Research Article Open Access
A Novel Procedure to Process Extracted Teeth for Immediate Grafting of Autogenous Dentin
Itzhak Binderman1*, Gideon Hallel2, Casap Nardy3, Avinoam Yaffe4, and Lari Sapoznikov21Department of Oral Biology, School of Dental Medicine and Department of Bio-Engineering, Faculty of Engineering, Tel Aviv University, Tel Aviv, Israel
2Private Practice, Tel Aviv, Israel
3Departments of Maxillofacial Surgery and Hebrew University Jerusalem, Israel
4Hadassah Faculty of Dental Medicine, Hebrew University Jerusalem, Israel
- Corresponding Author:
- Itzhak Binderman
Department of Oral Biology
School of Dental Medicine
Tel Aviv University, Ramat Aviv 69978, Tel Aviv, Israel
E-mail: Binderman.itzhak@gmail.com
Received date June 05, 2014; Accepted date October 13, 2014; Published date October 17, 2014
Citation: Binderman I, Hallel G, Nardy C, Yaffe A, Sapoznikov L (2014) A Novel Procedure to Process Extracted Teeth for Immediate Grafting of Autogenous Dentin. J Interdiscipl Med Dent Sci 2:154. doi: 10.4172/2376-032X.1000154
Copyright: © 2014 Binderman I, et al. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.
Visit for more related articles at JBR Journal of Interdisciplinary Medicine and Dental Science
Abstract
Background: Extracted teeth are still considered a clinical waste and therefore being discarded. It is evident that chemical composition of dentin is similar to bone. Following tooth replantation the tooth is replaced by bone then followed by root resorption and ankyloses and finally integrated into the surrounding alveolar bone.
Aims: Here we present a novel procedure in a clinical setting that employs freshly extracted teeth that are processed into a bacteria-free particulate dentin, and then grafted immediately into extraction sites or bone deficiencies.
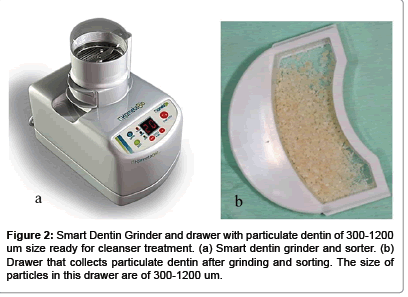
Methods: The procedure consists of reducing any restorations, caries or debris. The clean and dry tooth, mostly dentin, is immediately grinded using a specially designed 'Smart Dentin Grinder'. The dentin particulate of 300-1200 um is sieved through a special sorting system. The sorted particulate dentin is immersed in basic alcohol cleanser in a sterile container to dissolve all organic debris and bacteria. Then, the particulate is washed by sterile saline. The bacteria-free particulate dentin is ready for immediate grafting into extraction sites or into bone defect sites.
Results: During the period of two years, more than 100 procedures were performed, most of which for the purpose of preservation of alveolar bone. In those patients, implant insertion was possible as soon as 2-3 month after grafting of autogenous dentin. On x-rays and biopsy of grafting sites a dense dentin-bone composite was found. No wound healing complications were observed.
Conclusion: Autogenous mineralized dentin particulate grafted immediately after extractions should be considered as the gold standard for socket preservation, bone augmentation in sinuses and bone defects.
Keywords
Smart dentin grinder and sorter; Autogenous particulate dentin graft; Socket preservation.
Introduction
Tooth extraction is one of the most widely performed procedures in dentistry and it has been historically well documented that this may induce significant dimensional changes of the alveolar ridge [1]. In this review, Horowitz et al. [1] stated that less ridge resorption is occurring when alveolar ridge preservation procedures were used versus the placement of no graft material in fresh alveolar sockets. If performed inadequately, the resulting deformity can be a considerable obstacle to the esthetic, phonetic, and functional results. In dentistry allogeneic bone and synthetic mineral materials are the main source for grating in bone. However, fresh autogenous bone graft is still considered gold standard since it exhibits bioactive cell instructive matrix properties and is non-immunogenic and non – pathogenic in spite of the need for harvesting bone and possible morbidity resulting from it.
