Research Article Open Access
A Comparison of Prognostic Scoring Systems in Turkish Alcoholic Hepatitis Patients
Fatih Tekin*, Zeki Karasu, Elvan Isik Erdogan, Fulya Gunsar, Galip Ersoz, Omer Ozutemiz and Ulus Akarca
Ege University Medical School, Department of Gastroenterology, Izmir, Turkey
- Corresponding Author:
- Dr. Fatih Tekin
Ege Universitesi Tip Fakultesi
Gastroenteroloji Bilim Dali
Bornova, 35100, Izmir, Turkey
Tel: +90-232-3904357
Fax: +90-232-3427764
E-mail: drtekinfatih@gmail.com
Received Date: November 08, 2016; Accepted Date: November 30, 2016; Published Date: December 07, 2016
Citation: Tekin F, Karasu Z, Erdogan EI, Gunsar F, Ersoz G, et al. (2016) A Comparison of Prognostic Scoring Systems in Turkish Alcoholic Hepatitis Patients. J Gastrointest Dig Syst 6:480. doi:10.4172/2161-069X.1000480
Copyright: © 2016 Tekin F, et al. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.
Visit for more related articles at Journal of Gastrointestinal & Digestive System
Abstract
Objective: There is a lack of data concerning Turkish patients with alcoholic hepatitis (AH). The aims of the present study were to present the clinical characteristics of hospitalized AH patients and to compare the predictive ability of Maddrey’s discriminant function (DF) score, Model for End-Stage Liver Disease (MELD) score, Glasgow AH (GAHS) score and age, bilirubin, International Normalized Ratio (INR), and creatinine (ABIC) score on in-hospital mortality.
Methods: The DF score and clinical data of 34 patients with AH admitted from 2008 to 2014 were reviewed from patient’s files. Scores for MELD, GAHS and ABIC were then retrospectively calculated. A comparison of scores was obtained using area under the receiver operating characteristics curves to predict in-hospital mortality.
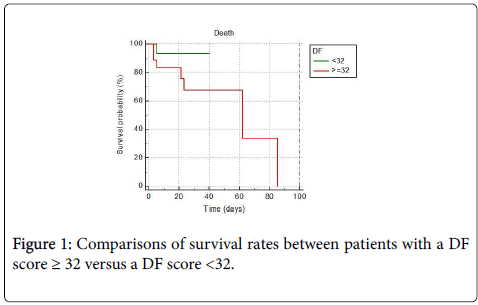
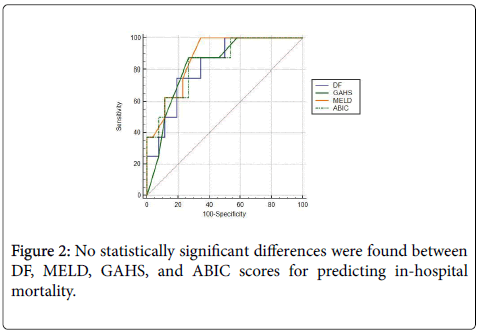
Results: In-hospital mortality was calculated at 23.5% (8/34). Treatment with corticosteroids and/or pentoxifylline was started in 18 patients with DF score ≥ 32; however, seven of them died (7/18, 39%). No significant differences were found between DF, MELD, GAHS and ABIC scores for predicting in-hospital mortality (p>0.05).
Conclusion: DF score, which is easier and more practical, can be used in clinical practice to predict in-hospital mortality because other scores have no statistical superiority. The response to corticosteroid and/or pentoxifylline treatment in patients with a DF score ≥ 32 was poor in Turkish AH patients.
