Research Article Open Access
A Pilot Study on Undergraduate Palliative Care Education A Study on Changes in Knowledge, Attitudes and Self-Perception
Karger A1, Scherg A2*, Schmitz A2, Wenzel-Meyburg U2, Raski B1, Vogt H2, Schatte G2, Schatz M2, Schnell MW3and Schulz C1,21University Dusseldorf, Medical Faculty, Institute for Psychosomatic Medicine, Dusseldorf, Germany
2University Dusseldorf, Medical Faculty, Interdisciplinary Centre for Palliative Medicine, Dusseldorf, Germany
3Institute for Ethics and Medical Communication (IEKG), Witten/Herdecke University, Germany
- *Corresponding Author:
- Alexandra Scherg, PhD
University Hospital Dusseldorf
Interdisciplinary Centre for Palliative Medicine
Moorenstraße 5, Dusseldorf
40225, Germany
Tel: +49 211 8108696
E-mail: alexandra.scherg@med.uni-duesseldorf.de
Received date: January 11, 2015 Accepted date: November 04, 2015 Published date: November 07, 2015
Citation:Karger A, Scherg A, Schmitz A, Wenzel-Meyburg U, Raski B, et al. (2015) A Pilot Study on Undergraduate Palliative Care Education–A Study on Changes in Knowledge, Attitudes and Self-Perception. J Palliat Care Med 5: 236. doi:10.4172/2165-7386.1000236
Copyright: © 2015 Karger A, et al. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.
Visit for more related articles at Journal of Palliative Care & Medicine
Abstract
Background: Since 2013 medical faculties in Germany have to teach and assess palliative care issues. Objective: Evaluation of a one-week intensive seminar in palliative care with regard to cognitive and affective learning objectives. Methods: Exploratory prospective naturalistic study with pre (T1) and post (T2) measurement, investigating medical students' (N=31) knowledge, opinions and attitudes as well as estimation in self-efficacy regarding palliative care issues. The sample contains of undergraduate medical students before and after an interdisciplinary palliative care course (40 teaching units) held at the Medical Faculty of Heinrich Heine University Dusseldorf, Germany. Results: Upon completion of the seminar, students demonstrated a significant increase of palliative care-related knowledge and a positive self-estimation in competence and self-efficacy with regard to treating and caring for dying patients. However, no changes were found on the subject of a greater acceptance and reduced fear of death and dying. Conclusions: The acquisition of affective learning objectives with regard to essential attitudes towards death and dying may require a longer learning process and thus a longitudinal implementation into medical school curricula.
Keywords
Palliative care; Undergraduate medical education; Attitude; Competence; Knowledge
Abbreviations
TU: Teaching Unit (45 minutes)
Background
Palliative care is becoming more and more important in medical education and the number of European countries with palliative care training for medical students is rising [1,2]. Since 2013 medical faculties in Germany face the challenge and formal obligation to teach and assess palliative care learning objectives within the medical curriculum. By being integrated into the Medical Licensure Act for Physicians in 2009, undergraduate palliative care education (UPCE) was mandatorily incorporated in medical education in Germany [3].
There is a national as well as an international expert consensus on palliative care curricula, developing basic recommendations for enhancing the quality of structures and processes in medical underand postgraduate education (cf. EAPC 2007, DGP 2009). With regard to medical education, for instance, a minimum amount of forty teaching units (TU=forty-five minutes) as well as structured and weighted teaching contents are strongly recommended.
Various studies have highlighted the limited knowledge base in palliative care of final-year medical students in Germany [4-6]. A current survey conducted in 2012 to investigate the progress of implementation of palliative care curricula in medical faculties in Germany [6,7] demonstrated that UPCE was mainly taught interprofessionally and in an advanced semester and comprised twelve to forty-three TU.
However, less than half of the faculties (47%) include bedside teaching and only 59% include real patient contacts into their curricula. Predominant teaching formats are lectures (93%) and seminars (75%). Formal assessment of knowledge and skills is mostly effectuated by means of multiple choice tests (84%), all of which might indicate a lack of human resources in teaching and assessing palliative care, resulting in the above-mentioned observed dominance of cognitive learning objectives with rare patient contact in UPCE in Germany.
Currently, the main focus in medical education in Germany is on gaining factual knowledge rather than psychomotor skills or communication. Teaching and assessing affective and psychomotor learning objectives [8] in the context of students’ perception of personal competencies and patient-oriented professional practice come second [9].
