A New Focus on Preconception Healthcare and the Life Course Theory of Health
Received: 02-Mar-2018 / Accepted Date: 13-Mar-2018 / Published Date: 20-Mar-2018 DOI: 10.4172/2471-9846.1000216
Abstract
Preconception healthcare (PCHC) is a set of prevention and health promotion interventions to reduce reproductiveaged women’s health risks before conception and improve birth outcomes. This timelier intervention is underutilized in the United States (U.S.). The current health framework integrates the Fetal Origin of Adult Disease (FOAD) theory, the Developmental Origin of Health and Disease (DOHaD) and the Life Course Theory of health (LCT). This continuous integrative health framework emphasizes the important role of PCHC on birth outcomes and on reducing the burden of adult chronic diseases in the population
Keywords: Preconception healthcare; Fetal origin of adult diseases; Life course theory of health; Adult chronic diseases
Introduction
Preconception healthcare (PCHC) includes a set of evidence-based preventive and health promotion interventions to improve reproductiveaged women and men health before conception [1,2]. Infant mortality and adverse birth outcomes remain high and show great disparities along racial and socioeconomic lines in the United States (U.S.). Most of the leading causes of adverse birth outcomes and infant mortality are associated with women’s health and risk behaviors that are preventable through PCHC [3]. The concept of preconception healthcare was first described almost two centuries ago. In his early 19th century, children’s medical treatise, Dr. Dewees [4], the American pioneer in perinatal health, proposed that the medical treatment of children should begin with the earliest formation of the embryo and should include the mother before marriage as well as during pregnancy. Despite this early recognition, PCHC has not become part of the routine care of most reproductive-aged women.
Preconception healthcare today
Almost two centuries later, in 2006, the Center for Disease Control and Prevention (CDC) published PCHC recommendations [1,2]. Despite good evidence supporting the CDC recommendations, PCHC is underutilized in the U.S. [5,6]. Many reproductive-aged women are not aware of the CDC recommendations, nor do they receive all of the recommended preconception care interventions. An assessment of PCHC interventions among rural women revealed that only one-half received counselling about contraception, one in three were offered sexually transmitted infections (STIs) screening and one in four received counseling about the effects of body weight, prescription drugs, folic acid intake and substance use impact on birth outcomes. Only one in five received information on rubella and hepatitis B immunizations or about the effects of illegal drugs in maternal and fetal outcomes and wellbeing. Most surprisingly, among those who were diabetic at the time of the assessment, only 6.2% had discussed the need to have their diabetes under control before planning a pregnancy [5] (Table 1).
| Reproductive-life planning** |
|---|
| High blood pressure Folic acid supplementation |
| Rubella seronegativity |
| Hepatitis B vaccination immunity |
| Overweight and obesity |
| Underweight |
| Anemia |
| Tobacco and Alcohol use** |
| Illegal drug use** |
| Prescription drug use (especially isoretinoids, anti-epileptics, oral anticoagulants) |
| Diabetes and diabetes control |
| Hypothyroidism |
| Phenylketonurea (PKU) |
| HIV/AIDS |
| Sexually transmitted infections (Chlamydia, gonorrhea, syphilis)** |
| Zika virus** |
| Environmental chemical exposures** |
| Physical and emotional abuse |
*MMWR-Recommendations and Reports-Center for Disease Control and Prevention
(CDC 2006, 2012, 2017)
**Male recommendations
Table 1: Recommendations to improve women’s preconception healthcare.
Researchers have investigated why PCHC has not become part of the routine care for all reproductive-aged women in the U.S. Potential explanations included lack of time during patient visits, lack of reimbursement, lack of sufficient professional training and not feeling comfortable talking with women about improving their health before pregnancy [7]. One additional explanation could be the lack of health policy in favor of comprehensive PCHC. Policy makers argue that there is not enough evidence about the benefits of providing PCHC on birth outcomes to support a policy; however, there is ample evidence supporting the benefits of the individual PCHC interventions on improving birth outcomes. Some of these interventions include adequate folic acid intake, healthy pre-pregnancy weight, tobacco and alcohol abstinence, tight diabetes control and rubella and hepatitis B immunizations [1-3].