It is well known that jaw bones, alveolar bone and teeth develop from cells of the neural crest and that many proteins are common to bone, dentin, and cementum [2,3]. It is therefore not surprising that dentin that comprise of more than 85% of tooth structure can serve as native bone grafting material. Interestingly, Schmidt-Schultz and Schultz [4] found that intact growth factors are conserved even in the collagenous extracellular matrix of ancient human bone and teeth. In previous reports, a method for processing bovine dentin into particulate and sterile grafting material for preservation of alveolar bone was described and used in animal studies [5-7]. It is therefore evident that teeth become grafts that are slowly and gradually replaced by bone [8]. Currently, all extracted teeth are considered a clinical waste and therefore are simply discarded. Recently, several studies reported that extracted teeth from patients that undergo a process of cleaning, grinding, demineralization and sterilization is a very effective graft to fill alveolar bone defects of same patient [9-11]. However, this procedure is much time consuming since the graft is ready many hours and days after extraction. We present here a modified procedure, in a clinical setting that employs freshly extracted teeth, by recycling them into a bacteriafree particulate autogenous mineralized dentin for immediate grafting. A ‘Smart Dentin Grinder’™ was devised to grind and sort extracted teeth into a specific size dentin particulate. A chemical cleanser is applied to process the dentin particulate into a bacteria free graft during 15-20 minutes. This novel procedure is indicated mainly in cases when teeth are extracted because of periodontal reasons and partially or totally impacted teeth. Teeth that underwent root canal fillings should not be employed in this procedure because of foreign materials contamination. On the other hand, crowns and fillings can be reduced and clean dentin of tooth crown can be processed for immediate grafting.
Methods
Procedure from tooth extraction to grafting of particulate dentin
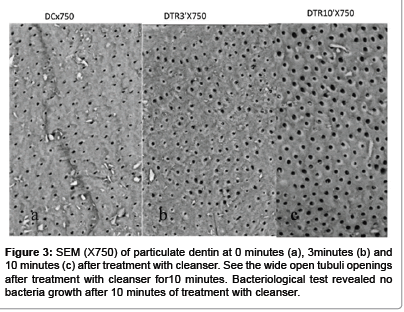
Teeth without root canal fillings that are extracted due to advanced periodontal bone loss or other indications like wisdom teeth or orthodontics indications, are prepared for immediate grafting. Immediately after extraction, restorations like crowns and fillings should be cut off or removed. Also carious lesions and discolored dentin or remnants of Periodontal ligament (PDL) and calculus should be reduced by tungsten bur (Figure 1a and 1b). We find that high speed tungsten carbide burs are most efficient for this process. The roots could be split in case of multi-rooted teeth. Clean teeth including crown and root dentin are dried by air syringe, put into a grinding sterile chamber of a newly designed ‘Smart Dentin Grinder’™ (Figure 2a). The ‘Smart Dentin Grinder’™ (SDG) is capable in 3 seconds to grind the roots and then by vibrating movement of the grinding chamber for 20 seconds the particles of less than 1200 μm fall through a sieve to a lower chamber that keeps particles between 300-1200 μm (Figure 2b). The particles less than 300 μm fall into a waist drawer. This fine particulate (less than 300 μm) is considered as a non-efficient particulate size for bone grafting. This grinding and sorting protocol is repeated to grind the remaining teeth particles left in grinding chamber. In the collecting drawer chamber dentin particles between 300-1200 μm are collected (Figure 2b). The particulate dentin from the drawer is immersed in basic alcohol for 10 minutes, in a small sterile glass container. The basic alcohol cleanser consists of 0.5M of NaOH and 30% alcohol (v/v), for defatting, dissolving all organic debris, bacteria and toxins of the dentin particulate. The efficiency of the cleanser to dissolve all the organic debris from dentin particulate including dentin tubules is demonstrated in Figure 3. The SEM picture shows wide open and clean tubules after 10 minutes of cleanser treatment (Figure 3c). After decanting the basic alcohol cleanser, the particulate is washed twice, in sterile phosphate buffered saline (PBS). The PBS is decanted leaving wet particulate dentin ready to graft into freshly extracted sockets or into alveolar bone defects or in procedures of augmenting maxillary sinus. The process from tooth extraction until grafting takes approximately 15-20 minutes. It should be noted, that the efficiency of selecting the dentin particulate of specific size for grafting is more than 95%. It is obvious that the volume of the particulate dentin is more than twice of the original root volume. Alternatively, the wet particulate can be put on a hot plate (140â�?¦C) for 5 minutes and the dry bacteria-free particulate autologous dentin that can serve for immediate or future grafting procedures.