The predominance of cognitive learning objectives is acknowledged as a general problem in undergraduate medical education. Two systematic reviews [10,11] investigating palliative care education in medical faculties in Europe and America conclude that, apart from summative and formative assessments, affective learning objectives with regard to attitude toward dying patients should be awarded significantly greater importance in the future.
Various authors particularly emphasize the significance of a positive attitude towards dying and death as well as towards caring for terminally ill and dying patients [5,10,12] and the use of reflection [13] for the development of an adequate perception of the physician’s professional role. In medical practice, unconscious ambivalent or negative emotions (e.g. fear of dying and death) are associated with various avoidance strategies and, ultimately, with a lower quality of medical practice [3,14-18]. Presumably, the reverse is also true, that a positive change of attitude improves the quality of care [19].
How to teach affective learning objectives, skills and attitudes is an issue which has been rarely investigated empirically with regard to undergraduate and post-graduate palliative care education [20]. The purpose of the present exploratory prospective naturalistic study was to evaluate a one-week palliative care course with regard to the acquisition of affective learning objectives. In addition, the questionnaires and instruments to assess attitudes towards death and dying and emotional experiences are shortly introduced.
Methods
Study sample
The study sample consisted of two cohorts of undergraduate students from Heinrich Heine University Düsseldorf (Schulz 2015). In the first study cohort, fifteen medical undergraduate students completed the compulsory elective subject Palliative Care during the summer semester of 2012, whereas the second study cohort was comprised of the sixteen students completing the course during the winter semester of 2012/2013, resulting in a total of thirty-one participants of both cohorts (nine male, twenty-two female). At the beginning of the study, participants were aged between twenty to thirty-five years (mean=25.50, SD=3.22) and in their fourth to sixteenth semester (mean=8.84, SD=2.38). Two participants reported pre-education in palliative care. The majority of students had already experienced an encounter with a dying patient in the course of their medical education (n=19) or personal bereavement of a loved one (n=25).
Data were collected via written self-assessment. Ethical approval was obtained from the ethics committee of the Medical Faculty of Heinrich Heine University Dusseldorf, Germany. The study was conducted in accordance with the Declaration of Helsinki on Ethical Principles for Medical Research involving Human Subjects. Before the start of the study, the participants were informed about the purpose and procedure of the study and provided their written informed consent prior to participation.
The course
Since 2008, an interdisciplinary working group of the Medical Faculty of Heinrich Heine University Dusseldorf, Germany, had been developing a palliative care curriculum in a systematic process according to Kern’s approach [21] to curricular development and in accordance with the recommendations of the EAPC (2007) and the DGP (2009) which is being implemented in a three-step process.
The longitudinal curriculum consists of five contextual teaching domains: symptom management, communication and interaction, inter-professionalism, ethical/legal/societal aspects, and self-reflection, all of which had been assigned specifically defined cognitive psychomotor learning objectives. The structure of the curriculum is described elsewhere [22]. The UPCE course evaluated in the present study is a one-week intensive seminar consisting of ten modules and comprising 40 TU.
It is part of the mandatory elective courses and is held on an interdisciplinary and interprofessional basis for fourth- and fifth-year medical students and comprises topics from palliative medicine, oncology, psychooncology, spiritual care, social services and self-help [22]. The used didactic methods and approaches are learner-centred small-group-teaching, virtual standardized patient contact (VSPC), bedside teaching, standardized role play with simulated/standardized patients as well as 5 TU guided group sessions for self-reflection (Table 1).
| Mandatory elective Course >>Palliative care-intensive course<<Timetable | |||||
|---|---|---|---|---|---|
| Time | Monday | Tuesday | Wednesday | Thursday | Friday |
| 08 30 | Evaluation | ||||
| 09 00 | Film >>I See You<< Module 1 Psychiatric symptoms in palliative care | Module 3 Gastrointestinal symptoms: Nausea, vomiting, obstipation, diarrhoea Indications for PEG-tube (in patients with chronic dysphagia/weight loss) | Module 5 Symptom management pain, acute pain | Module 7 Basal stimulation maintaining patient’s quality of life and well-being/comfort | Module 9 Symptom management during final phase |
| Lecture/Profession | Physician/Psychotherapist | Physician | Physician | Nurse | Physician |
| Didactic method/approach | Virtual Standardized Patient(VSP) | Problem Based Learning/PBL including Case studies | Small groups Real patient contact | Small groups experimental/Self awareness | Interactive exercise/Problem based learning/PBL |
| 12 00 | Lunch break | ||||
| 13 00-16 00 | MODULE 2 CoMed Breaking Bad news in Palliative care | MODULE 4 Ethical issues at the end of life Advance care planning | MODULE 6 Working within the interprofessional team | MODULE 8 Finding sense & existential issues/phenomena | MODULE 10 CoMed Communication with mourning relatives |
| Lecturer/profession | Physician Psychologist | Physician | Social worker | Clergy | Physician Psychologist |
| Didactic method/approach | Standardized patient contact(SPC) | Interactive lecture Role play | Small groups Group discussions | Interactive exercise Role play Model based learning | Standardized patient contact(SPC) |
| 16 15- 16 45 | Self-development within the group | Self-development within the group | Self-development within the group | Self-development within the group | Self-development within the group |
Table 1: Timetable UPCE-course Heinrich Heine University Dusseldorf September 2012/March 2013.