Some progress has been made in facilitating the integration of PCHC into the routine primary care of reproductive-aged women. Professional organizations such as the American Academy of Family Physicians have published updated PCHC guidelines for primary healthcare providers, emphasizing the importance of PCHC in the continuum of women’s care [8]. These guidelines include key clinical recommendations for practice, the level of evidence that supports them and Continue Medical Education self-assessments for primary healthcare clinicians. Additional resources for healthcare providers are available from the National Preconception Care and Health Care Initiative (national public and private partnership led by the Center for Maternal and Infant Health at the University of North Carolina Chapel Hill [9]. Recently, the US Department of Veteran Affairs developed a preconception healthcare mobile app to guide healthcare providers in counseling women before pregnancy [10]. In addition, the US Department of Health and Human Services/Women Health provides resources for women, including a checklist that they can use to prompt a conversation about PCHC with their healthcare provider [11]. Some policy changes have also occurred that emphasize including prevention and health promotion in primary care, which might open the door to providing PCHC to more women [2,12].
For the past seven years, our research has focused on increasing women’s PCHC knowledge and on empowering them to seek PCHC. In a recently completed intervention study, we used a quasi-experimental, non-randomized, two-group design to evaluate the effect of a PCHC educational program on PCHC knowledge and self-efficacy among rural reproductive-aged women. The educational intervention followed the Health Belief Model (HBM). A mixed-model ANOVA (alpha=0.05) assessed the effect of the intervention on PCHC knowledge and HBM scores. Women 18 to 45 years of age (N=85) participated in the study.
Post-intervention PCHC knowledge (p=0.02) and HBM summary score (p=0.009) increased in the study group. The study group demonstrated an increase in PCHC knowledge (p<0.001) and in the HBM summary scores (p=0.015) when evaluated over time. The study supported that providing PCHC education to rural reproductive-aged women increased their knowledge and self-efficacy in accessing PCHC. We are currently working on using available innovative technology to reach urban and rural reproductive-aged women with PCHC education tailored to their needs.
Integrating preconception healthcare in the life course theory
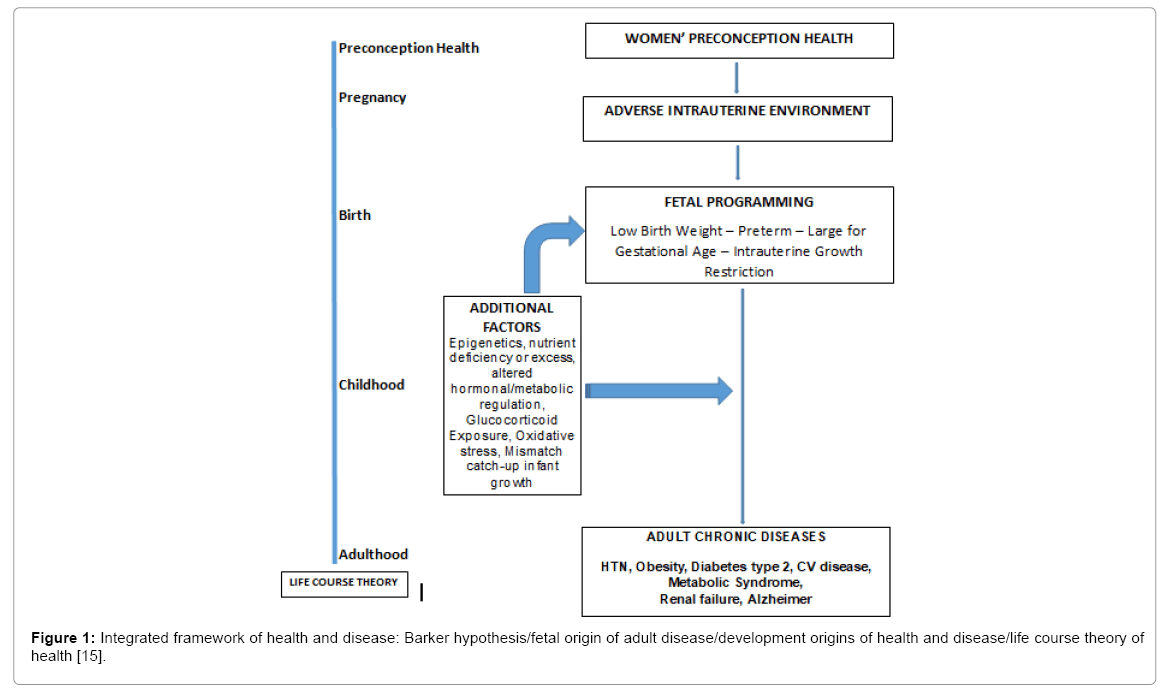
There is an additional benefit to provide PCHC to all reproductiveaged women aside from improving birth outcomes and infant mortality. These same interventions have the potential to reduce adult chronic diseases. Cardiovascular disease, cancer and diabetes are leading causes of death and disability in the U. S. First proposed by Dr. Barker, the Fetal Origins of Adult Disease (FOAD) theory describes that exposure to an adverse event while in utero increases the risk of adult diseases in the child [13]. This impact is seen through generations, in babies born to mothers who themselves suffered adverse exposures earlier in life [13]. Since Barker’s theory was proposed, extensive animal models and human cohort studies evaluated and supported this theory [14]. Exposure to adverse events during critical periods in human development causes physiological and metabolic responses that persist later in life and cause disease. Evidence supports that extremes in fetal weight are associated with coronary artery disease, stroke, hypertension, kidney failure, dyslipidemia, insulin resistance, cancer, osteoporosis and some mental disorders [15]. The current conceptual framework that explains health and disease integrates Barker’s FOAD theory, the Developmental Origin of Health and Disease (DOHaD) concept and the Life Course Theory (LCT) [16]. In this framework, nutrition extremes, epigenetics modifications, oxidative stress and increased corticoids exposure coupled with mismatch compensatory growth after low birth weight; increase the risk of chronic adult disease. This continuous framework recognizes that programing events (biological and social determinants of health) can act before conception, during pregnancy and after birth and can explain adult diseases as well as health disparities in the population. The LCT framework contributes to the understanding of the pathogenesis of chronic disease and identifies opportunities for more timely interventions to reduce the burden of adult diseases, including PCHC (Figure 1).
