A Discursive Examination of the Neurodegenerative Alzheimer's Disease
Received: 01-Dec-2022 / Manuscript No. cpb-22-83777 / Editor assigned: 05-Dec-2022 / PreQC No. cpb-22-83777 / Reviewed: 19-Dec-2022 / QC No. cpb-22-83777 / Revised: 26-Dec-2022 / Manuscript No. cpb-22-83777 / Published Date: 30-Dec-2022 DOI: 10.4172/2167-065X.1000305
Abstract
Introduction: Alzheimer's disease is the most advanced type of dementia in the globe. Putting an increasing strain on healthcare systems. Almost 6.2 M American (age 65) and older suffering from AD .72 % are 75 year old. One out of every nine adults aged 65 and up suffers from AD (11.3 %)
Phathophysiology: Alzheimer's disease is a cross neurodegenerative illness with a wide range of symptoms. That involve in genetic changes, Education, maturity level, and atmosphere. Now AD is due to some factors like cholinergic hypothesis, beta amyloid and tau protein and neuro mediated inflammation, neurofibrillary tangles of tau.
Symptomatology: mainly over time, more than 90% of all patients experience, restless, anxiety, depression, delusions, dementia, motor abnormality, irritability, sleep problems, hunger disorders, or poor impulse control.
Diagnosis: Furthermore, magnetic resonance spectroscopy is linked to molecular diagnosis (MRS). MicroRNAs (miRNAs), which short non-coding RNAs that motivate gene expression post-transcriptionally. Though Alzheimer's disease (AD) is still a clinical diagnosis, imaging techniques such as PET amyloid and bioparameter in CSF can aid in the evaluation of many patients.
Treatment Avenue: A gene is responsible for the expression of a therapeutic enzyme or a growth factor was used as a primary approach of treatment of AD. However it can treat with medication like AchE inhibitors. Furthermore, Gene therapy and immunotherapy is also use as treatment
Conclusion: AD can be treated with a variety of criteria, including programs, bodily fluids, and imaging studies, in overall studies. AChE inhibitors, and many therapy used for treatment of AD
Introduction
AD affects around 45M people around the world, according to researches. Alzheimer's disease is the main cause of dementia, accounting for 62-82% of cases [1].
5.8 million Americans over the age of 65 are believed to be affected by AD, and that number is calculation to rise to 14.1M by the year 2050. While Ad's prevalence grows, so does the expense of caring for those who are infected with the disease. Dementia-related healthcare and hospice costs in the United States are expected to equal $305 billion by 2020 [2].
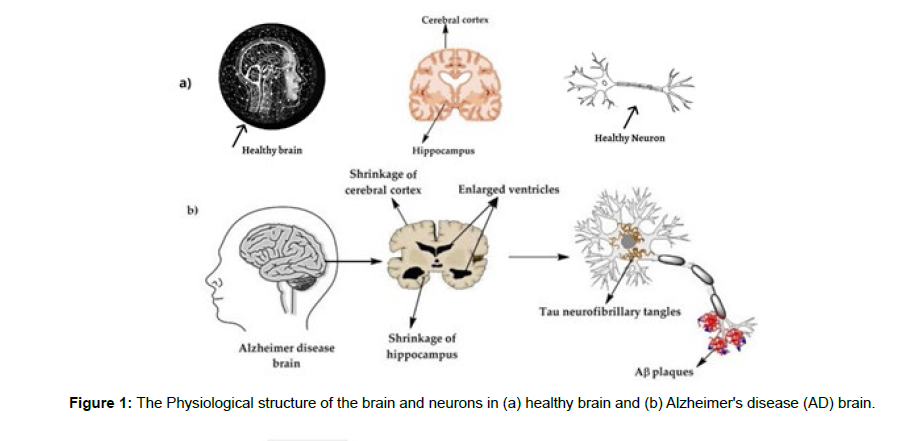
Extracellular AB plaque accumulation and intracellular neurofibrillary tangles of hyper phosphorylated tau characterize the neuropathology of Alzheimer's disease. Although biomarkers in the CSF and positron emission tomography (PET) can improve prefect diagnosis, AD is still a clinical diagnosis (Figure 1).
