A Medical-Design Collaboration in the Age of COVID-19: Mobile Health for Rural Populations
Received: 01-Sep-2022 / Manuscript No. jcmhe-22-75190 / Editor assigned: 05-Sep-2022 / PreQC No. jcmhe-22-75190 (PQ) / Reviewed: 19-Sep-2022 / QC No. jcmhe-22-75190 / Revised: 26-Sep-2022 / Manuscript No. jcmhe-22-75190 (R) / Published Date: 03-Oct-2022
Abstract
Purpose: The COVID-19 pandemic has presented new infection mitigation challenges and exacerbated existing health inequities. Mobile health care has the potential to increase access to high quality culturally responsive care. We sought to demonstrate that such care can be provided safely by engaging space design experts and community based organizations (CBOs) in the design and implementation of a mobile health initiative.
Materials and methods: Mobile clinics were organized by CBOs serving migrant farmworkers and university based health providers. Community members were informed of clinic dates and locations through social media, informal networks, and word of mouth. An architectural designer planned the clinic space and flow of pedestrian traffic for safe social distancing.
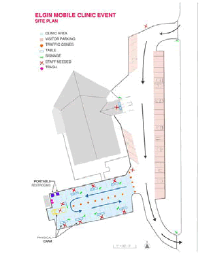
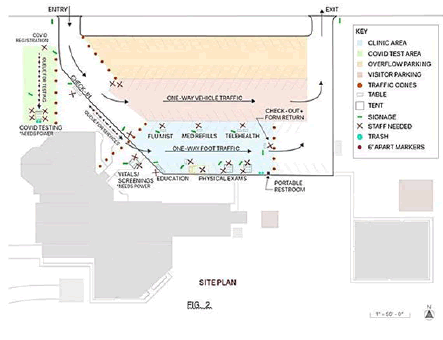
Results: Clinic schematics were created by the architectural designer and used for foot traffic flow. Two mobile health clinics serving 94 patients were held during a peak COVID-19 infection period in 2020. Events held in 2021 utilized the same designs and were expanded to include additional services and vaccines in response to feedback received from the 2020 clinics.
Conclusion: Partnerships developed with community based and faith based organizations can increase access and health equity by leveraging trust built over time and incorporating care into community events. Despite challenges with seeking health care during the COVID-19 pandemic, health care events for testing and/or vaccinations can be safely performed by utilizing practices based in architectural design to minimize face to face contact. Mobile clinic programs can be done safely and effectively during the pandemic so long as emphasis is placed on infection mitigation through clinic design. This model can be used in health events where respiratory infection risk is high.
Keywords: COVID-19; Mobile health; Healthcare design; Health equity
Introduction
Designing safe mobile clinics in the age of COVID-19: A medical design collaboration
The COVID-19 pandemic has presented new infection mitigation challenges within traditional healthcare settings and has exacerbated existing inequalities among Black, Indigenous, and People of Color (BIPOC) communities. These traditionally underserved groups have also seen disproportionately high numbers of COVID-19 cases, due in part to social determinants of health such as poverty, working essential jobs and higher housing density in multi-family and multi-generational housing. For many of these communities living in rural areas, access to quality medical care is particularly challenging due to lack of transportation, insurance, and/or access to culturally aware and affordable medical care [1,2].
Mobile healthcare, which we define as providing care where people live, work, and play, can help bridge the gap and increase health equity. In particular, partnerships between community based organizations (CBOs) or faith based organizations (FBOs) and university programs have the potential to improve health equity because of the community trust of CBOs/FBOs and the access to grant funding and learners in the university setting. Approximately 2,000 mobile health systems exist in the US, according to the Mobile Health Map database, many of which have proven successful in improving health outcomes and are seen as a necessary part of the healthcare system as a whole [3,4]. Healthcare access for marginalized populations, even during a pandemic, can be improved by bringing health care to the patient through mobile clinics.
As with all healthcare delivery in the pandemic-era, special infection prevention precautions are essential. For this reason, we developed a partnership between interprofessional health science providers in the University of Minnesota’s Office of Academic Clinical Affairs and an architectural designer to create a mobile space to provide vital services while mitigating infection risk. This team, along with a CBO working directly with migrant farmworker families, successfully organized two mobile health clinics in Southern Minnesota in September of 2020. It is with this experience that we hope to demonstrate that operating mobile health clinics during a pandemic can be done safely and still be effective when emphasis is placed on clinic design and fostering relationships with CBOs.