Figure 1: Integrated framework of health and disease: Barker hypothesis/fetal origin of adult disease/development origins of health and disease/life course theory of health [15].
Conclusion
Early prenatal care reduces pregnancy complications that can cause adverse birth outcomes, which in turn can increase the risk of adult chronic disease; however, gestation can be ongoing for six to eight weeks when prenatal care starts. Preconception healthcare represents a timelier primary care intervention available to all health providers caring for women. With PCHC as a component of the routine care for reproductive-aged women, we would be able to collect long-term data on PCHC impact on birth outcomes and its contribution to the subsequent reduction in the burden of adult chronic disease.
References
- Centers for Disease Control and Prevention (2006) Recommendations to improve preconception health and health care-United States: A report on the CDC/ATSDR preconception care workgroup and the select panel on preconception care.
- Centers for Disease Control and Prevention (2012) Preconception health and health care: Information for health professionals.
- World Health Organization (2013) Meeting to develop a global consensus on preconception care to reduce maternal and childhood mortality and morbidity.
- Dewees WP (1958) A treatise on the physical and medical treatment of children. Philadelphia: Blanchard and Lea.
- Lammers CR, Hulme PA, Wey H, Kerkvliet J, Arunachalam SP (2017) Understanding women's awareness and access to preconception health care in a rural population: A cross sectional study. J Community Health 42: 489-499.
- Frey KA, Files JA (2006) Preconception health care: What women know and believe. Matern Child Health J 10: S73-S77.
- Tough SC, Clarke M, Hicks M, Cook J (2006). Pre-conception practices among family physicians and obstetrician-gynecologists: Results form a national survey. J Obstet Gynaecol Can 28: 780-788.
- Farahi N, Zolotor A (2013) Recommendations for preconception counseling and care. Am Fam Physician 88: 499-506.
- National preconception care and health care (2018) University of North Carolina Chapel Hill.
- U.S. Department of Veterans Affairs (2018) Health care professionals professional apps. Preconception health care.
- Curtis MG (2010) Preconception care: Clinical and policy implications of the preconception agenda. J Clin Outcomes Manag 17: 167-172.
- Barker DJ (2004) The developmental origins of adult disease. J Am Coll Nutr 23: 588S-595S.
- Calkins K, Devaskar SU (2011) Fetal origins of adult disease. Curr Probl Pediatr Adolesc Health Care 41: 158-176.
- Brenseke B, Prater MR, Bahamonde J, Gutierrez JC (2013) Current thoughts on maternal nutrition and fetal programming of the metabolic syndrome. J Pregnancy 368461: 1-13.
- Cheng TL, Solomon BS (2014) Translating life course theory to clinical practice to address health disparities. Matern Child Health J 18: 389-395.
Citation: Lammers C (2018) A New Focus on Preconception Healthcare and the Life Course Theory of Health. J Comm Pub Health Nursing 4:216. DOI: 10.4172/2471-9846.1000216
Copyright: © 2018 Lammers C. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.
Share This Article
Recommended Journals
Open Access Journals
Article Tools
Article Usage
- Total views: 6729
- [From(publication date): 0-2018 - Feb 22, 2025]
- Breakdown by view type
- HTML page views: 5912
- PDF downloads: 817