Intoxications, infections and abnormality in the pulmonary and circulatory systems, which produce a reduction in the oxygen supply towards the brain, nutritional deficiency, cobalamin deficiency, tumors, and other factors can all cause progressive loss of cognitive skills. [4,5] .
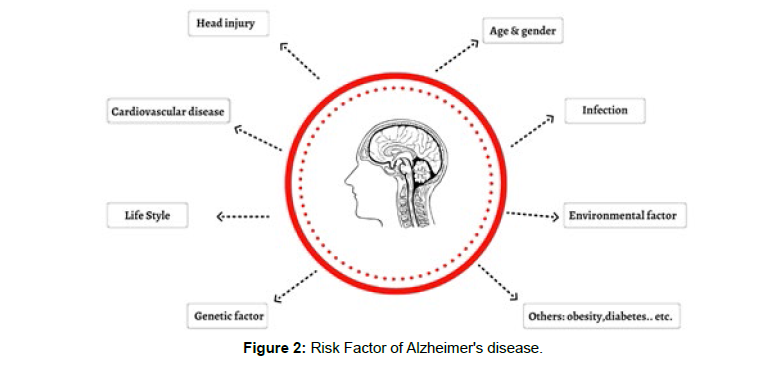
Alzheimer's is a neurologic disease that leads to the death of brain cells. AD is the most intimate form of dementia. A neurotransmitter plays a main role in AD. The abnormal level of Acetylcholine is mainly responsible for progression of Alzheimer’s disease (Figure 2).
Pathophysiology
Cholinergic Theorem
The cholinergic theorem, which was the initial thought connected to AD etiology, is one of the most researched processes related to the starting and progress of AD [5].
In general, AD carriers' brains show shrinkage, synaptic loss, and a lack of central neurotransmission, in addition to the previously mentioned histological indicators. Neurons in the forebrain are degenerating in general [6]. In the early stages of Alzheimer's disease, cholinergic neurons in the basal nucleus and cortex die. By the end of the disease, more than 91% of the cholinergic neuron in the basal nucleus has died.
Inflammatory Mechanism of Mitochondrial Irregularity
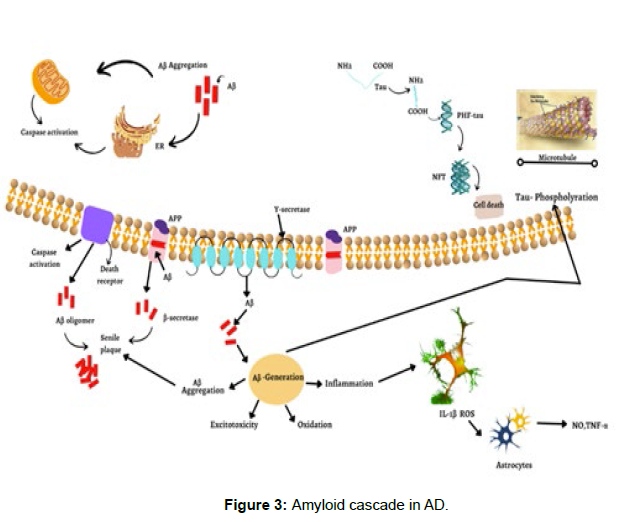
Alzheimer's disease is closely linked to inflammatory responses. Additionally, various investigations have found that Tau disorders are greatly exacerbated when acute and chronic inflammatory processes occur [7]. Clusters of microglia, increased levels of pro-inflammatory cytokines, and microglial activation before the formation of nfts are all signs that the brain is getting ready to get sick. (Figure 3) are all implicated in these inflammatory processes [7,8].