Keywords
Alcoholic hepatitis; Prognostic models; Scoring system; Mortality
Introduction
Although alcoholic hepatitis (AH) is a relatively common lifethreatening liver disease, some controversy exists about its assessment. The most important two points are to assess the mortality risk and the decision to use corticosteroid and/or pentoxyfylline treatment. Several prognostic scores have been described regarding these two key factors. The first score for AH, the discriminant function (DF) score, was described in 1978 and modified in 1989 [1,2]. The second score, the Glasgow AH (GAHS) score, was developed in 2005 [3] and revealed that patients with GAHS ≥ 9 may benefit from treatment with corticosteroids [4]. Thereafter, the Model for End-Stage Liver Disease (MELD) [5,6] and age, bilirubin, International Normalized Ratio (INR) and creatinine (ABIC) [7] scores have been presented to assess patients diagnosed with AH. A value of 18 for MELD score [8] and a value of 9 for ABIC score [7] were recommended prior to starting any treatment. However, it remains unclear as to which scoring system should be selected for assessing the patient mortality risk and allow a decision for corticosteroid and/or pentoxifylline treatment. Another important point is the identification of patients who will positively respond to corticosteroid and/or pentoxifylline treatment. The Lille score [9], which includes the reduction in serum bilirubin at day 7, is known to be an accurate outcome predictor for treated patients and classifies patients as complete, partial, and non-responders. After 7 days of corticosteroid treatment, a Lille score of ≥ 0.45 is a predictive indicator of a poor response [10]. In such poor responders, the cessation of corticosteroid treatment is recommended [11]. In this study, we aimed to present the clinical characteristics of hospitalized Turkish AH patients, to show the usefulness of the Lille score in predicting the response to treatment, and to prospectively compare the predictive ability of DF, GAHS, MELD, and ABIC scores on in-hospital mortality.
Materials and Methods
Selection of the patients
Hospitalized patients who had been clinically diagnosed with AH (ICD-10 code K70.1) between 2008 and 2014 were retrieved from the hospital electronic database. The diagnosis was given at discharge by the responsible physician and detailed examinations of patients’ files were performed to confirm an exact diagnosis.
Patients were included in the study if their files were consistent with AH, which was defined as follows: the presence of alcohol use of ≥ 40 g/day up until at least 3 weeks before hospitalization and clinical properties consistent with AH. Patients with coexistent viral hepatitis, autoimmune hepatitis, suspected drug use, and alcoholic cirrhosis were excluded from the study. Patients with AH and previously diagnosed alcoholic cirrhosis were identified as acute-on-chronic liver disease, and these patients were also excluded. The study was approved by the University Ethical Committee, decree B.30.2.0.20.05.00/OY, dated July 14, 2015.
Unit protocol
Our unit protocol included prescribing of corticosteroids (prednisolone, 40 mg/day) or pentoxifylline (400 mg t.d.s) or a combination of these two treatments in patients with DF ≥ 32. The presence of sepsis, active gastrointestinal bleeding, or renal failure were considered to be contraindications for corticosteroid treatment. Routine assessment of suspected infections in the ascites, blood, urine, and lungs were performed. In such cases, patients diagnosed with an infection were started on pentoxifylline treatment. In our unit MELD, GAHS, and ABIC scores were not routinely used, but the Lille score was normally calculated on day 7 of treatment. When the Lille score was found to be ≥ 0.45, treatment was stopped. Otherwise, it was continued for 4 weeks.
Scoring systems
DF score and clinical data from the 34 patients with AH admitted from 2008 to 2014 were reviewed from the patient’s files. It was not routine protocol to use MELD, GAHS, and ABIC scores; thus, these scores were all retrospectively calculated.
Statistical analysis
Area under the receiver operating characteristics curves (AUROCs) were used to compare the different scores to predict in-hospital mortality. Pairwise comparisons of ROC curves were done using the MedCalc® (version 16.4.3,-64 bit) statistical programme, following the method described by DeLong et al. [12]. The chi-squared test was used to compare the data (age and gender) of the patients with DF scores ≥ 32 and <32, whereas the Mann-Whitney-U test was used to compare the MELD, GAHS, and ABIC scores and the hospital stay of patients with a DF ≥ 32 and <32. Any differences found in in-hospital mortality were tested with Fisher’s exact test. Kaplan-Meier survival curves were calculated and compared for MELD, GAHS, and ABIC score, and DF scores were calculated using the log-rank test. Statistical analyses were all performed using SPSS 15.0 for Windows (SPSS Inc., Chicago, USA).