Questionnaires
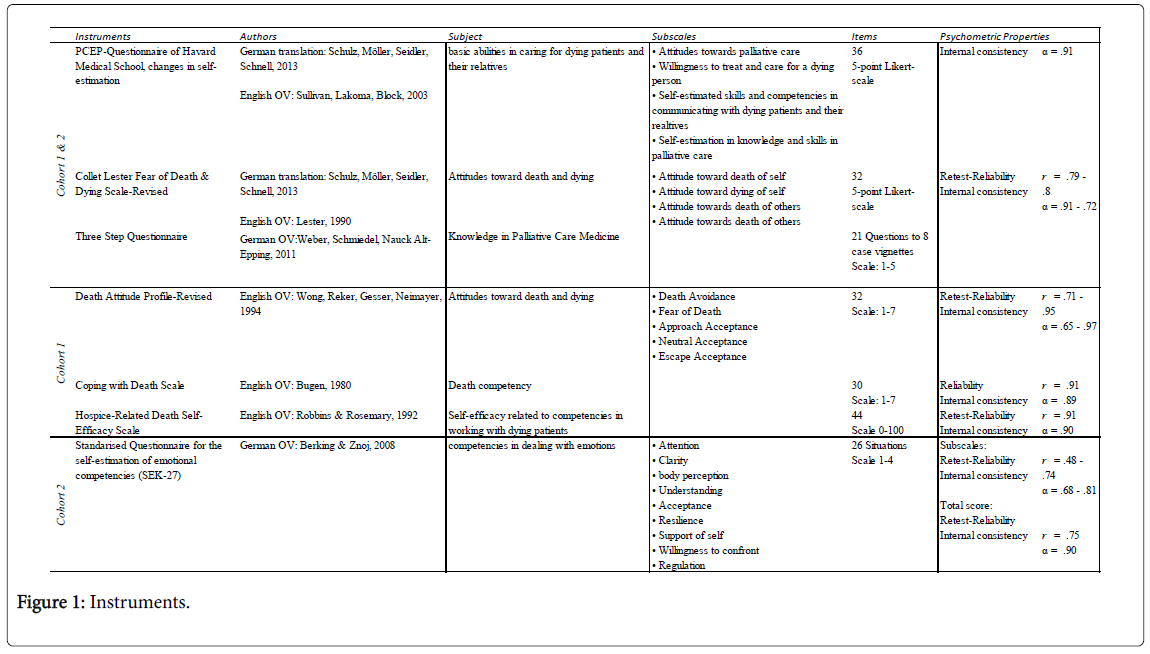
We applied four questionnaires to all students. The questionnaire of the Program in Palliative Care Education and Practice (PCEP) of Harvard Medical School, Boston, USA [23,24] was used to obtain information about attitudes towards palliative care, willingness to treat and care for a dying person, self-estimated skills and competencies in communicating with dying patients and their relatives as well as selfestimation in knowledge and skills in palliative care. The Collet Lester Fear of Death and Dying Scale-Revised [23-25] was used to obtain information about attitudes towards and fears of death and dying of self and others. Data about participants’ palliative care knowledge was collected by means of the Three Step Questionnaire [6,7], an instrument consisting of 21 questions related to eight case examples.