Materials and Methods
Clinic dates and locations were chosen in collaboration with the CBO via remote video conferences. Detailed clinic schematics were created by the team architectural designer based on in person site visits and feedback from other team members and partners. A preliminary scaled site plan was created using Google Maps and Adobe Illustrator, and the finalized schematics were used for set up and orchestration of patient/vehicle flow. University based Health Sciences volunteers were recruited via email and word of mouth. Skills, interests, and availability of volunteers were assessed via a Google Forms survey. Clinic supplies, PPE, and medical providers were university based. Bilingual nurses, Spanish interpreters, and ancillary staff were provided by the CBO. Advertising for the two clinic events was done through the local community organization’s network of families 3-5 days in advance of the clinics [5]. Feedback from volunteers after the event was received during both the debriefing session immediately after the clinics and through an anonymous Google Form sent one day following the event. Feedback from patients was received via an optional opt in phone call after their clinic visit.
The Centers for Disease Control (CDC) has recommended physical distancing more commonly termed social distancing since COVID-19 surge in the US in Spring 2020. Thus, in designing the mobile clinic, it was imperative that we also took measures to limit unnecessary interaction and provided adequate space for both patients and providers [6].
Results
We utilized schematics created by an architectural designer to provide necessary safety measures for COVID-19 (Figures 1 and 2), including adequate space for patient queues, one-way vehicle/pedestrian traffic, and appropriate distance between each service station. Due to the unilateral nature of movement through the clinic, patients did not come into contact with other individuals attending the clinic, therefore removing another potential risk of COVID-19 transmission. The one-way traffic also allowed all patients to encounter the COVID-19 education booth. The doctor that worked this booth was able to answer common questions about the COVID-19 virus, ways to prevent COVID-19 transmission, and what to do if a patient felt ill. Having this booth as a stopping point for all patients aided in combating misinformation. The registration and waiting area also aided in infection mitigation, as we avoided both unnecessary contact and large queues by having registration via a drive through and by having patients wait in their vehicles [7]. The switch in Clinic B to assign two doctors to one tent also allowed family units to stay together and avoid extra contact with other clinic personnel.
The schematics for Clinic A (Figure 1) and Clinic B (Figure 2) included a layout for each clinic location, anticipated directionality of pedestrian and vehicle flow, labels for parking areas, clinic check-in, type of service, staffing needs, and the location of support services such as trash, signage, portable restrooms, power, etc. They were used to visualize the design, to set up the clinic, and to communicate the flow of people, vehicles, and services to the volunteers and patients.
The patient check-in process was as follows: Patients arrived at the site via car and registered via drive through system. They chose the medical services they desired, received a surgical mask, were screened for COVID-19 symptoms via verbal questionnaire, and had their temperature taken via a forehead scanner. Participants who screened negatively could proceed into the clinic, and those who screened positive were offered COVID-19 testing (Clinic B only) to reduce transmission. After checking in, patients waited in their cars in the parking lot to be called via cell phone when a provider was available and were told to proceed to the vital signs station to begin their clinic visit. Spanish interpreters were assigned if needed. After vitals, patients followed a dedicated pathway to the COVID-19 education booth where they waited until a physical exam station was ready. In Clinic A, large family units were split up into two different physical exam stations to maximize efficiency; this was changed in Clinic B, where two doctors were assigned to one tent to keep family units together as much as possible. Once patients were finished with the physical exam station, they followed a highlighted walkway to the medication refill and flu shot stations and then back to the parking lot. The clear pathways allowed for social distancing and optimal patient flow through the clinic.
Both clinics offered health screenings, physical exams, and medication refills. We also provided oral health preventative care, flu vaccines, insurance assistance, and COVID-19 education. Each Clinic had iPads available to provide telehealth services from a nearby community clinic, one for medical insurance registration with a social worker and the other for clinic intake appointments with an internist who would provide follow up for patients with complicated concerns. Clinic B incorporated COVID-19 testing and provided voter engagement and registration. Both clinics were well staffed with doctors from several different primary care specialties and community partner staff that worked as bilingual nurses, registration, traffic control, and Spanish interpreters. Residents were supervised by attending. Personal protective equipment included masks, gloves, and hand sanitizer for all the volunteers, with the addition of face shields for registration and medical staff. In Clinic B, the COVID-19 swab team all wore N95s, face shields, gowns, and gloves. In total, the clinic served 94 patients.