Results
In total, 34 hospitalized patients (28 male; age: 23-67 years) were diagnosed with AH between 2008 and 2014, with an in-hospital mortality rate of 23.5% (8/34). Data from the 34 patients is summarized in Table 1. Among them, 18 patients had a DF score ≥ 32. Treatment with corticosteroid (prednisolone, 40 mg/day), pentoxifylline (400 mg t.d.s), and a combination treatment (corticosteroid and pentoxifylline) were started in eight, three, and seven patients, respectively. The decision of the type of treatment, i.e., corticosteroid versus a combination treatment, was made by the responsible physician. The study did not include any patients admitted with active gastrointestinal bleeding. Pentoxifylline (400 mg t.d.s) was started in one patient (patient no. 6) who had renal failure and died on day 21 post admission. There were two patients diagnosed with hepatic encephalopathy who were started with pentoxifylline, one of whom was suffering with clinical sepsis due to pneumonia and the other with a urinary tract infection. Pentoxifylline was started in these 2 patients. Five patients also had ascites with no spontaneous bacterial infections.
| Patient no |
WBC (109 ⁄ l) |
Bilirubin (mg/dl) |
PT (second) | INR | Urea (mg/dl) |
Creatinine (mg/dl) |
Albumin (mg/dl) |
7th day bilirubin (mg/dl) |
|---|---|---|---|---|---|---|---|---|
| 1 | 19100 | 20.5 | 15.6 | 1.2 | 70 | 1.25 | 3.2 | 13.5 |
| 2 | 12500 | 20.1 | 17.5 | 1.5 | 13 | 0.42 | 2.5 | 20.9 |
| 3 | 6940 | 17.9 | 36.1 | 3 | 33 | 0.93 | 3.1 | 20.5 |
| 4 | 20440 | 11.2 | 24 | 1.9 | 37 | 0.33 | 1.7 | * |
| 5 | 12510 | 9.5 | 20.4 | 1.8 | 18 | 0.47 | 2.5 | 4.2 |
| 6 | 12800 | 47.4 | 23.7 | 1.9 | 118 | 2.41 | 3.5 | 49.7 |
| 7 | 17400 | 21.1 | 20.8 | 1.7 | 27 | 0.7 | 2.5 | 15.7 |
| 8 | 10440 | 37.6 | 18.9 | 1.7 | 40 | 1.48 | 2.9 | 28.5 |
| 9 | 11020 | 31.9 | 35.3 | 1.7 | 49 | 0.74 | 2.9 | 26.7 |
| 10 | 15420 | 10.2 | 19 | 1.5 | 51 | 1.27 | 2.5 | 6.4 |
| 11 | 14760 | 45.8 | 16.3 | 1.8 | 53 | 1.64 | 3.7 | 42.2 |
| 12 | 14650 | 14.5 | 16.7 | 1.3 | 16 | 0.5 | 2.5 | 14 |
| 13 | 26140 | 18.2 | 89 | 11 | 19 | 0.93 | 3.4 | * |
| 14 | 13700 | 24.1 | 24.6 | 1.9 | 20 | 0.83 | 2.3 | 23.3 |
| 15 | 18070 | 38 | 34.6 | 2.6 | 25 | 0.77 | 3.5 | 43 |
| 16 | 12600 | 32.1 | 87.2 | 10.2 | 7 | 0.6 | 2.9 | * |
| 17 | 16800 | 3.8 | 23 | 1.7 | 25 | 0.76 | 3.4 | 1.5 |
| 18 | 22900 | 46.2 | 28 | 2.2 | 79 | 1.28 | 3.2 | 23 |
| 19 | 5400 | 4.1 | 15.3 | 1.3 | 12 | 0.39 | 3.5 | 4.5 |
| 20 | 5140 | 4.7 | 12.5 | 1 | 16 | 0.62 | 3.6 | 3.5 |
| 21 | 6360 | 8.5 | 13.3 | 1.1 | 35 | 0.74 | 2.9 | 2.4 |