In addition, the following questionnaires were applied to the first cohort of 15 students: the Death Attitude Profile-Revised [26] to enquire about opinions and attitudes towards death, the Coping with Death Scale [27] to identify participants’ self-estimation in skills and competencies in dealing with death and dying, and the Hospice- Related Death Self-Efficacy Scale [28] to investigate estimation in selfefficacy in communicating with and caring for the dying. In the second cohort of 16 students, the Standardized Questionnaire for Self- Estimation in Emotional Competency and Skills (SEK-27, [29] was used. We didn’t apply all seven questionnaires to all students to keep the answering time on a manageable level. No bias was introduced by the different treatment of the two cohorts because no inter-cohort comparisons were made. For details of all questionnaires used, (Figure 1).
As no validated German translation existed for the questionnaires death attitude profile-revised, coping with death scale and hospice related death self-efficacy scale, the english original versions were used for the purpose of this study
Data collection
The participating students completed the paper-based questionnaires immediately before the start (T1) as well as immediately after completion (T2) of the one-week intensive seminar as described above. In addition, semi-structured interviews were conducted with the first-cohort-participants and analysed qualitatively, the results of which will be published after completion of the qualitative analysis.
Hypotheses and statistical analyses
It was hypothesized that, upon completion of the course, the students would show an increased self-estimation in skills and competencies with regard to dealing and communicating with dying patients and would have acquired increased knowledge with regard to palliative care. It was furthermore expected as a result of the increased self-esteem and knowledge that the participating students would develop a more positive and accepting attitude, i.e. a decrease of fear of patients dying and death with no changes with regard to fear of death and dying of self.
The study used a pre (T1) and post (T2) measurement, with the collected data being analysed by means of a dependent t-test for paired samples. Missing data of T1 were substituted by the study subject’s mean value of the respective subscale, whereas missing data of T2 were substituted by the respective data of T1, in which case no change in attitude was assumed. We treated the missing data of T1 and T2 differently because the statistically more accurate method is to fill up missing data with respective former data, which in this case is only possible at T2. Whereas the less accurate but only possible method to fill up missing data at T1 is using the means of the respective subscale. The level of statistical significance was α=0.05.
Results
The comparison of pre and post data of the Harvard-PCEP questionnaire yielded significant changes in the three subscales (level of preparation for dealing and communicating with dying patients, self-estimation in palliative care skills and self-estimation in communication competency), with higher values at T2. No changes were observed regarding attitudes towards palliative care (Table 2). However, upon completion of the intensive seminar, almost a third of the students still estimated their level of preparation as well as their communication competencies, knowledge and skills as insecure or neutral.
| Scale | T1 M ± SD | T2 M ± SD | t | df | p-value | MD | 95 % CI |
|---|---|---|---|---|---|---|---|
| Attitude | 39.80 ± 3.33 | 41.23 ± 3.11 | -1.73 | 60 | 0.09 | -1.42 | -3.06 -0.22 |
| Preparation | 28.49 ± 6.79 | 43.16 ± 5.76 | -21.49 | 47.17 | .00* | -14.67 | -17.87 -11.47 |
| Communication | 26.39 ± 3.34 | 17.97 ± 5.26 | 7.49 | 51.09 | .00* | 8.42 | 6.17 10.67 |
| Knowledge/Skills | 10.0 ± 2.72 | 14.32 ± 2.23 | -6.85 | 60 | .00* | -4.32 | -5.59 -3.06 |
Table 2: Results of pre (T1) and post (T2) measurements, PCEB questionnaire of Harvard Medical School.
Data obtained from the Collet-Lester Fear of Death and Dying Scale-Revised with regard to the investigated subscales fear of death of self, fear of dying of self, fear of death of others and fear of dying of others yielded no significant changes in attitudes measured at T1 and T2 (Table 3).
| Scale | T1 M ± SD | T2 M ± SD | t | df | p-value | MD | 95 % CI |
|---|---|---|---|---|---|---|---|
| Fear of death - self | 23.96 ± 6.16 | 24.35 ± 7.01 | -0.23 | 60 | 0.81 | -0.39 | 3.74 2.97 |
| Fear of dying - self | 17.52 ± 4.79 | 17.96 ± 5.26 | -0.35 | 60 | 0.73 | -0.45 | -3.01 2.11 |
| Fear of death - others | 18.86 ± 5.32 | 19.87 ± 5.56 | -0.73 | 60 | 0.46 | -1.01 | -3.38 1.75 |
| Fear of dying - others | 21.84 ± 4.94 | 24.03 ± 5.72 | -1.61 | 60 | 0.11 | -2.19 | -4.90 0.53 |
Table 3: Results of pre (T1) and post (T2) measurements, Collet-Lester-FoDD-Scale-Revised.