Results
Clinical evaluation
During the period of 2 years, more than 100 dentists are employing the present procedure for preparing autogenous dentin particulate from extracted teeth for immediate grafting in same patient. It should be noted that teeth that underwent root canal treatment were discarded. When intact teeth were processed the enamel and cementum were included. Here, we present typical case presentations where teeth were extracted and processed into bacteria-free particulate autogenous tooth dentin for immediate grafting in same patient.
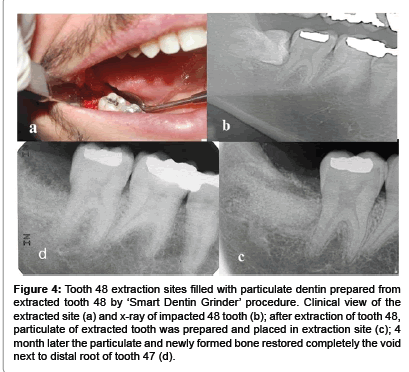
From a series of 16 wisdom teeth that included partially impacted, horizontally impacted and others that their crown was destroyed by caries were processed by SDG procedure and immediately grafted in the extraction sockets. We present here a horizontal impacted tooth 48 that was in close proximity to distal root surface of 47 (Figure 4b), creating a deep void. The surgically extracted tooth 48, exposed the distal root surface of 47 almost denuded from bone tissue. Here, we processed immediately the tooth 48 into particulate graft which filled totally the extraction site (Figure 4c). The healing and recovery after surgical procedure and grafting was without complications. A follow up after 4 month revealed a normal pattern of marginal gingiva around the tooth 47. Probing was normal 1-2mm in depth. On x-ray distal to tooth 47, new bone and particulate dentin was integrated into bone restoring completely the site of extraction and a distal bone support of tooth 47 ( Figure 4d).
Figure 4:Tooth 48 extraction sites filled with particulate dentin prepared from extracted tooth 48 by ‘Smart Dentin Grinder’ procedure. Clinical view of the extracted site (a) and x-ray of impacted 48 tooth (b); after extraction of tooth 48, particulate of extracted tooth was prepared and placed in extraction site (c); 4 month later the particulate and newly formed bone restored completely the void next to distal root of tooth 47 (d).
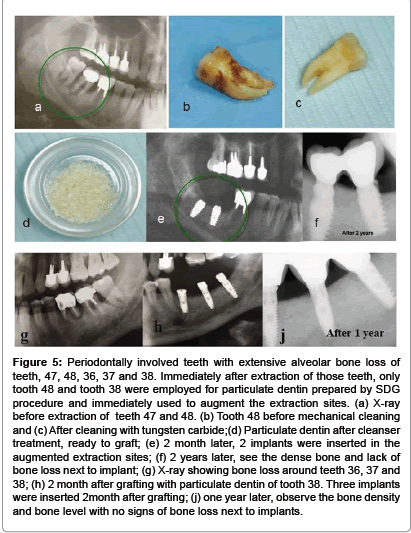
Another series of 37 extracted teeth because of poor periodontal attachment, bone loss and mobility is presented here by a patient, 56 years old male with localized advanced periodontal condition in posterior parts of mandible. Teeth 47 and 48 were extracted and the granulation tissue was removed exposing bone tissue walls. Tooth 47 had a root canal filling and therefore was discarded. Tooth 48 processed into particulate dentin by the SDG device and prepared for immediate grafting in the extraction sites. The grafting of one tooth produced volume of particulate dentin that was adequate to overfill the extraction site of sockets. A Choukrouns PRF membrane (platelet rich fibrin) was prepared from patient blood [12] to cover the graft. Mucoperiosteum was sutured to PRF, avoiding tension of tissues. An improved healing was achieved because of the PRF membrane. 2 month later two implants were placed, followed by a cemented bridge of 47-48 crowns. After two years, clinical and x-ray follow up revealed a very radiopaque bone integrated into implants, most possibly consisting of bone-dentin producing a very solid support for implants (Figure 5). A similar procedure was performed in same patients left side of lower jaw. X-ray showing bone loss around teeth 36, 37 and 38 (Figure 5g). Two months after grafting with particulate dentin of tooth 38 three implants were inserted (Figure 5h), and one year later observe the bone density and bone level with no signs of bone resorption at the crest after restoration (Figure 5j).