| 22 | 18700 | 5.3 | 13 | 1 | 44 | 0.72 | 2.2 | 2.4 |
| 23 | 9750 | 2.4 | 14.1 | 1.1 | 21 | 0.63 | 2.4 | 1.3 |
| 24 | 9800 | 14 | 12.3 | 1 | 26 | 0.75 | 3.7 | 8 |
| 25 | 7560 | 11.3 | 13.8 | 1.1 | 15 | 0.55 | 2.4 | 5 |
| 26 | 11420 | 11.9 | 16.1 | 1.4 | 33 | 1.3 | 2.5 | * |
| 27 | 6400 | 11.2 | 13 | 1.1 | 15 | 0.6 | 2.8 | 3.5 |
| 28 | 13160 | 10.5 | 14.8 | 1.2 | 8 | 0.54 | 3.2 | ** |
| 29 | 5670 | 5 | 10.9 | 1 | 34 | 0.92 | 3 | 2.6 |
| 30 | 6360 | 22.2 | 14.3 | 1.3 | 22 | 0.49 | 3.4 | 14.4 |
| 31 | 6700 | 5.1 | 12.4 | 1 | 25 | 1.01 | 3.9 | 2.3 |
| 32 | 5900 | 3.1 | 12.2 | 1 | 21 | 1.08 | 3.9 | 2 |
| 33 | 17100 | 23.2 | 14.5 | 1.1 | 20 | 0.54 | 3 | 10.9 |
| 34 | 6710 | 17.5 | 11.5 | 1 | 20 | 1.28 | 3.7 | 5.2 |
*: died before day 7 of hospitalization;
**: patient discharged before day 7 of hospitalization
Table 1: Data of 34 patients with alcoholic hepatitis.
Among the 34 patients, 18 had a DF score ≥ 32. Seven of the 18 patients (39%) died. The results of applied scoring systems are summarized in Table 2. Among the patients with a DF score ≥ 32, the Lille score was calculated in only 15 of these patients because the remaining three patients died before day 7 of treatment (Table 2). The Lille score was found to be ≥ 0.45 in 13 of these patients (13/15, 86.6%). No changes in treatment were performed, and treatment was then stopped in all 13 patients. In our study, there were 16 patients with a DF score <32. Results of applied scoring systems in these 16 patients are summarized in Table 3.
| Patient no |
Age/Gender | DF | MELD | GAHS | ABIC | Lille | Exitus time (day) | Hospital stay (day) |
|---|---|---|---|---|---|---|---|---|
| 1 | 38/M | 33 | 22 | 7 | 7.01 | 0.665 | 14 | |
| 2 | 54/M | 41 | 22 | 8 | 8.33 | 0.98 | 57 | |
| 3 | 62/F | 124 | 30 | 10 | 10.02 | 0.99 | 23 | |
| 4 | 41/F | 62 | 23 | 9 | 6.63 | 3 | ||
| 5 | 35/M | 44 | 22 | 6 | 5.59 | 0.41 | 20 | |
| 6 | 54/M | 97 | 37 | 10 | 11.39 | 0.99 | 21 | |
| 7 | 34/M | 57 | 24 | 9 | 6.65 | 0.71 | 31 | |
| 8 | 45/M | 65 | 30 | 8 | 9.3 | 0.94 | 28 | |
| 9 | 67/M | 134 | 25 | 11 | 10.83 | 0.99 | 57 | |
| 10 | 52/M | 38 | 22 | 9 | 7.59 | 0.87 | 85 | |
| 11 | 33/M | 63 | 28 | 9 | 8.59 | 0.98 | 62 | |
| 12 | 42/M | 32 | 19 | 6 | 6.55 | 0.91 | 28 | |
| 13 | 52/F | 367 | 44 | 11 | 15.37 | 3 | ||
| 14 | 42/M | 78 | 26 | 9 | 7.89 | 0.97 | 21 | |
| 15 | 53/M | 137 | 30 | 11 | 10.56 | 0.99 | 17 | |
| 16 | 23/M | 373 | 46 | 10 | 13.2 | 5 | ||
| 17 | 51/M | 50 | 17 | 9 | 6.99 | 0.81 | 9 | |
| 18 | 30/M | 115 | 32 | 11 | 8.81 | 0.15 | 44 |
Table 2: Data of 18 alcoholic hepatitis patients with a DF score ≥ 32.