With regard to the students’ palliative care knowledge which had been assessed by the Three Step Questionnaire, the mean value of the proportionally correct answers at T1 of 0.28 (SD=0.11) was shown to have significantly increased by T2 to 0.45 (SD=0.16) (t (30)=-7.58; p=<0.001). Furthermore, the mean value of incorrect answers tended to decrease from 0.39 (SD=0.03) to 0.32 (SD=0.16) (t (30)=1.99; p=0.055). The possibility not to choose any of the given answers was used more frequently at T1, which is why the mean proportional share was 0.33 (SD=0.17) and significantly decreased at T2 to M=0.23 (SD=0.16) (t (30)=3.67; p=0.001). Due to the interdependency of the amount of correct and incorrect answers – the more correct answers are given, the less incorrect answers can be given – the ratio of correct and incorrect answers was compared as well, also demonstrating a decided change of the mean value from T1 to 0.89 (SD=0.68) at T2 (t(30)=-3.22; p=0.003). Therefore analyses demonstrate an increase of palliative care-related knowledge and skills upon completion of the mandatory elective course Palliative Care.
With respect to the questionnaires which had been additionally applied to the first cohort (N=15), a comparison of T1 and T2 in the subscales of the Death Attitude Profile-Revised yielded no significant changes regarding attitudes to death (Table 4). On the other hand, a comparison of pre and post data from the Coping with Death Scale and the Hospice-Related Death Self-Efficacy Scale showed significant changes. For instance, the mean value of the Coping with Death Scale significantly increased from 127.8 (SD=18.86) at T1 to 139.33 (SD=17.24) at T2. Likewise, the analysis of data from the Hospice- Related Death Self-Efficacy Scale showed a significant difference of the mean score (t (14)=-4.23; p=0.001), with a mean value of 63.02 (SD=10.68) at T1, compared to the mean value of 70.24 (SD=9.70) at T2. Analyses therefore demonstrate that upon completion of the mandatory elective course, the participating students consider themselves as more competent in dealing with death and dying.
| Scale | T1 M ± SD | T2 M ± SD | t | df | p-value | MD | 95 % CI |
|---|---|---|---|---|---|---|---|
| Attention | 7.81 ± 2.37 | 9.31 ± 2.06 | -1.99 | 15 | 0.065 | -1.5 | -3.10 0.10 |
| Lucidity | 7.41 ± 2.25 | 9.06 ± 1.98 | -2.76 | 15 | 0.015 | -1.66 | -2.93 0.38 |
| Body awareness | 7.19 ± 2.17 | 8.38 ± 2.5 | -2.08 | 15 | 0.055 | -1.19 | -2.41 0.03 |
| Understanding | 7.75 ± 2.98 | 8.81 ± 1.87 | -1.18 | 15 | 0.257 | -1.06 | -2.98 0.86 |
| Acceptance | 7.75 ± 1.63 | 8.31 ± 1.99 | -1.31 | 15 | 0.21 | -0.81 | -2.14 0.51 |
| Resilience | 6.69 ± 2.52 | 8.25 ± 1.69 | -2.40 | 15 | 0.03 | -1.56 | -2.95 -0.17 |
| Self-support | 7.19 ± 3.33 | 8.06 ± 2.64 | -1.24 | 15 | 0.234 | -0.88 | -2.38 0.63 |
| Regulation | 5.88 ± 2.28 | 7.75 ± 2.49 | -2.46 | 15 | 0.027 | -1.88 | -3.50 -0.25 |
| Willingness to deal with conflicts | 7.56 ± 2.50 | 8.75 ± 1.88 | -2.41 | 15 | 0.029 | -1.19 | -2.24 -0.14 |
| Gesamt | 64.97 ± 14.62 | 76.69 ± 13.46 | -2.52 | 15 | 0.023 | -11.72 | -21.62 -1.81 |
Table 4: Results of pre (T1) and post (T2) measurements, self-estimation in emotional competencies and skills (SEK-27).
Likewise, the analyses of the pre and post data of the various subscales of the questionnaire Standardized Questionnaire for Self- Estimation in Emotional Competency and Skills (SEK-27), which had been applied exclusively to the second cohort (N=16), demonstrated a significant increase of the total mean value as well as of the mean value of the subscales lucidity, resilience, regulation and willingness to deal with conflicts (Table 4). The results of these analyses may be interpreted as students’ self-perceived increased emotional competence upon completion of the course.