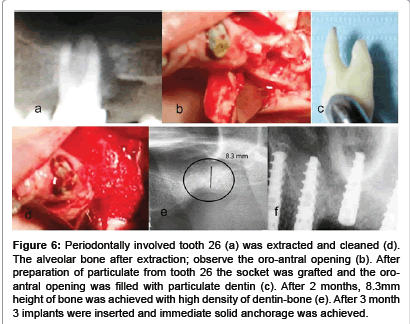
Autogenous dentin particulate can serve as superior grafting matrix for augmenting bone in maxillary sinuses, as is presented in the next case. Alveolar bone loss with infrabony pockets that extended into the maxillary sinus of tooth 26 (Figure 6). Tooth 26 was extracted, cleaned and processed into a bacteria free particulate dentin (Figure 6d). An immediate grafting of the extraction socket was performed and the tract into the sinus was occluded by the particulate dentin. Closure of the wound and sutures of mucoperiosteum flap was performed. Healing was normal and three month later an alveolar ridge of minimum 8.3 mm height was achieved, allowing insertion of 3 implants. It should be noted that one molar of tooth 26 produced at least 2cc of particulate dentin which allowed augmenting the extraction socket and part of sinus. Moreover, we found that autogenous dentin grafting enables to insert implants after 3 month in the upper jaw, because the new bone that was integrated with particulate dentin produced a solid support for implants. Loading of implants followed. During preparation of a slot for implant insertion, a core of bone was recovered from the grafted socket site. The histology revealed new bone integrated with grafted dentin producing bone-dentin interface and connectivity (Figure 7).
Figure 5:Periodontally involved teeth with extensive alveolar bone loss of teeth, 47, 48, 36, 37 and 38. Immediately after extraction of those teeth, only tooth 48 and tooth 38 were employed for particulate dentin prepared by SDG procedure and immediately used to augment the extraction sites. (a) X-ray before extraction of teeth 47 and 48. (b) Tooth 48 before mechanical cleaning and (c) After cleaning with tungsten carbide;(d) Particulate dentin after cleanser treatment, ready to graft; (e) 2 month later, 2 implants were inserted in the augmented extraction sites; (f) 2 years later, see the dense bone and lack of bone loss next to implant; (g) X-ray showing bone loss around teeth 36, 37 and 38; (h) 2 month after grafting with particulate dentin of tooth 38. Three implants were inserted 2month after grafting; (j) one year later, observe the bone density and bone level with no signs of bone loss next to implants.
Figure 6:Periodontally involved tooth 26 (a) was extracted and cleaned (d). The alveolar bone after extraction; observe the oro-antral opening (b). After preparation of particulate from tooth 26 the socket was grafted and the oroantral opening was filled with particulate dentin (c). After 2 months, 8.3mm height of bone was achieved with high density of dentin-bone (e). After 3 month 3 implants were inserted and immediate solid anchorage was achieved.