In terms of mitochondrial irregularity, it is thought that the accumulation of Aβ fragments and abnormal Tau protein in brain cells impact mitochondrial function, particularly mitochondrial oxidative metabolism [8,9]. Benevento's research into the existence of Abeta peptides allowed him to more valuable infers that these peptides can be directly hazardous to mitochondria of neurons [9].
Beta Amyloid and Protein Tau Hypothesis
As previously stated, Aβ fragments and nfts are significant markers for Alzheimer's disease [7], and they specify the amyloid theorem.
These deposits arise as a result of native proteins folding incorrectly, i.e., after a change in cleavage of the amyloid precursor protein [10].
Amyloid precursor protein is a 770-amino-acid membrane protein made by a wide range of cells, including neurons in the brain. [10,11]. APP is cleaved by the enzymes α-, β- and ɣ-, and -secretase, and the Amyloidosis is stimulated once APP is broken down by -secretase, which makes 39 to 43 insoluble peptides that can't be dissolved in water. This demonstrated that Aβ is not fundamentally cytotoxic and does not cause tau to accumulate when Aβ fibrils accumulate extracellularly. The assumption evolved that Aβ oligomers (multimers), which are a typical metabolic byproduct of APP and are not harmful in and of themselves under physiologically normal conditions, were the main toxic agents. Furthermore, it was noted that when an oligomers (dimers) from AD patients' brains were directly transferred to the hippocampus, dendritic spines decreased, long-term potentiation was inhibited, long-term suppression was promoted, and memory learning was impaired [10].
Symptomatology
When the signs of Alzheimer's disease (AD) grow severe, with slow and progressive degradation of the brain, it is a common reason of dementia in the elder’s. Language, personality, and cognitive control are all influenced by memory [11]. The medical and economic consequences of Alzheimer's disease are significant Dementia, dependency, and disability all has social consequences [12].
Disinterest, anxiousness, nervousness, distress, delusions, dementia, motor activity abnormality, irritation, abnormal sleep problems, eating disorders or poor impulse control affect A lot of people who have Alzheimer's disease have problems with their moods at some point during the disease's development. Depression can be discovered in 40-50% of people who have it disorders affect 10- 20% of cases. In Alzheimer's disease, depressive symptoms are particularly common.
Some common symptoms of AD:-
• Increased confusion & loss of memory
• Inability to acquire information
• Difficulties in reading, writing, and explain numbers
• Having problem about thought.
• Coping issues when confronted with unfamiliar conditions
• Multi task, such as dressed, are difficult to complete it.
• Having difficulty to identify close one.
• Hallucinations, delusions, are all symptoms of schizophrenia.
• Excessive anger
• Moodiness, discontent, nervousness, and tears.
• Repeat movements, muscular twitches on occasion
Medicines can improve or decrease the symptoms. People who suffer from AD and their caring person can benefit from a variety of occasions and services. Alzheimer's disease patients may benefit from drugs that help them maintain their freedom and optimize their functionality.
Diagnosis
It is critical to diagnose AD early on in the disease's progression to guarantee that the patient has a decent quality of life [13,14]. In a variety of fields, neuropsychological and psychometric test are perform for a patient's cognitive abilities. Blood testing, neuro-imaging, molecular and functional neuro-imaging, and other tests are also available.
Evoked potentials, cerebrospinal fluid, and electroencephalogram (EEG) are all conducted. Genetic investigations are also significant supplemental tests that can help with a more thorough diagnosis of diseases [15].
The following factors should be included in laboratory blood testing to diagnose Alzheimer's disease:
Comprehensive blood count, urea, creatinine, T4, TSH, albumin, enzymes of lever , vitamin B12, calcium, and complete HIV serology in individuals under the age of 60 [16].
Furthermore, magnetic resonance spectroscopy is linked to molecular diagnosis (MRS). MicroRNAs, that influence gene expression post-transcriptionally, have been used to diagnose Alzheimer's disease [17]. Disturbance in regulation of genes in the amyloidogenic cascade (APP, BACE1, and MAPT) is produced by modify in the miRNA metrix generated through disease [18].