Discussion
The present pilot study evaluated changes in palliative care-relevant knowledge as well as in opinions and attitudes towards palliative care and end-of-life issues upon completion of a one-week intensive seminar in palliative care. In summary, it can be stated that the participating students estimated their palliative care-related knowledge and skills as well as their skills in communicating with dying patients and their relatives as significantly improved after completing the course. This improvement of skills corresponds to an objective knowledge gain, as can be seen from the results of the Three Step Questionnaire [7], which measures objective knowledge gain. Nevertheless, almost a third of the participating students remained neutral to insecure with respect to their self-estimated knowledge and skills upon completion of the seminar. No changes were observed regarding participants’ attitudes to death and dying, which was also supported by the analyses of data obtained from the additional questionnaires applied to either one or the other student cohort. While self-estimation in competencies in dealing with and caring for dying patients improved significantly, no changes were observed in participants’ opinions and attitudes towards death and dying. Therefore and contrary to what had been assumed, a critical affective learning objective was not accomplished.
The results of the present study are in accordance with the literature, the fact of which might suggest that changing opinions and attitudes or the acquisition of affective learning objectives may be considerably more difficult or complex than assumed [30]. For example, fourth year students’ attitudes were investigated after a two-week palliative care course and compared with an intensive four-week course [31]. Selfefficacy was assessed using the Self-efficacy in Palliative Care Scale, and attitudes towards palliative care and caring for dying patients were measured by means of the Thanatophobia Scale.
At the end of both curricula, students’ self-efficacy and attitude towards caring for dying patients improved significantly, with a more pronounced increase of self-efficacy after the intensive course than after the two-week course and no difference regarding students’ attitude towards caring for dying patients. A mandatory one-week palliative care course in undergraduate medical education with fifthyear students (N=84) was evaluated [32] which included regular direct patient encounters on a palliative care ward. The study used a naturalistic design to assess palliative care-relevant knowledge and skills at the beginning and at the end of the course as well as an evaluation of teaching contents and methods/approaches. Results demonstrated a positive view of the course and a significant improvement of palliative care-relevant knowledge and skills.
A prospective controlled quasi-experimental study [24] was conducted to evaluate an undergraduate palliative care curriculum based upon EAPC recommendations, which was offered to fourth-year medical students. For evaluation purposes, the German version of the Program in Palliative Care Education and Practice of Harvard Medical School in Boston, USA, as well as the Collet-Lester-Fear-of-Death- Scale-Revised were used. The course consisted of thirty one TU taking place in the course of two consecutive semesters.
The used didactic methods and approaches were learner-centred small-group-teaching, problem-based learning, bedside teaching as well as role-play. The study demonstrated significant effects in students of the intervention group, with a better feeling of preparedness for dealing with and caring for dying patients, an improved self-estimation in palliative care-related knowledge and skills as well as communication skills with regard to dying patients and their relatives. Empowering medical students on a knowledge and psychomotor skills level to gain competence in palliative care seems to be more achievable than changing their emotional responses to death and dying and their attitudes. It has also to be stated that change of attitudes and affective psychomotor skills get less attention in educational research on palliative care.
There are some lessons, which can be learnt from educational research. Longer and longitudinally integrated palliative care teaching [22] might support attitudinal change in a better way. However, this is not the only possible conclusion. It is well known from the literature that death confrontation has a relevant impact on the professional role modelling for medical students [17,19,33]. Having an opportunity to talk about their experiences and having a validating and supportive peer and professional environment after a significant death confrontation seem to be the central aspects for developing resilience in clinical death encounters. Hence, developing effective teaching interventions that focus on the emotional impact of palliative care in medical students should be considered a research priority.
The limitations of this study arise from its nature as naturalistic study (without a control group). The small number of participants also leads to limitations of the results. As a pilot study, the work presented here identifies open questions in the field of didactic research in palliative care education. The data at T2 was collected immediately after the course. This timing causes limitations to the section of knowledge-gain. However, the timing doesn’t affect the change of attitudes and change of self-reflection.
The theoretically assumed and heuristically reasonable relation of attitudes and skills is still unclear. It is a strong theoretical argument, that higher grade of acceptance of death and dying does in fact correspond to a higher quality in treatment and care of dying patients and their relatives but up to date there is no empirical study on this subject. Furthermore, the psychological concepts regarding the general significance of attitudes for people’s actions/practice also are still inconsistent. The relevance of subjective estimation in self-efficacy is still not known. According to the concept of self-efficacy [34], a positive estimation in self-efficacy corresponds to improved knowledge and expertise. Nevertheless, it has not been established whether a positive self-estimation with regard to dealing with and caring for dying patients does in fact result in a higher quality in terminally ill patient’s healthcare, a fact which also indicates a general predicament of didactic research in palliative care education [35].