Discussion
More than 40 years ago, autogenous teeth were routinely transplanted into extraction sockets when possible. It is evident that transplanted teeth that are ankylosed in jaw bone undergo replacement resorption by bone, during 5-8 years [13]. In addition, it is well documented that avulsed teeth that are implanted back into their sockets undergo firm reattachment by bone which is formed directly on root dentin or cementum, leading to ankylosis [14]. An ankylosed root is continuously resorbed and replaced by bone, eventually resorbing the entire root, while the alveolar process is preserved during this period and later. In a recent review, Malmgren [15] stressed that ankylosed teeth that are treated by decoronation, the alveolar ridge is maintained in the buccal/palatinal direction, while vertical height is even increased [16]. Our results reveal similar interaction between mineralized dentin and osteogenic cells that attach and produce mineralized bone matrix directly on the dentin graft.
A Tooth Bank in Korea provides service that prepares autogenic demineralized dentin matrix graft as block-type or granular-type [10,11,17], delaying the grafting procedure from several hours to several days and therefore needs an additional surgical session. Although demineralized dentin exposes matrix derived growth and differentiation factors for effective osteogenesis, the newly formed bone and residual demineralized dentin are weak to support implant anchorage. In contrast, our SDG procedure allows preparation of bacteria-free particulate dentin from freshly extracted autologous teeth, ready to be employed as autogenous graft immediately, in the same session. Mineralized dentin particles have the advantage to maintain its mechanical stability, allowing early loading after grafting in fresh sockets and bone defects. Moreover, in spite of delayed inductive properties [18,19], the mineralized dentin is firmly integrated with newly formed bone, creating a solid site for anchorage of dental implants. In fact, our clinical data indicate that implant insertion and loading can be performed in lower and upper jaws 2-3 month after grafting of dentin. Since the mineralized dentin is very slowly remodeled [18,20,21] in comparison to cortical bone or most biomaterials the esthetic and structure pattern of the alveolar crest and mucoperiosteum is maintained for years.
Teeth and jawbone have a high level of affinity, having similar chemical structure and composition. Therefore, we and others [10,11,17] propose that extracted non-functional teeth or periodontally involved teeth should not be discarded anymore. Extracted teeth can become an autogenous dentin ready to be grafted within 15 minutes after extraction. We consider autogenous dentin as the gold standard graft for socket preservation, bone augmentation in sinuses or filling bone defects.
Key Findings
Autogenous mineralized dentin particulate that is grafted immediately after extractions should be considered as the gold standard for socket preservation, bone augmentation in sinuses or filling bone defects.
Footnotes
‘Smart Dentin Grinder’™ is distributed by Kometa Bio ltd., Holon, Israel.
Acknowledgements
We acknowledge the help of providing the authors with documented case reports where autogenous dentin graft was performed using the present procedure.
Conflict of Interest
We certify that IB and LR have shares in Kometa Bio Company and helped to develop the Smart Dentin Grinder™. GH, CN and AY have no conflict of interest. GH, CN and AY participated actively in providing clinical cases and their follow up.
References
- Horowitz R, Holtzclaw D, Rosen PS (2012) A review on alveolar ridge preservation following tooth extraction.J Evid Based Dent Pract 12: 149-160.
- Donovan MG, Dickerson NC, Hellstein JW, Hanson LJ (1993) Autologous calvarial and iliac onlay bone grafts in miniature swine.J Oral MaxillofacSurg 51: 898-903.
- Qin C, Brunn JC, Cadena E, Ridall A, Tsujigiwa H, et al. (2002) The expression of dentin sialophosphoprotein gene in bone.J Dent Res 81: 392-394.
- Schmidt-Schultz TH, Schultz M (2005) Intact growth factors are conserved in the extracellular matrix of ancient human bone and teeth: a storehouse for the study of human evolution in health and disease.BiolChem 386: 767-776.
- Fugazzotto PA, De Paoli S, Benfenati SP (1986) The use of allogenic freeze-dried dentin in the repair of periodontal osseous defects in humans.Quintessence Int 17: 461-477.