Dementia can determine by EEG test. The electric impulses of cortical neurons are read by EEG, which show function of brain. Subcortical dementias, such as DLB and PDD, have aberrant EEG recording patterns. The purpose of EEG, which is also a technology, is to achieve earlier diagnosis, similar to other approaches. In repeated research in rest behavior EEG, four consequences of Alzheimer's disease have been identified [19]. In Alzheimer's disease, the power spectrum shifts from high prevalence (alpha, beta, gamma) to low prevalence (beta, gamma) [20]. The advancement of AD is related to the change from high to low frequency. EEG signal complexity is reduced in people with AD, which is most likely due to neuronal death [21]. In patients with Alzheimer's disease, there is a loss in synchronisation as a result of diminished connection between brain areas [22, 23].
Treatment Avenue
Gene Therapy
Gene therapy is a process that has a lot of attention in the Studies. The basic method was to introduce a gene that produces an enzyme or growing factor that is reparative. Its main objective is to reach brief regulation of specific genes at therapeutically useful quantities. Depending on the target ailment, the method of gene transfer and in vivo vs. ex vivo treatment differs. Gene enhancement, gene suppression, and genetic manipulation are the most common methods [24].
The most popular forms of vector use in genetic engineering are RNA or DNA viral vector. The most prevalent sources of RNA-based viral vectors are retroviruses like the Leukaemia Virus (MLV) and lentiviruses like the immunodeficiency virus (HIV). An adenovirus or an adenovirus-associated virus (AAV) is the most common DNA vectors. It is important to note that each vector has its own restrictions, and various vectors are used based upon the nature of the research and the target cell. In addition to providing neuroprotection and neuro restoration, its pathological route also allows it to effectively target the pathogenic process at the root of the problem. There are a lot of factors involved in gene therapy, including time and location specificity, gene regulation and the most prevalent impediment in treating neuro-degenerative diseases, the gene delivery process that must be considered. Amyloid Beta (Aβ) Immunotherapy Neurodegenerative diseases like Alzheimer's disease have attracted a significant lot of interest and scientific research into immunotherapy's potential anti- Aβ therapeutic benefits [25]. Preclinical and clinical testing has shown a variety of therapeutic alternatives as 2nd generation Aβ vaccines and anti-Aβ monoclonal antibodies [26]. Active immunisation is the injection of vaccinations intended to activate the body’s immune cell in response to outside antigens. To produce Aβ -specific antibodies, the active vaccination process relies on both the cellular and humoral immune systems. The fact that an active vaccination comprises an antigen means that overlapping conformational epitopes on a protein may lead to the generation of multiple antibodies. First vaccine was developed (Elan Pharmaceuticals) synthetic A in combination with QS-21, a surface-active saponin additive (AN1792). Patients with moderate to severe Alzheimer's disease experienced considerable amyloid plaque removal and cognitive improvement in the first two clinical trials. Meningoencephalitis, a potentially deadly side effect, forced the researchers to call time on the experiments in 2002 [27]. Ache Inhibitors Several ChE inhibitors have been developed. Currently, there are four drugs on the market for the therapy of AD: donepezil; galantamine; and memantine (3032). The effectiveness of these drugs is limited, but they have a wide range of dose-related side effects, particularly at higher doses [28,29]. Galantamine and donepezil are AChE inhibitors; further rivastigmine is a reversible antagonist. Donepezil is far more AChEtargeted than BChE. Inhibitory concentrations of AChE for tacrine are 77 nM, donepezil is 6.7 nM, and rivastigmine is 4.3 nM [29]. Physostigmine: Eserine, commonly known as physostigmine, is an AC hE inhibitor that was initially discovered from Calabar beans in 1864 [30,31]. Physostigmine can cross the