Case Report Open Access
A Judicious Treatment Approach for the Management of Localized Aggressive Periodontitis: A Case Report
Nanditha S1*, Senthilkumar Muthusamy1, Balamanikandasrinivasan Chandrasekaran2 and Sathya Kannan2
1Academic unit of Adult Dental Health, AIMST Dental Centre; AIMST University, Malaysia
2Academic unit of Craniofacial Clinical Care, AIMST Dental Centre; AIMST University, Malaysia
- Corresponding Author:
- Dr. Nanditha S
MDS, AIMST Dental Centre; AIMST University
Bedong, Kedah, Malaysia
Tel: 0060164640380
E-mail: nandu98402@gmail
Received Date: March 03, 2015; Accepted Date: April 13, 2015; Published Date: April 17, 2015
Citation: Nanditha S, Muthusamy S, Chandrasekaran S, Kannan S (2015) A Judicious Treatment Approach for the Management of Localized Aggressive Periodontitis: A Case Report. J Interdiscipl Med Dent Sci 3:174. doi: 10.4172/2376-032X.1000174
Copyright: © 2015 Nanditha , et al. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.
Visit for more related articles at JBR Journal of Interdisciplinary Medicine and Dental Science
Abstract
Background: To introduce a judicious treatment modality for Localized Aggressive Periodontitis (LAP) using bone graft with platelet rich fibrin (PRF) for satisfactorily regenerating bone in defect sites.
Methods: Preoperative probing pocket depths ranging from 6-8.5 mm were present in relation to the teeth 31 and 46.Clinical attachment levels were recorded to be of same values as pocket depths. Vertical bone defects were found in periapical radiographs of teeth 46 and 31. Management of tooth 46 was done with conventional regenerative techniques but in relation to tooth 31 a customized approach was used due to limited availability for regeneration. Platelet rich fibrin with bone graft was used to regenerate the combined bone defect.
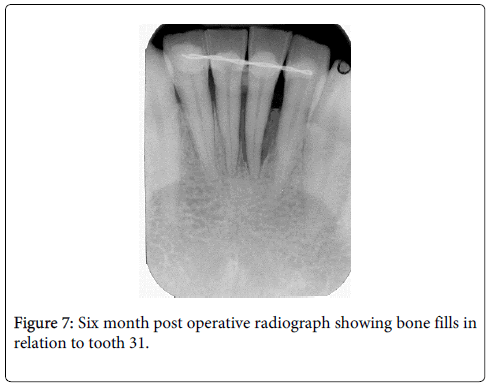
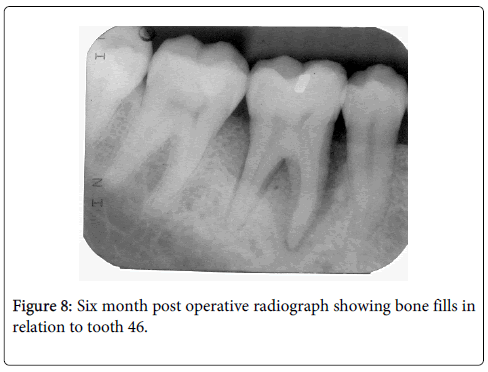
Results: Soft tissue healing showed significant improvement in probing pocket depths and clinical attachment levels. (4-4.5 mm) Satisfactory bone fill of 9 mm and 6 mm were achieved in both the sites 31 and 46 respectively at the end of six months which were measured using IOPA grid system.
Conclusion: A patient with localized aggressive periodontitis was treated successfully by addressing the key factors such as early diagnosis, elimination of periodontal pathogens and regeneration of the defect sites were accomplished using combination of bone grafts and PRF.
Keywords
Aggressive periodontitis; Blood platelets; Bone grafting; Fibrin; Guided tissue regeneration; Regeneration
Introduction
Human teeth have pivotal role in terms of speech, mastication and in maintenance of esthetic profile of an individual’s face. The salubrious nature of dentition is directly proportional to the wellbeing of structures within and enclosing them. However among these, periodontal tissues play a more pivotal role for retention of teeth. Apart from negligence of oral hygiene, the influence of genetic, anatomical and microbial factors can affect the supporting structures either independently or due to their interaction. Among various conditions affecting the periodontium, aggressive periodontitis (AP) is unique as this form is associated with potential periodontal pathogens exhibiting distinct clinical features such as rapid attachment loss, bone destruction not proportional to local factors and familial aggregation [1-3]. Due to the aggressive nature of this disease, treatment warrants beyond that of chronic periodontitis. When diagnosed early, these can be treated conservatively with OHI and systemic antibiotic therapy. With more advanced cases, treatment comprises of a more comprehensive approach including debridement, local and systemic antibiotics, and regenerative therapy. The responsiveness of aggressive periodontitis to conventional periodontal treatment is however unpredictable and the overall prognosis for these patients are poorer than for patients with chronic periodontitis [4]. In this report we present a novel technique for management of a case of localized aggressive periodontitis (LAP).
