Case Report Open Access
A Focal Liver Lesion in a Patient with Chronic Hepatitis B and Cirrhosis not always Hepatocellular Carcinoma
Samuel Raimundo Fernandes1*, Joana Rita Carvalho1, Luis Araujo Correia1, Artur Silva2, Cilenia Baldaia1, Helena Cortez-Pinto1 and Jose Velosa1
1Gastroenterology and Hepatology Service, Hospital Santa Maria, Lisbon Hospital Centro North, Portugal
2Pathological Anatomy Service, Hospital Santa Maria, Lisbon Hospital Centro North, Portugal
- Corresponding Author:
- Samuel Raimundo Fernandes
MD, Gastroenterology and Hepatology Service
Hospital Santa Maria, Lisbon Hospital Center North, Portugal
Tel: 351968644836
E-mail: Samuelrmfernandes@gmail.com
Received Date: March 08, 2016; Accepted Date: March 21, 2016; Published Date: March 28, 2016
Citation: Fernandes SR, Carvalho JR, Correia LA, Silva A, Baldaia C, et al. (2016) A Focal Liver Lesion in a Patient with Chronic Hepatitis B and Cirrhosis not always Hepatocellular Carcinoma. J Gastrointest Dig Syst 6:403. doi:10.4172/2161-069X.1000403
Copyright: © 2016 Fernandes SR, et al. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.
Visit for more related articles at Journal of Gastrointestinal & Digestive System
Abstract
Chronic liver disease and cirrhosis are known risk factors for hepatocellular carcinoma (HCC). We present a 68- year old male patient with chronic hepatitis B infection and cirrhosis admitted for investigation of a 10-cm solid liver nodule detected during surveillance ultrasound. Abdominal computed tomography (CT) revealed an additional 3 cm lesion in the right liver lobe and multiple lesions in the spleen without typical features of HCC. Histopathologic examination of the liver nodule biopsy was compatible with metastasis from a neuroendocrine tumor. The patient was referred for chemotherapy but unfortunately died 2 months later from infectious complications. The present case seemed unusual considering that the background chronic liver disease would make HCC a more likely diagnosis. The multiple comorbidities presented by our patient provided an additional challenge by broadening the differential diagnosis.
Keywords
Cirrhosis; Chronic hepatitis B; Focal liver lesion
Introduction
Hepatocellular carcinoma (HCC) is a major health concern worldwide, representing one of the leading causes of cancer relatedmortality. More than 80 % of the cases of HCC occur in the setting of cirrhosis [1]. Chronic hepatitis B virus (HBV) infection is the most important etiologic factor, accounting for half of all cases, and reaching 78% in areas of high HCC incidence [2]. According to current international guidelines, patients with advanced liver disease and cirrhosis should undergo routine ultrasound surveillance every six months in order to screen for HCC. Patients with cirrhosis who present with a solid focal lesion are at a very high risk for HCC and must be considered to have HCC until proven otherwise [1]. We report a patient with chronic hepatitis B and cirrhosis with a large liver nodule whose final diagnosis based on histopathology was a neuroendocrine tumor metastasis. The present case seemed of great interest considering the uncommon diagnosis in a patient with liver cirrhosis. We present the current case, highlight clinical and pathophysiologic findings and review the available literature.
Case Report
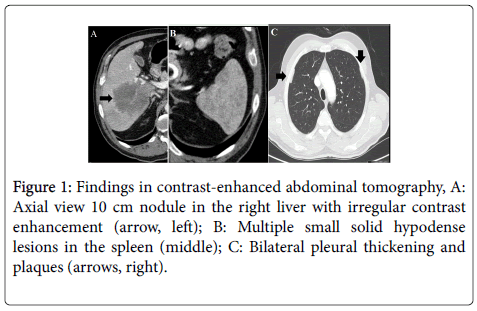
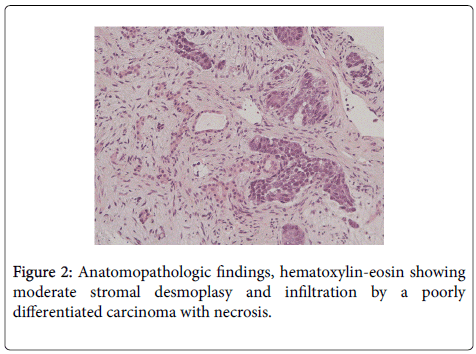