blood-brain barrier, however its short half-life and significant side effect, it has a limited therapeutic index [32]. Diarrhea, stomach pains, increased saliva production, and excessive perspiration are all frequent adverse effects [32]. Because of these drawbacks; physostigmine was not passed for the treatment of AD. Donepezil: the medication donepezil was authorised for the treatment of delicate to Alzheimer’s disease in 1996 [33]. Donepezil, on the opposite hand, will cause temporary state, loss of appetence, diarrhea, cramps, and muscle weakness [34]. Low pressure level, severe projection, muscle weakness, extreme nausea, respiratory problem, and arrhythmia area unit common aspect effects of high dosages of donepezil [34]. Donepezil could have further modes of action additionally to inhibiting ChE [35]. ChE inhibitors of the next generation The better effectiveness of THA in improving cognitive function in Alzheimer patients cannot be explained by the fact that it inhibits cholinesterase less potently than physostigmine does in vivo. Furthermore, the information that is now available on cholinesterase inhibition following invivo therapy with THA suggests that this may not be the drug's exclusive mode of action [36]. Apparently, THA interacts with muscarinic receptors (5-15). Low doses of muscarinic agonists couldn't bind to THA. Physostigmine byproducts, like phenserine, eseroline, are manufactured as Choline esterase inhibitors. Phenserine: In vitro and in vivo, phenserine may be a selective, noncompetitive AChE substance that not solely inhibits AC hE however additionally lowers APP synthesis [36]. Moreover, phenserine's toxicity is less than that of tacrine and physostigmine [37]. Treatment with phenserine, as an example, has been tried to extend memory and learning in previous dogs and rats [36].
Eseroline: Eseroline is Associate in nursing agonist for opioids [38]. It absolutely was discovered in 1982 that eseroline may be a substance of physostigmine; but, not like alkaloid, eseroline’s impact on AC hE inhibition is restricted and reversible [39]. Physostigmine analogues are studied for his or her ability to suppress ChE [40].
Conclusion
When the NINCDS-ADRDA reclassified and up-to-date its 1984 criteria, it improved early detection of people at risk for AD besides the ability to identify those who are most likely to develop the condition. Programs, physiological fluids, and imaging examinations have all been suggested for a more accurate diagnosis of AD in the previous several years. There has been no change in the prognosis of Alzheimer's therapy despite this. Cholinesterase enzyme inhibitors include physostigmine, donepezil, and phenserine.
Alzheimer's disease medication is most effective when it is administered early and biomarkers are used to track the illness's course. Alzheimer's disease pathology may be slowed by the use of combination treatment and future tau pathology medicines.
References
- Crous-Bou M, Minguillón C, Gramunt N, Molinuevo JL (2017) Alzheimer’s disease prevention: from risk factors to early intervention. Alzheimers Res Ther.
- Alzheimer’s A (2020) Alzheimer’s disease facts and figures. Alzheimer’s & Dement 16: 391-460.
- Terry RD, Davies P (1980) Dementia of the Alzheimer type. Annu Rev Neurosci 3: 77-95.
- Rathmann KL, Conner CS (1984) Alzheimer's disease: clinical features, pathogenesis, and treatment. Drug Intell Clin Pharm 18: 684-691.
- De Falco A, Cukierman DS, Hauser-Davis RA, Rey NA (2016) Alzheimer’s disease: etiological hypotheses and treatment perspectives. Quim Nova 39: 63-80.
- Racchi M, Mazzucchelli M, Porrello E, Lanni C, Govoni S (2004) Acetylcholinesterase inhibitors: novel activities of old molecules. Pharmacol Res 50: 441-451.
- Stancu I C, Vasconcelos B, Terwel D, Dewachter I (2014) Models of β-amyloid induced Tau-pathology: the long and “folded” road to understand the mechanism. Mol Neurodegener.
- Cabezas-Opazo F A, Vergara-Pulgar K, Pérez M J, Jara C, Fuentealba C, et al. (2015) Mitochondrial dysfunction contributes to the pathogenesis of Alzheimer’s Disease. Oxid Med Cell Longev.
- Benevento C E (2011) Mitochondrial dysfunction induced by beta-amyloid peptides. Universidade Estadual de Campinas.