Discussion
Mobile health clinics are key resources that should be utilized to provide much needed health care during and beyond the COVID-19 pandemic. We believe that the success of the clinics in regard to safety and effectiveness came from focusing on the clinic design and fostering a partnership with a local community organization.
The flexibility of the schematics allowed us to add COVID-19 testing to Clinic B. We were able to identify a testing area that was a safe distance from other services as well as situate the necessary COVID-19 testing support services (refrigerator, trash, power, etc.) within the testing area to avoid cross-contamination with other services. The key part in the clinic design was incorporating spatial barriers to separate the testing area from the other clinic services to avoid potential contact and transmission.
We believe that it was with these physical distancing measures combined with mandatory masking that led to our success in protecting both volunteers and patients from catching COVID-19 at our clinics.
Challenges and limitations in our clinic design
At both of our sites, all the patients came via car and had cell phones available to receive calls. While we had added a space in the schematic for patient queues, our set up assumed that foot or bicycle traffic would be minimal. Using a number system for patient check-in regardless of arrival method would also allow for different forms of transportation such as pedestrian, bicycle, or public transport. Giving an estimated time to check back to registration could cause a crowd.
Patient flow and maintaining a queue was more challenging when patients needed multiple services. For example, if a patient signed up for a flu shot and a physical exam, the flu shot station was more readily available and quicker than the physical exam stations, so they received the flu shot first. This resulted in the patient waiting in the middle of the clinic for a physical exam, even though there were others ahead of them in the queue. One solution would be to create a Part A and a Part B of the clinic.
Part A has all the ancillary services available to the patient, from flu shots to preventative dental care to insurance registration, whereas part B would be exclusively provider stations. Patients would be able to take advantage of services in Part A while they wait for their appointment in Part B. When a provider is available, a registrar at the check-in desk separating Part A and B would call out the patient’s name or de-identified number. For the registration at the drive through check-in and the personnel at the check-in desk between Part A and Part B to communicate, they could each utilize a tablet to have the most recent list as well as which physician the patient would need (i.e., paediatrician, internist, or family medicine/Med-Peds). We were able to have both clinics outdoors due to favourable weather, but indoor back up plans would be wise and would need to incorporate different mitigation strategies. We were prepared for light rain with pop-up tents, but severe weather would have been a major barrier.
Community partnership
Community engagement should begin with the community itself [8]. Partnering with established, trusted community based organizations (CBO) or faith based organizations (FBO) is particularly important to increase access within BIPOC communities, especially as some communities may have distrust due to a history of systemic and structural racism within medicine. These interventions for underserved communities have been shown to be effective in terms of health behaviors, health consequences, participant self-efficacy, and perceived social support [8]. We believe that working with and involving a local organization that was already active in the migrant farmworker community from start to finish was what led to the success of both clinics.
The trusted community organization allowed us not only to better define and understand the needs of the community, but it also enabled us to deliver care in the most helpful manner.
The nature of interactions between community members and participants influences the accessibility of health program. As a mobile clinic, accessibility was one of our main priorities, as we knew that the clinic would only be as successful as it was reachable [8]. Working with a community partner allowed for a better idea of where and when to engage the community as well as what space would be seen as recognizable and safe. For Clinics A and B, we were able to operate out of the community organizations’ parking lots familiar spaces for patients and trusted childcare centers for many of their children.
Collaborating across sectors in this case, between a university system and a rural community organization allows for pooling of local community knowledge and resources with external partners' contributions of financial and technical support to achieve common goals. CBO staff and volunteers significantly aided in our success, as they not only provided cultural knowledge and helped remove language barriers but were also a recognized trusted source of help in patients’ eyes [9]. This existing relationship between the migrant farmworker population and the community staff/volunteers helped to create a safe space for patients and provided an opportunity to establish trust between the University mobile health team and the migrant community.
Acknowledging power dynamics was another important component we considered when partnering with a local community organization and a marginalized, underserved population. It can be a difficult shift to move from a physician oriented office space to a brand new environment with no appointment schedule. We recognized that we were a group of health professionals from a university system interacting with a small community organization in a rural town and made sure to understand that our role was one of effectively supporting our community partner and following their guidance throughout our collaboration [10]. This power dynamic was communicated to our volunteers prior to the event, and they were encouraged to approach the experience with flexibility, empathy, humility, and grace.