| Patient no |
Age Gender | DF | MELD | GAHS | ABIC | Exitus time (day) | Hospital stay (day) |
|---|---|---|---|---|---|---|---|
| 19 | 46/F | 15 | 15 | 6 | 6.06 | 16 | |
| 20 | 44/M | 6 | 12 | 5 | 5.76 | 10 | |
| 21 | 54/M | 10 | 15 | 8 | 7.13 | 15 | |
| 22 | 32/M | 5 | 13 | 7 | 4.65 | 40 | |
| 23 | 54/F | 7 | 11 | 6 | 6.66 | 15 | |
| 24 | 38/M | 14 | 17 | 6 | 5.94 | 7 | |
| 25 | 44/M | 15 | 16 | 6 | 6.31 | 14 | |
| 26 | 49/M | 26 | 22 | 7 | 7.36 | 5 | |
| 27 | 49/M | 12 | 17 | 6 | 6.85 | 8 | |
| 28 | 30/M | 19 | 17 | 6 | 4.96 | 3* | |
| 29 | 36/M | 5 | 13 | 6 | 5.07 | 13 | |
| 30 | 58/M | 28 | 21 | 8 | 8.76 | 20 | |
| 31 | 56/M | 5 | 13 | 6 | 7.09 | 13 | |
| 32 | 39/M | 4 | 12 | 5 | 5.33 | 10 | |
| 33 | 36/F | 30 | 19 | 8 | 6.69 | 28 | |
| 34 | 32/M | 17 | 17 | 8 | 5.64 | 22 |
Table 3: Data of 16 alcoholic hepatitis patients with a DF score <32.
One patient (patient no. 26; DF score 26) died due to a myocardial infarction on day 5 of hospitalization. Patients with a DF score <32 had shorter hospital stay, and a lower in-hospital mortality rate (Figure 1) when compared to patients with a DF score ≥ 32. Comparisons of the scores of patients with DF ≥ 32 versus DF <32 are shown in Table 4. No statistically significant differences were found between DF, MELD, GAHS, and ABIC scores for predicting in-hospital mortality (p>0.05) (Figure 2).
| Parameter | Group 1: DF ≥ 32 (n = 18) |
Group 2: DF<32 (n = 16) |
p-values |
|---|---|---|---|
| Age (years ±SD) | 44.9 ± 5.8 | 43.6 ± 4.9 | 0.717 |
| Gender (male / female) | 15 / 3 | 13 / 3 | 0.874 |
| MELD (mean ±SD) | 27.7 ± 4.0 | 15.6 ± 1.7 | <0.001 |
| GAHS (mean ±SD) | 9.2 ± 0.7 | 6.4 ± 0.5 | <0.001 |
| ABIC (mean ±SD) | 9.0 ± 1.3 | 6.3 ± 0.6 | <0.001 |
| Hospital stay (days ±SD) | 29.5 ± 11.0 | 15.4 ± 5.0 | 0.010 |
| In-hospital mortality (n) | 7 | 1 | 0.043 |
Table 4: Comparisons of the patients with DF score ≥ 32 versus DF score <32 (overall n=34).
Discussion
To our knowledge, this is the first study that documents the clinical characteristics of Turkish AH patients. The present study showed that more than 50% of the hospitalized AH patients (18/34) had a DF score ≥ 32, and corticosteroid, pentoxifylline, or combination treatment had a limited effect on in-hospital mortality. Seven of the 18 treated patients (39%) with a DF score ≥ 32 died. The Lille score was found to be ≥ 0.45 in 86.6% of the treated patients, and their treatment was stopped. Switching to pentoxifylline was performed in none of the patients receiving corticosteroid treatment because an early switch in treatment to pentoxifylline was found to have no effect on patient mortality [13]. Therefore, no additional treatment modality was left, except supportive treatments for these patients. Granulocytapheresis [14] and molecular adsorbent recirculating system (MARS) [15] treatments have also shown to be ineffective in treating AH patients, and new therapeutic options should be considered in non-responsive ones. In these patients, early liver transplantation may be considered after a careful selection process [16]. However, this treatment modality is still under review in Turkey, and to our knowledge, no early liver transplantation has been performed till date.