A 68 year old male patient was admitted to our gastroenterology clinic for investigation of a focal liver nodule. The patient’s medical history was relevant for chronic hepatitis B, diagnosed 20 years earlier. Three years before, due to persistent elevation in aminotransferase levels and transient elastography showing advanced fibrosis, the patient was started on entecavir with sustained virologic response. One year ago, while maintaining undetectable viral load, the patient developed esophageal varices and splenomegaly and was diagnosed with liver cirrhosis. Four-months before admission, despite adherence to entecavir, there was an unexpected rise in hepatitis B viral load and so it was changed to tenofovir. One month prior to admission, the patient started complaining of worsening epigastric pain and progressive weight loss. Unexpectedly, abdominal ultrasound revealed portal vein thrombosis and a 10 cm solid nodule in the right liver lobe, not present in his previous examination. The patient was admitted for further investigation. The physical examination was relevant for mild upper abdominal tenderness on palpation. Laboratory tests showed anemia, elevated inflammatory markers and a mild cholestastic pattern. Alpha-fetoprotein was normal (Table 1). A percutaneous biopsy of the liver nodule was performed. While waiting for anatomopathologic results, a staging CT was performed. Unexpectedly, CT revealed an additional 3 cm lesion in the right liver lobe and multiple hypodense lesions in the spleen. These lesions showed irregular arterial enhancement and no late washout, untypical of HCC (Figures 1A and 1B). In addition, CT identified bilateral pleural thickening and multiple pleural plaques in accordance with a previous exposure to asbestos (Figure 1C). Our patient presented with a newonset solid liver nodule. Considering the coexistence of liver cirrhosis, hepatocellular carcinoma should be the first hypothesis. Other differentials should include other malignancies such as cholangiocarcinoma and metastasis from other organs. The previous exposure to asbestos could suggest a diagnosis of mesothelioma. Histopathologic examination of the liver nodule biopsy revealed infiltration by a low differentiated carcinoma with moderate stromal desmoplasy (Figure 2). Proliferation ratio was estimated at 70%. Immunochemistry was positive for cytokeratin (CK) 8/18, CK19, epithelial membrane antigen, vimentin, synaptophysin, CD10, CD56, and CDX2. There was no staining for CK5/6, CK7, CK20, CK903, S100p, anti-polyclonal carcinoembryonic antigen, hepatocyte paraffin 1 monoclonal antibody, chromogranin A, inibine, Wilms tumour-1, calretinine, thyroid transcription factor-1, racemase and prostate specific antigen (Figure 3). This pattern was highly suggestive of a metastasis from a neuroendocrine tumor. Subsequently, plasma levels of neuronal specific enolase were confirmed to be markedly elevated (178.1 μg/L, normal range <16.3 μg/L). The patient underwent extensive workup including upper and lower gastrointestinal endoscopy, thyroid ultrasound and bronchofibroscopy. Unfortunately, these exams did not provide further clues on the primary location of the tumor. The patient was started on systemic chemotherapy with etoposide and carboplatin. Two months later, the patient was admitted with fever and jaundice. CT confirmed biliary duct compression by multiple liver metastasis. An endoscopic cholangiopancreatography was performed and a biliary stent was left in place, providing shortterm relief of the obstruction. Unfortunately, the patient died in a subsequent admission with a severe systemic infection.
| Item | Patient levels | Reference levels |
|---|---|---|
| Hemoglobin (g/dL) | 11.5 | 12.0-16.0 |
| Leukocytes (x 109/L) | 16.3 | 4.0-10.0 |
| Platelets (x 109/L) | 267 | 150-400 |
| Prothrombin time (sec) | 13.1 | 11.6 |
| CRP (mg/dl) | 2.7 | <0.8 |
| Albumin (mg/dl) | 4.1 | 3.2-4.8 |
| ALT (U/L) | 60.8 | Dec-78 |
| AST (U/L) | 44 | <34 |
| GGT (U/L) | 356 | <73 |
| LDH (U/L) | 475 | 208-378 |
| Total bilirubin (mg/dL) | 0.9 | < 1 |
| Alpha-fetoprotein (µg/ml) | 6.7 | <8.1 |
| Quantitative hepatitis B surface antigen | 2480 | <0.05 |
| HBV DNA (log) | 3.99 | - |
| Anti-HBcIgM | - | - |
Table 1: Laboratory evaluation at admission to our institution. There is mild anemia, raised inflammatory markers and a mild cholestastic pattern. The hepatitis B viral load is positive.