Case History
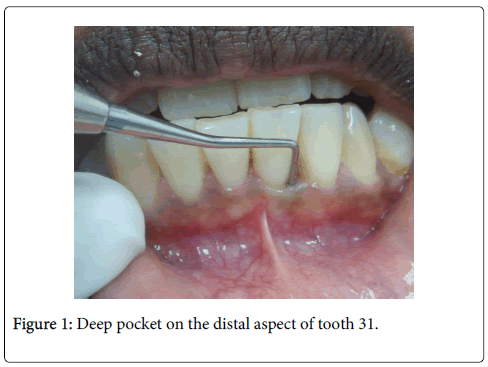
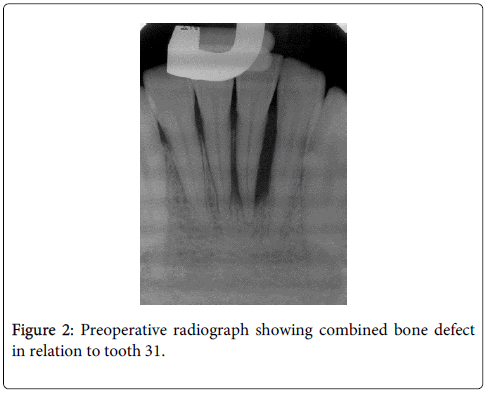
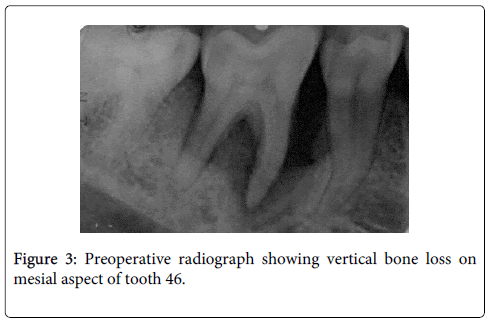
A 21 year old male, reported to AIMST dental centre with complaints of shaky lower front and right back teeth. A six point pocket depth measurement was recorded using Williams periodontal probe for both these teeth which ranged between 6-8.5mm with the disto buccal aspect of 31 measuring the deepest (Figure 1). Clinical attachment levels were recorded to be of same values as pocket depths as the gingival margins corresponded to the cemento-enamel junction. Both teeth 31and 46 had grade I mobility. His oral hygiene was good and rest of dentition seemed healthy. Radiographic examination showed extensive vertical bone loss extending to apical one third on the distal aspect of tooth 31 (Figure 2) and vertical bone loss on mesial of tooth 46 (Figure 3). Both teeth 31 and 46 were found to be vital. A clinical diagnosis of localized aggressive periodontitis was made. The patient was started on antibiotic therapy (amoxicillin and metronidazole) for seven days. Empirical therapy was used in this case over targeted selection of antibiotics as the regimen offers no greater advantage as per literature evidence [3]. Also further microbiological analysis was not performed as it was considered not necessary and cost ineffective. Flap surgery with bone grafting was planned for both the affected sites after informed consent.
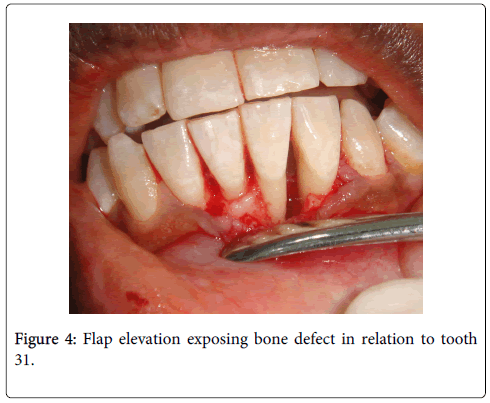
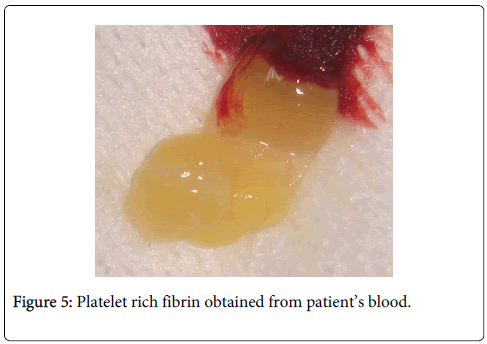
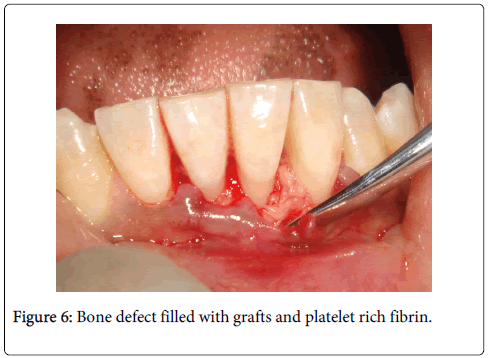
Under local anesthesia full thickness flaps were raised in relation to 31 (Figure 4) and 46. A three walled and a two walled bone defect were seen in relation to mesial aspects of teeth 46 and 31 respectively. The bone defect in tooth 46 was filled with Puros® (Zimmer Dental, USA) allograft and GTR (Biomend)® (Zimmer Dental, USA) membrane. Management of tooth 31 was bespoked by incorporating platelet rich fibrin (PRF) obtained by centrifuging 5ml of patient’s own blood at 2700rpm for 13 minutes with Puros allograft (Figures 5 and 6) [4]. Flaps were approximated using interrupted black silk (4-0) sutures. Periodical follow ups were done at regular intervals for six months during which adequate bone fill was confirmed through radiographic and clinical parameters in both sites (Figures 7 and 8). Soft tissue healing showed significant improvement in probing pocket depths and clinical attachment levels (4-4.5 mm). Periapical radiograph of teeth 31 and 46 regions were superimposed on a non-metallic grid of 1x1 mm2 calibrations and the following parameters were measured (Table 1):
| Radiographic assessment of Bone defect | Tooth 31 | Tooth 46 |
|---|---|---|
| Pre-operative bone defect [measured as the distance from cemento enamel junction (CEJ) to the base of intra bony defect (IBD).] | 16 mm | 9 mm |
| Post operative bone fill [measured by subtracting the preoperative bone defect from the distance between CEJ to the crest of new bone level.] | 9 mm | 6 mm |
Table 1: Radiographic assessment.
Discussion
The term “aggressive periodontitis” refers to a multifactorial, severe and rapidly progressive form of periodontitis [3]. Two forms exist- generalized and localized, among which the localized form typically affects the incisors and first molars. Treatment methods for aggressive periodontitis are often similar to those used in chronic periodontitis. These include: Oral hygiene instructions, reinforcement and evaluation of the patient’s plaque control, supragingival and subgingival scaling and root planning, control of other local factors, occlusal therapy, if necessary, periodontal surgery, if necessary, periodontal maintenance [5,6].