It is well established that didactic interventions improve the competence of the students or physicians. But the present study indicates that an evaluation of palliative care education should include more than knowledge and self-efficacy. There is need for scientific studies evaluating objectively observable behaviours and practices of undergraduate medical students and physicians with respect to the treatment of and communication with dying patients. The change of attitudes, especially dealing with emotions regarding death and dying deserves more attention and its theoretically hypothesized relevance need empirical confirmation.
Acknowledgement
We thank the students for participating on the study. We thank Daniel Schlieper for critical reading of the manuscript.
References
- Centeno C, Lynch T, Donea O, Rocafort J, Clark D (2013) EAPC Atlas of Palliative Care in Europe 2013 - Full Edition. Milan: EAPC.
- DeCoste-Lopez J, Madhok J, Harman S (2015) Curricular Innovations for Medical Students in Palliative and End-of-Life Care: A Systematic Review and Assessment of Study Quality. Journal of palliative medicine 18(4):338-349.
- Hoppe JD, Wiesing U (2010) Empfehlungen der Bundesärztekammer und der zentralenEthikkommissionbei der BundesärztekammerzumUmgangmitVorsorgevollmacht und Patientenverfügung in der ärztlichen Praxis. DtschArztebl18:B769-774.
- Lang K, Puhlmann K, Falckenberg M (2006) Aus-, Fort- und Weiterbildung in der Palliativversorgung. Bundesgesundheitsblatt-Gesundheitsforschung-Gesundheitsschutz49:1149-1154.
- Olthuis G, Dekkers W (2003) Medical education, palliative care and moral attitude: some objectives and future perspectives. Medical education 37:928-933.
- Weber M, Schmiedel S, Nauck F, Alt-Epping B (2011) Knowledge and attitude of final-year medical students in Germany towards palliative care-an interinstitutional questionnaire-based study. BMC palliative care 10:19.
- Weber M, Schmiedel S, Nauk F, Alt-Epping B (2015) Wissen und Selbsteinschätzung in Bezug auf palliativmedizinischeFragestellungenbeiMedizinstudierenden: Macht das praktischeJahreinenUnterschied?Der Schmerz1-7.
- Anderson LW, Krathwohl DR, Airasian PW, Cruikshank KA, Mayer RE, et al. (2001) Taxonomy for learning, teaching, and assessing: A revision of Bloom's taxonomy of educational objectives, abridged edition. White Plains (NY): Longman.
- Rodin G (2013) Research on psychological and social factors in palliative care: An invited commentary. Palliat Med 27:925-931.
- Lloyd-Williams M, Macleod RDM (2004) A systematic review of teaching and learning in palliative care within the medical undergraduate curriculum. Med Teach 26:683-690
- Bickel-Swenson D (2007) End-of-life training in US medical schools: a systematic literature review. Journal of palliative medicine 10:229-235.
- Gibbins J, McCoubrie R, Forbes K (2011) Why are newly qualified doctors unprepared to care for patients at the end of life? Medical Education 45:389-399.
- Rosenbaum ME, LobasJ & Ferguson K (2005) Using reflection activities to enhance teaching about end-of-life care. Journal of Palliative Medicine 8:1186-1195.
- Kasket E (2006) Death and the Doctor. Existential Analysis: Journal of the Society for Existential Analysis 17: 1.
- Wentland K, Krzyzanowska MK, Swami N, Rodin GM, Le LW, et al. (2012) Referral Practices of Oncologists to Specialized Palliative Care. Journal of Clinical Oncology 30:4380-4386.
- Ciakowska-Rysz A, Diercanowski T (2013) Personal fear of death and dying affects the proper process of breaking bad news. Arch Med Sci9:127-131.
- Kumar SP, D’Souza M, Sisodia V (2013) Health care professionals fear of death an dying: Implications for palliative care. Indian J Palliat Care 19:196-198.
- Romotzky V, Galushko M (2015) It’s not that easy“ – Medical students fears and barriers in end-of life communication. Journal of cancer education 30:333-339.
- Corn BW (2009) Ending end-of-life phobia—a prescription for enlightened health care reform. New England Journal of Medicine 361:e63.
- Kaye (1991) Will a course on death and dying lower students death and dying anxiety. Journal of cancer education 6:21-24.
