancy in Malaysia: A cross-sectional survey. Asia Pac J ClinNutr 16: 527-536.
- Tan ACC, Leong EWK, Chua AC, Moy FM (2013) Racial variations in booking haemoglobin of primigravidae in Malaysia: A prospective study. BMC Res Notes 6: 173.
- WHO (2015) The global prevalence of anaemia in 2011. World Health Organization, Geneva.
- Kolarović J, Ćulafić J, Čabarkapa V, Vučković N, Vučković D, et al. (2014) The incidence of anemia in the adult working population of Vojvodina. J Med Biochem 33.
- Pala K, Dundar N (2008) Prevalence and risk factors of anaemia among women of reproductive age in Bursa, Turkey. Indian J Med Res 128: 282.
- Piammongkol S, Chongsuvivatwong V, Williams G, Pornpatkul M (2006) The prevalence and determinants of iron deficiency anemia in rural Thai-Muslim pregnant women in Pattani province.
- Wang X, Wu Z, Chen Y, Zhu J, Dong X, et al. (2015) Increased prevalence and incidence of anemia among adults in transforming rural China: Two cross-sectional surveys. BMC Public Health 15: 1302.
- Alquaiz AJM, Khoja TA, Alsharif A, Kazi A, Mohamed AG, et al. (2015) Prevalence and correlates of anaemia in adolescents in Riyadh city, Kingdom of Saudi Arabia. Public Health Nutr 18: 3192-3200.
- Juárez-Cedillo T, Basurto-Acevedo L, Vega-García S, Manuel-Apolinar L, Cruz-Tesoro E, et al. (2014) Prevalence of anemia and its impact on the state of frailty in elderly people living in the community: SADEM study. Ann Hematol 93: 2057-2062.
- Gaskell H, Derry S, Moore AR, McQuay HJ (2016) Prevalence of anaemia in older persons: Systematic review. BMC Geriatr 8: 1.
- Yildirim T, Yalcin A, Atmis V, Cengiz OK, Aras S, et al. (2015) The prevalence of anemia, iron, vitamin B12, and folic acid deficiencies in community dwelling elderly in Ankara, Turkey. Arch GerontolGeriatr 60: 344-348.
- Chandyo RK, Strand TA, Ulvik RJ, Adhikari RK, Ulak M, et al. (2007) Prevalence of iron deficiency and anemia among healthy women of reproductive age in Bhaktapur, Nepal. Eur J ClinNutr 61: 262-269.
- Haidar JA, Pobocik RS (2009) Iron deficiency anemia is not a rare problem among women of reproductive ages in Ethiopia: A community based cross sectional study. BMC Blood Disord 9: 7.
- Asres Y, Yemane T, Gedefaw L (2014) Determinant factors of anemia among nonpregnant women of childbearing age in Southwest Ethiopia: A community based study. IntSch Res Not 2014: 1-8.
- Abdallah TM, Adam I, Abdelhadi MA, Siddig MF, Ali AA (2012) Anaemia among adults in Kassala, Eastern Sudan. BMC Res Notes 5: 202.
- MOH (2016) National plan of action for nutrition of Malaysia (NPANM) III, 2016-2025. Ministry of Health Malaysia.
- Sanchis-Gomar F, Cortell-Ballester J, Pareja-Galeano H, Banfi G, Lippi G (2013) Hemoglobin point-of-care testing the hemocue system. J Lab Autom 18: 198-205.
- Nkrumah B, Nguah S, Sarpong N, Dekker D, Idriss A, et al. (2011) Hemoglobin estimation by the HemoCue® portable hemoglobin photometer in a resource poor setting. BMC ClinPathol 11: 5.
- Briggs C, Carter J, Lee SH, Sandhaus L, Simon-Lopez R, et al. (2008) ICSH Guideline for worldwide point-of-care testing in haematology with special reference to the complete blood count. Int J Lab Hematol 30: 105-116.
- Galea S, Tracy M (2007) Participation rates in epidemiologic studies. Ann Epidemiol 17: 643-653.
Relevant Topics
- Addiction
- Adolescence
- Children Care
- Communicable Diseases
- Community Occupational Medicine
- Disorders and Treatments
- Education
- Infections
- Mental Health Education
- Mortality Rate
- Nutrition Education
- Occupational Therapy Education
- Population Health
- Prevalence
- Sexual Violence
- Social & Preventive Medicine
- Women's Healthcare
Recommended Journals
Article Tools
Article Usage
- Total views: 7243
- [From(publication date):
April-2017 - Nov 23, 2024] - Breakdown by view type
- HTML page views : 6390
- PDF downloads : 853