Several studies in the 80’s and early 90’s have demonstrated that treatment revolving solely around mechanical debridement either in the form of “closed” debridement or access flap technique did not produce satisfactory results leading to progressive attachment loss [7-11]. This was later attributed to the fact that pathogens associated with LAP such as Aggregatibacter actinomycetemcomitans (A.A) can penetrate tissues and therefore never completely eliminated by mechanical therapy alone [12]. Hence synergistic use of suitable antibiotics selected based on the predominant pathogen, is used as an adjunct to mechanical therapy [2,13,14].
However studies conducted to evaluate the effectiveness of microbial testing concluded that the usefulness of microbial testing may be limited and that empirical use of antibiotics, such as a combination of amoxicillin and metronidazole, may be more clinically sound and cost effective than bacterial identification and antibiotic-sensitivity testing [15]. Hence in this case we used the same combination with successful results. Certain cases however might require in addition to basic periodontal management, placement of bone grafts and GTR membranes, hemisection, bicuspidisation etc to salvage the affected tooth. Finally success of any treatment relies on maintenance care and individual tailor made maintenance programs are designed based on risk factors of the patients such as smoking, genetic factors and systemic diseases for successful management of Aggressive Periodontitis patients [16].
In our patient typical clinical features of LAP were seen in relation to tooth 46 and 31. As tooth 46 exhibited vertical bone loss, conventional approach was used for its management. The presence of combined bone defect in relation to tooth 31 necessitated transmogrification of the conventional approach.
Regeneration of combined bone defects in the anterior teeth region is seldom attempted due to the limited availability of area for regeneration. However this impediment has been surmounted in recent years with the availability of newer regenerative biomaterials such as PRF which can serve as a resorbable membrane [17]. Growth factors released after activation from the platelets gets trapped within fibrin matrix which has been shown to stimulate the mitogenic response in the periosteum for bone repair during wound healing [18]. In comparison to conventional regenerative techniques PRF provides synergistic effect with graft materials and enhances angiogenesis. Concentrated platelets can accelerate tissue regeneration and enhance the quality and quantity of newly formed tissues by functioning as an ideal reservoir for autologous growth factors [19].
Our approach in management of this case was a successful as the treatment addressed important key factors such as early diagnosis, elimination of periodontal pathogens and aimed at stability of the affected site through the employed regenerative technique. A literature search (PubMed) disclosed no reported studies on the usage of PRF with bone grafts in the treatment of LAP. Although PRF has been tested and found effective in combination with bone grafts it has never been used in treating combined bone defects in lower anterior teeth which makes this treatment approach relatively innovative.