- Kern DE, Thomas PA, Hughes MT (2010) Curriculum development for medical education: a six-step approach.
- Schulz C, Wenzel-Meyburg U, Karger A, Scherg A, In der Schmitten J, et al (2015) Implementation of palliative care as a mandatory cross-disciplinary subject (QB13) at the Medical Faculty of the Heinrich-Heine-University Düsseldorf, Germany. GMS Z Med Ausbild 32: Doc6.
- Sullivan AM, Lakoma MD, Block SD (2003) The Status of Medical Education in End-of-life Care. J Gen Intern Med 18:685-695.
- Schulz C, Möller MF, Seidler D, Schnell MW (2013) Evaluating an evidence-based curriculum in undergraduate palliative care education: piloting a phase II exploratory trial for a complex intervention. BMC medical education 13:1.
- Lester D (2015) The collett-lester fear of death scale: The original version and a revision. Death Studies 14:451-68.
- Wong P, Reker G, Gesser G (1994) Death Attitude Profile-Revised: A multdimensionalmeassure of attitudes toward death. In: Neimeyer RA, editor. Death Anxiety Handbook: Research, Instruments, and Application121-48.
- Bugen L, Berlinger L, Hawkins R (1980) The measurement of coping processes: Attributes, skills, and quality of life indicators.
- Robbins RA (1992) Death competency: A study of hospice volunteers. Death Studies 16:557-569.
- Berking M, Znoj H (2008) Entwicklung und ValidierungeinesFragebogenszurstandardisiertenSelbsteinschätzungemotionalerKompetenzen (SEK-27). ZeitschriftfürPsychiatrie, Psychologie und Psychotherapie 56:141-153.
- Mann K, Gordon J, MacLeod A (2009) Reflection and reflective practice in health professions education: a systematic review. Adv in Health SciEduc 14:595-621.
- Horowitz R, Gramling R, Quill T (2014) Palliative care education in US medical schools. Medical Education48:59-66.
- Tai V, Cameron-Taylor E, Clark K (2013) A Mixed Methodology Retrospective Analysis of the Learning Experience of Final Year Medical Students Attached to a 1-Week Intensive Palliative Care Course Based at an Australian University. American Journal of Hospice and Palliative Medicine.
- Rhodes-Kropf J, Carmody S, Seltzer D, Redinbaugh E, Gadmer N, et al. (2005) This ist just to awful; I just can’t believe I expierenced that….“: Medical Student‘ Reactions to Their „Most Memorable“ Patient death. Academic Medicine 80:634-640.
- Bandura A (1977) Self-efficacy: toward a unifying theory of behavioral change. Psychological review84:191.
- Schulz C, MöllerM, Schmincke-Blau I, Schnell M (2009) Communication with the dying patient–Results of a controlled intervention study on communication skills in undergraduates. European Journal of Palliative Care 11.
Relevant Topics
- Caregiver Support Programs
- End of Life Care
- End-of-Life Communication
- Ethics in Palliative
- Euthanasia
- Family Caregiver
- Geriatric Care
- Holistic Care
- Home Care
- Hospice Care
- Hospice Palliative Care
- Old Age Care
- Palliative Care
- Palliative Care and Euthanasia
- Palliative Care Drugs
- Palliative Care in Oncology
- Palliative Care Medications
- Palliative Care Nursing
- Palliative Medicare
- Palliative Neurology
- Palliative Oncology
- Palliative Psychology
- Palliative Sedation
- Palliative Surgery
- Palliative Treatment
- Pediatric Palliative Care
- Volunteer Palliative Care
Recommended Journals
- Journal of Cardiac and Pulmonary Rehabilitation
- Journal of Community & Public Health Nursing
- Journal of Community & Public Health Nursing
- Journal of Health Care and Prevention
- Journal of Health Care and Prevention
- Journal of Paediatric Medicine & Surgery
- Journal of Paediatric Medicine & Surgery
- Journal of Pain & Relief
- Palliative Care & Medicine
- Journal of Pain & Relief
- Journal of Pediatric Neurological Disorders
- Neonatal and Pediatric Medicine
- Neonatal and Pediatric Medicine
- Neuroscience and Psychiatry: Open Access
- OMICS Journal of Radiology
- The Psychiatrist: Clinical and Therapeutic Journal
Article Tools
Article Usage
- Total views: 12007
- [From(publication date):
November-2015 - Apr 02, 2025] - Breakdown by view type
- HTML page views : 11024
- PDF downloads : 983