Conclusion
Mobile clinics can be done safely and effectively during the pandemic if organizers take care to focus on mitigating infection through clinic design and fostering relationships with local community organizations. Per Yu et al, “by entering communities to connect individuals to healthcare, Mobile health clinics are serving as a stepping stone between their target community and the larger healthcare system.” This bridging has the potential to be particularly impactful by forming partnerships between university programs and CBOs to leverage the economic benefits from the university and the existing relationships to community members. Mobile health settings also offer a great opportunity to begin or expand upon telehealth services as well as incorporate useful ancillary services outside of what we often consider healthcare services insurance enrolment, voter registration, food assistance, legal services, etc. Incorporating these services allows us to provide a more holistic approach to health and work to address some of the social determinants of health that significantly impact people’s health outcomes and their ability to access healthcare services. As we slowly move from high COVID-19 infection rates to high vaccination rates, this mobile clinic model can also be used for testing and vaccine distribution as well as be a ready model for future periods marked by high levels of respiratory infection risk.
Authors' Contributions
All authors made substantial contributions to the design, writing and editing of this manuscript.
Acknowledgement
We would like to thank our community-based organization partners, Tri-Valley Opportunity Council, Community Health Services, Inc., UNIDOS, COPAL, Centro Campesino, Shelly Goddard (Tri-Valley Opportunity Council) as well as Anne Marie Weber-Main, PhD, for her help with article editing and Bobbi Daniels, MD, for her incredible support.
Funding
Otto Bremer Trust, Lynne and Andrew Redleaf Foundation, and the Office of Academic Clinical Affairs at the University of Minnesota.
Conflict of Interest
None to declare
Ethics Approval
N/A
Consent to Participate
N/A
Consent for Publication
N/A
Availability of Data and Material (Data Transparency)
Yes
Code Availability
N/A
References
- Alcendor DJ (2020) Racial disparities-associated COVID-19 mortality among minority populations in the US. J Clin Med. 9(8):2442.
- Webb HM, Nápoles AM, Pérez-Stable EJ (2020) COVID-19 and racial/ethnic disparities. J Am Med Assoc. 323:2466.
- Yu SWY, Hill C, Ricks ML, Bennet J, Oriol NE (2017) The scope and impact of mobile health clinics in the United States: A literature review. Int J Equity Health. 16.
- Driving change in health care delivery j mobile health map (2021) Mobilehealthmap.org.
- Matrajt L, Leung T (2020) Evaluating the effectiveness of social distancing interventions to delay or flatten the epidemic curve of coronavirus disease. Emerg Infect Dis. 26:1740-1748.
- Mian A, Khan S (2020) Coronavirus: The spread of misinformation. BMC Medicine. 18:89.
- Attipoe Dorcoo S, Delgado R, Gupta A, Bennet J, Oriol NE, et al. (2020) Mobile health clinic model in the COVID-19 pandemic: Lessons learned and opportunities for policy changes and innovation. Int J Equity Health. BioMed Central Ltd. 19:73.
- O’Mara-Eves A, Brunton G, McDaid D, Oliver S, Kavanagh J, et al. (2013) Community engagement to reduce inequalities in health: A systematic review, meta-analysis and economic analysis. Public Health Res, 1(4), 1-526.
- Anderson LM, Adeney KL, Shinn C, Safranek S, Buckner-Brown J, et al. (2015) Community coalition- driven interventions to reduce health disparities among racial and ethnic minority populations. Cochrane Database Sys Rev. CD009905.
- Connor A, Rainer LP, Simcox JB, Thomisee K (2007) Increasing the delivery of health care services to migrant farm worker families through a community partnership model. Public Health Nurs. 24(4):355-360.
Citation: Sharma H, Kindell E, Hane J, Kirsch JD (2022) A Medical-Design Collaboration in the Age of COVID-19: Mobile Health for Rural Populations. J Community Med Health Educ 12:778.
Copyright: © 2022 Sharma H, et al. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.
Share This Article
Recommended Journals
Open Access Journals
Article Usage
- Total views: 1684
- [From(publication date): 0-2022 - Apr 05, 2025]
- Breakdown by view type
- HTML page views: 1341
- PDF downloads: 343