Discussion
Neuroendocrine tumors are rare neoplasms that arise from cells of the neuroendocrine system. Although estimates vary, the annual incidence of neuroendocrine tumors is approximately 2.5-5 per 100.000 [2]. Coexistence of chronic hepatitis B and various types of neuroendocrine tumors has seldom been reported [3,4]. Nevertheless, a recent study evaluating the prevalence of various human viruses in patients with neuroendocrine tumors found no association with hepatitis B virus [5]. We could not find an association between nucleotide analogue reverse transcriptase inhibitors and increased incidence of neuroendocrine tumors. It is unknown if chronic liver disease and cirrhosis increases the risk for neuroendocrine tumors. There have been reports on coexistence of liver cirrhosis and neuroendocrine tumors [6,7] A recent study reported elevated serum levels of chromogranin A in over one third of patients with hepatocellular carcinoma. The author hypothesizes that some hepatocellular carcinomas could acquire a neuroendocrine differentiation [8]. This is in accordance with some reports on coexistence of HCC and neuroendocrine tumors [7]. Curiously, the author reports an unusual and aggressive combination of hepatocellular-cholangiocarcinoma and neuroendocrine carcinoma. Our patient also presented pulmonary disease related to chronic exposure to asbestos. Some authors have suggest that asbestos exposure could increase the risk for neuroendocrine tumors [9]. Bénédicte showed that cumulative exposure to asbestos was higher in patients with pulmonary carcinoid tumors versus lung cancer controls (3.5 ± 4.5 versus 0.3 ± 0.5, p<0.04). These findings, however, have not been confirmed by other authors [10]. This case highlights an unexpected finding in a patient with hepatitis B associated liver cirrhosis. The multiple comorbidities presented by our patient provided an additional challenge by broadening the final diagnosis. It is still to ascertain the importance of viral breakthrough on the occurrence of neuroendocrine tumor. The important message clinicians should be aware is that not all focal liver lesions in patients with cirrhosis should be attributed to hepatocellular carcinoma. In the presence of atypical findings every attempt to exclude other causes should be undertaken.
References
- Dufour JF, Greten TF, Raymond E, Roskams T, De T, et al. (2012) Clinical Practice Guidelines EASL – EORTC Clinical Practice Guidelines: Management of hepatocellular carcinoma European Organisation for Research and Treatment of Cancer. J Hepatol 56: 908-943.
- Siegel R, Naishadham D, Jemal A (2013) Cancer statistics, 2013. CA Cancer J Clin 63: 11-30.
- Fiorino S, de Biase D, Fornelli A, Masetti M, Cuppini A, et al. (2015) Hepatitis B Virus Infection and Pancreatic Neuroendocrine Tumor. Pancreas 44: 341.
- Lin CW, Lai CH, Hsu CC, Hsu CT, Hsieh PM, et al. (2009) Primary hepatic carcinoid tumor: a case report and review of the literature. Cases J 2: 90.
- Schmitt M, Hofler D, Koleganova N, Pawlita M (2011) Human polyomaviruses and other human viruses in neuroendocrine tumors. Cancer Epidemiol Biomarkers Prev 20: 1558-1561.
- Shelat VG, Diddapur RK (2008) Duodenal carcinoid: a rare cause of melaena in a cirrhotic patient. Singapore Med J 49: e198-201.
- Ishida M, Seki K, Tatsuzawa A, Katayama K, Hirose K, et al. (2003) Primary hepatic neuroendocrine carcinoma coexisting with hepatocellular carcinoma in hepatitis C liver cirrhosis: report of a case. SurgToday 33: 214-218.
- Biondi A, Malaguarnera G, Vacante M, Berretta M, D'Agata V, et al. (2012) Elevated serum levels of Chromogranin A in hepatocellular carcinoma. BMC Surg 12: S7.
- Clin B, Andujar P, Al Samad I, Azpitarte C, Le Pimpec-Barthes F, et al. (2012) Pulmonary carcinoid tumors and asbestos exposure. Ann Occup Hyg 56: 789-795.
- Neumann V, Fischer M, Tannapfel A (2008) Carcinoid tumours of the lung and definition of the medico-legal term "lung cancer" used in the list of occupational disease in Germany--results of the German Mesothelioma Register. Pneumologie 62: 569-573.
Relevant Topics
- Constipation
- Digestive Enzymes
- Endoscopy
- Epigastric Pain
- Gall Bladder
- Gastric Cancer
- Gastrointestinal Bleeding
- Gastrointestinal Hormones
- Gastrointestinal Infections
- Gastrointestinal Inflammation
- Gastrointestinal Pathology
- Gastrointestinal Pharmacology
- Gastrointestinal Radiology
- Gastrointestinal Surgery
- Gastrointestinal Tuberculosis
- GIST Sarcoma
- Intestinal Blockage
- Pancreas
- Salivary Glands
- Stomach Bloating
- Stomach Cramps
- Stomach Disorders
- Stomach Ulcer
Recommended Journals
Article Tools
Article Usage
- Total views: 13432
- [From(publication date):
April-2016 - Nov 21, 2024] - Breakdown by view type
- HTML page views : 12673
- PDF downloads : 759