- Nampo T, Watahiki J, Enomoto A, Taguchi T, Ono M, et al. (2010) A new method for alveolar bone repair using extracted teeth for the graft material.J Periodontol 81: 1264-1272.
- Qin X, Raj RM, Liao XF, Shi W, Ma B, et al. (2014) Using rigidly fixed autogenous tooth graft to repair bone defect: an animal model.Dent Traumatol 30: 380-384.
- Hasegawa T, Suzuki H, Yoshie H, Ohshima H (2007) Influence of extended operation time and of occlusal force on determination of pulpal healing pattern in replanted mouse molars.Cell Tissue Res 329: 259-272.
- Kim YK, Kim SG, Byeon JH, Lee HJ, Um IU, et al. (2010) Development of a novel bone grafting material using autogenous teeth.Oral Surg Oral Med Oral Pathol Oral RadiolEndod 109: 496-503.
- Kim SG, Kim YK,Lim SC,Kim KW, Um IW (2011) Histomorphometric analysis of bone graft using autogenous tooth bone graft. Implantology15: 134-141.
- Murata M, Akazawa T, Mitsugi M, Um, IW, Kim, KW & Kim, YK (2011) Human Dentin as Novel Biomaterial for Bone Regeneration, Biomaterials - Physics and Chemistry, Rosario Pignatello, ISBN: 978-953-307-418-4, INTECK Publisher, Croatia. p127-140.
- Cieslik-Bielecka A, Choukroun J, Odin G, DohanEhrenfest DM (2012) L-PRP/L-PRF in esthetic plastic surgery, regenerative medicine of the skin and chronic wounds.Curr Pharm Biotechnol 13: 1266-1277.
- Sperling I, Itzkowitz D, Kaufman A, Binderman I (1986) A new treatment of heterotransplanted teeth to prevent progression of root resorption.Endod Dent Traumatol 2: 117-120.
- Andersson L, Bodin I, Sörensen S (1989) Progression of root resorption following replantation of human teeth after extended extraoral storage.Endod Dent Traumatol 5: 38-47.
- Malmgren B (2013) Ridge preservation/decoronation.J Endod 39: S67-72.
- Park CH1, Abramson ZR, Taba M Jr, Jin Q, Chang J, et al. (2007) Three-dimensional micro-computed tomographic imaging of alveolar bone in experimental bone loss or repair.J Periodontol 78: 273-281.
- Kim YK (2012) Bone graft material using teeth. Journal of the Korean Association of Oral and Maxillofacial Surgeons, 38: 134-138.
- Yeomans JD, Urist MR (1967) Bone induction by decalcified dentine implanted into oral, osseous and muscle tissues.Arch Oral Biol 12: 999-1008.
- Huggins C, Wiseman S, Reddi AH (1970) Transformation of fibroblasts by allogeneic and xenogeneic transplants of demineralized tooth and bone.J Exp Med 132: 1250-1258.
- Kim YK, Kim SG2, Yun PY1, Yeo IS3, Jin SC4, et al. (2014) Autogenous teeth used for bone grafting: a comparison with traditional grafting materials.Oral Surg Oral Med Oral Pathol Oral Radiol 117: e39-45.
- Andersson L (2010) Dentin xenografts to experimental bone defects in rabbit tibia are ankylosed and undergo osseous replacement.Dent Traumatol 26: 398-402.
Relevant Topics
- Cementogenesis
- Coronal Fractures
- Dental Debonding
- Dental Fear
- Dental Implant
- Dental Malocclusion
- Dental Pulp Capping
- Dental Radiography
- Dental Science
- Dental Surgery
- Dental Trauma
- Dentistry
- Emergency Dental Care
- Forensic Dentistry
- Laser Dentistry
- Leukoplakia
- Occlusion
- Oral Cancer
- Oral Precancer
- Osseointegration
- Pulpotomy
- Tooth Replantation
Recommended Journals
Article Tools
Article Usage
- Total views: 18653
- [From(publication date):
December-2014 - Apr 03, 2025] - Breakdown by view type
- HTML page views : 13589
- PDF downloads : 5064