- Rang HP, Dale MM, Ritter JM, Flower RJ, Henderson G (2011) Interaction between Pyridostigmine Bromide and Oxidative Stress. Farmacologia 7th ed. Elsevier: Rio de Janeiro.
- Aguera Morales E, Tunez Finana I (2011) Demencia Medicine 10: 5123-5128.
- Ghanemi A (2015) Alzheimer ’s disease Therapies: Selected advances and future perspectives. Alexandria J Med 51: 1-3.
- Diamond J (2005) Report on Alzheimer’s disease and current research; Alzheimer Society of Canada. Toronto.
- McKhann G, Drachman D, Folstein M, Katzman R, Price D, et al. (1984) Clinical diagnosis of Alzheimer’s disease: report of the NINCDS-ADRDA work group under the auspices of department of health and human services task force on Alzheimer’s disease. Neurology 34: 939-944.
- Folstein MF, Folstein SE, McHugh PR (975) “Mini-mental state”. A practical method for grading the cognitive state of patients for the clinician. J Psychiatr Res 12: 189-198.
- Nitrini R, Caramelli P, Bottino CM, Damasceno BP, Brucki SM, et al. (2005) Diagnosis of Alzheimer’s disease in Brazil: Diagnostic criteria and auxiliary tests. Recommendations of the scientific department of cognitive neurology and aging of the brazilian academy of neurology. Arq. Neuropsiquiatr 63: 713-719.
- Grasso M, Piscopo P, Confaloni A, Denti MA (2014) Circulating miRNAs as biomarkers for neurodegenerative disorders. Molecules 19: 6891-6910.
- Delay C, Mandemakers W, Hébert SS (2012) MicroRNAs in Alzheimer ’s disease. Neurobiol Dis 46: 285-290.
- Cassani R, Estarellas M, San-Martin R, Fraga FJ, Falk TH (2018) Systematic review on resting-state EEG for alzheimer's disease diagnosis and progression assessment.Dis Markers.
- Jeong J (2004) EEG dynamics in patients with Alzheimer's disease.Clin Neurophysiol 115: 1490-505.
- Jeong J, Kim SY, Han SH (1998) Non-linear dynamical analysis of the EEG in Alzheimer's disease with optimal embedding dimension.Electroencephalogr Clin Neurophysiol 106: 220-228.
- Dunkin JJ, Leuchter AF, Newton TF, Cook IA (1994) Reduced EEG coherence in dementia: state or trait marker?Biol Psychiatry 35:870-879.
- Wen D, Zhou Y, Li X (2015) A critical review: coupling and synchronization analysis methods of EEG signal with mild cognitive impairment.Front Aging Neurosci.
- Anguela XM, High KA (2019) Entering the modern era of gene therapy. Annu Rev Med 70: 273-288.
- Schenk D (2002) Amyloid-β immunotherapy for Alzheimer’s disease: the end of the beginning. Nat Rev Neurosci 3: 824-828.
- Herline K, Drummond E, Wisniewski T (2018) Recent advancements toward therapeutic vaccines against Alzheimer’s disease. Expert Rev Vaccines 17: 707-721.
- Gilman S, Koller M, Black RS, Jenkins L, Griffith SG, et al. (2005) Clinical effects of Aβ immunization (AN1792) in patients with AD in an interrupted trial. Neurology 64: 1553-1562.
- WeinstockM (1999) Selectivity of cholinesterase inhibition. CNS Drugs 12: 307-323.
- Ogura H, Kosasa T, Kuriya Y, Yamanishi Y (2000) Comparison of inhibitory activities of donepezil and other cholinesterase inhibitors on acetylcholinesterase and butyrylcholinesterase in vitro. Methods Find Exp Clin Pharmacol 22: 609-613.
- Holmstedt B (1972) Plants in the Development of Modern Medicine. Cambridge University Press, Cambridge.