References
- Satyanarayana KV, Anuradha BR, Srikanth G, Chandra Mohan P, Anupama T, et al. (2012) Clinical Evaluation of Intrabony Defects in Localized Aggressive Periodontitis Patients with and without Bioglass- An in-vivo Study. Kathmandu Univ Med J 37:11-15.
- Mambelli AW, Van winkelhoff AJ (1997) The systemic use of antibiotics in periodontal therapy. In: Lang N.P, Karring T, Lindhe J: Proceedings of the 2nd European workshop on periodontology. Quintessenz, Berlin 38-77.
- Armitage GC (1999) Development of a classification system for periodontal diseases and conditions. Ann Periodontol 4:1-6.
- Prakasam A, Elavarasu SS, Natarajan RK (2012) Antibiotics in the management of aggressive periodontitis. Journal of Pharmacy & Bioallied Sciences 4: 252-255.
- Noack B, Hoffmann T (2004) Aggressive periodontitis. PERIO-Periodont Prac Today 1: 335-344.
- American Academy of Peridontology (2000) Parameter on aggressive periodontitis. J Periodontol 71: 867-869.
- Christersson LA, Slots J, Rosling BG, Genco RJ (1985) Microbiological and clinical effects of surgical treatment of localized juvenile periodontitis. J Clin Periodontol 12: 465-476.
- Gunsolley JC, Zambon JJ, Mellott CA, Brooks CN, Kaugars CC (1994) Periodontal therapy in young adults with severe generalized periodontitis. J Periodontol 65: 268-273.
- Komman KS, Robertson PB (1985) Clinical and microbiological evaluation of therapy for juvenile periodontitis. J Periodontol 56:443-446.
- Mombelli A, Gmur R,Gobbi C, Lang NP (1994) Actinobacillus actinomycetemcomitans in adult periodontitis. II. Characterization of isolated strains and effect of mechanical periodontal treatment. J Periodontol 65: 827-834.
- Slots J, Rosling BG (1983) Suppression of periodontopathic microflora in localized juvenile periodontitis by systemic tetracycline. J Clin Periodontol 10: 465-486.
- Christersson LA, Albini B, Zambon JJ, Wikesjo UM, Genco RJ (1987) Tissue localization of Actinobacillus actinomycetemcomitans in human periodontitis. I. Light immunofluorescence and electron microscopic studies. J Periodontol 58: 529-539.
- Kamma JJ, Baehni PC (2003) Five year maintenance follow up of early-onset periodontitis patients. J Clin Periodontol 30:562-572.
- Mombelli A, Schmid B, Rutar A, Lang NP (2000) Persistance patterns of Porphyromonos gingivalis, Prevotella intermedia/nigrescens and Actinobacillus actinomycetemcomitans after mechanical therapy of periodontal disease. J Periodontol 71:14-21.
- Haffajee AD, Socransky SS, Gunsolley JC (2003) Systemic anti-infective periodontal therapy A systematic review. Annals of Periodontol 8:115.
- Lang NP, Tonetti M (1996) Periodontol diagnosis in treated periodontitis Why, when and how to use clinical parameters. J Clin Periodontol 23: 240-250.
- Dohan DM, Choukroun J, Diss A, Dohan SL, Dohan AJ, et al. (2006) Platelet rich fibrin: a second-generation platelet concentrate: Part I. Technological concepts and evolution. Oral Surg Oral Med Oral Path Oral Radiol Endod 101: 37-44.
- Gupta V, Vivek K Bains, Singh GP, Mathur A, Bains R (2011) Regenerative Potential of Platelet Rich Fibrin in Dentistry: Literature Review. Asian J Oral Health Allied Sci 1:22-8.
- Pluemsakunthai W, Kuroda S, Shimokawa H, Kasugai S (2013) A basic analysis of platelet rich fibrin: distribution and release of platelet-derived growth factor-BB. Inflamm Regen 33: 164-172.
Relevant Topics
- Cementogenesis
- Coronal Fractures
- Dental Debonding
- Dental Fear
- Dental Implant
- Dental Malocclusion
- Dental Pulp Capping
- Dental Radiography
- Dental Science
- Dental Surgery
- Dental Trauma
- Dentistry
- Emergency Dental Care
- Forensic Dentistry
- Laser Dentistry
- Leukoplakia
- Occlusion
- Oral Cancer
- Oral Precancer
- Osseointegration
- Pulpotomy
- Tooth Replantation
Recommended Journals
Article Tools
Article Usage
- Total views: 16220
- [From(publication date):
April-2015 - Jul 18, 2025] - Breakdown by view type
- HTML page views : 11460
- PDF downloads : 4760