- Thal LJ, Fuld PA, Masur DM, Sharpless NS (1983) Oral physostigmine and lecithin improve memory in alzheimer disease. Ann Neurol 13: 491-496.
- Coelho F, Birks J (2001) Physostigmine for Alzheimer's disease. Cochrane Database Syst Rev.
- Rogers SL, Friedhoff LT (1996) The efficacy and safety of donepezil in patients with Alzheimer's disease: Results of a US multicentre randomised double blind placebo‑controlled trial The donepezil study group. Dementia 7: 293-303.
- Rogers SL, Farlow MR, Doody RS, Mohs R, Friedhoff LT (1998) A 24 week double blind placebo controlled trial of donepezil in patients with Alzheimer's disease. Donepezil study group. Neurology 50: 136-145.
- Jacobson SA, Sabbagh MN (2008) Donepezil: Potential neuroprotective and disease‑modifying effects. Expert Opin Drug Metab Toxicol 4: 1363-1369.
- Klein J (2007) Phenserine. Exp Opin Investig Drugs 16: 1087-1097.
- Greig NH, De Micheli E, Holloway H W, Yu Q, Utsuki T (2000) The experimental Alzheimer drug phenserine:Preclinical pharmacokinetics and pharmacodynamics. Acta Neurol Scand Suppl 176: 74-84.
- Fürst S, Friedmann T, Bartolini A, Bartolini R, Aiello Malmberg P, et al. (1982) Direct evidence that eseroline possesses morphine like effects. Eur J Pharmacol 83: 233-241.
- Galli A, Renzi G, Grazzini E, Bartolini R, Aiello Malmberg P, et al. (1982) Reversible inhibition of acetylcholinesterase by eseroline, an opioid agonist structurally related to physostigmine (eserine) and morphine. Biochemical Pharmac 31: 1233-1238.
- Zhan ZJ, Bian HL, Wang JW, Shan WG (2010) Synthesis of physostigmine analogues and evaluation of their anticholinesterase activities. Bioorg Med Chem Letts 20: 1532-1534.
Indexed at, Google Scholar, Crossref
Indexed at, Google Scholar, Crossref
Indexed at, Google Scholar, Crossref
Indexed at, Google Scholar, Crossref
Indexed at, Google Scholar, Crossref
Indexed at, Google Scholar, Crossref
Indexed at, Google Scholar, Crossref
Indexed at, Google Scholar, Crossref
Indexed at, Google Scholar, Crossref
Indexed at, Google Scholar, Crossref
Indexed at, Google Scholar, Crossref
Indexed at, Google Scholar, Crossref
Indexed at, Google Scholar, Crossref
Indexed at, Google Scholar, Crossref
Indexed at, Google Scholar, Crossref
Indexed at, Google Scholar, Crossref
Indexed at, Google Scholar, Crossref
Indexed at, Google Scholar, Crossref
Indexed at, Google Scholar, Crossref
Indexed at, Google Scholar, Crossref
Indexed at, Google Scholar, Crossref
Indexed at, Google Scholar, Crossref
Indexed at, Google Scholar, Crossref
Indexed at, Google Scholar, Crossref
Indexed at, Google Scholar, Crossref
Indexed at, Google Scholar, Crossref
Indexed at, Google Scholar, Crossref
Indexed at, Google Scholar, Crossref
Indexed at, Google Scholar, Crossref
Indexed at, Google Scholar, Crossref
Citation: Ojha KB, Anurag, Mukherjee S, Rajput R, Vinod YR (2022) A Discursive Examination of the Neurodegenerative Alzheimer's Disease. Clin Pharmacol Biopharm, 11: 305. DOI: 10.4172/2167-065X.1000305
Copyright: © 2022 Ojha KB, et al. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.
Share This Article
Recommended Journals
Open Access Journals
Article Tools
Article Usage
- Total views: 2104
- [From(publication date): 0-2022 - Mar 12, 2025]
- Breakdown by view type
- HTML page views: 1862
- PDF downloads: 242