Many studies have shown that corticosteroids are more effective than pentoxifylline in AH patients. A recent multicenter, open-labeled, randomized trial confirmed this result [17]. In our study corticosteroids, pentoxifylline, and combination treatment (corticosteroid and pentoxifylline) were started in eight, three and seven patients, respectively. Both the European Association for the Study of the Liver (EASL) [11] and the American Association for the study of Liver Diseases (AASLD) [8] guidelines recommend patients with AH and a DF score ≥ 32 receive treatment with prednisolone at 40 mg/day for 4 weeks. However, several conditions, such as the presence of gastrointestinal bleeding, renal failure, and sepsis are accepted as contraindications for corticosteroid treatment. In our study, pentoxifylline treatment was started in three patients because of the presence of sepsis in two patients and renal failure in one patient. Combination treatment was started in seven patients in our study, although a large randomized controlled trial of 270 patients with severe AH failed to show any benefits of combination treatment over the use of corticosteroids alone [18]. Results of a recent well-designed study confirmed this result [19]. In our study, the decision to use treatment with corticosteroids versus combination treatment was made by the responsible physician.
In fact, several previously published studies have focused on a comparison of the scoring systems for the assessment of AH patients, but the findings were contradictory in each one, with no apparent clear explanation for the results [6,20-22] ". In this study, we retrieved DF scores from patients’ files and did not routinely use MELD, GAHS, or ABIC scores. Thus, these scores were retrospectively calculated. The ability of each score to predict in-hospital mortality was evaluated using receiver operating characteristics curves, and AUROCs were used to compare the scores. There were no differences found between DF, MELD, GAHS, and ABIC scores for predicting in-hospital mortality, which correlates with the results of a previously published Danish study [21]. It can, therefore, be concluded that a DF score, which is easier and more practical, can be used in clinical practice to predict in-hospital mortality because other scores have no superiority in the evaluation of AH patients.
There are a few limitations of our study, such as the small number of patients and the absence of a liver biopsy. In patients, AH is characterized by a sudden rise in serum bilirubin levels, coagulopathy, liver failure, and portal hypertension-related complications. A recent study using Tru-cut needles to obtain a liver biopsy revealed that the majority of patients with AH also had underlying cirrhosis [23]. Although the occurrence of AH can occur as the primary symptom in some patients, it may in fact be an exacerbation of pre-existing alcoholic cirrhosis in others. Therefore, AH should be distinguished from compensated cirrhotic patients. In addition, patients with alcoholic liver disease can present with an episode of jaundice and liver decompensation for reasons other than superimposed AH, such as sepsis, biliary obstruction, or drug-induced liver injury. Therefore, in alcoholic patients with other potential causes of jaundice or those involved in clinical trials, a transjugular liver biopsy is recommended to confirm the existence of AH [8,11], otherwise, routine liver biopsies are not utilized in many clinics, including our liver unit [11]. In our study, patients with AH and previously known alcoholic cirrhosis were considered as having acute-on-chronic liver disease, and these patients were, therefore, excluded. Despite this careful selection, AH patients with underlying unknown compensated cirrhosis might have been included in the study because of the absence of a liver biopsy. Such a condition might then result with a heterogeneous study group, including both AH patients and acute-on-chronic patients.
In studies by Louvet et al. [9] and Lafferty et al. [22], the Lille response to medical treatment was reported as 40% and 43% respectively. In the present study, the Lille score was found to be ≥ 0.45 in 86.6% of the treated patients, showing that Turkish AH patients were more likely to be non-responsive to medical treatment. Therefore, in light of these results indicating that existing therapies were not effective in many patients, alternative targeted approaches are urgently needed.
In conclusion, DF score which is easier and more practical, can be used in clinical practice to predict in-hospital mortality because other scores have no superiority in the evaluation of AH patients. The response to corticosteroid and/or pentoxifylline treatment in patients with a DF score ≥ 32 was found to be poor in Turkish AH patients, indicating that new therapeutic options should be considered and used in non-responsive ones.
References
- Maddrey WC, Boitnott JK, Bedine MS, Weber FL Jr, Mezey E, et al. (1978) Corticosteroid therapy of alcoholic hepatitis. Gastroenterology 75: 193-199.
- Carithers RL, Herlong HF, Diehl AM, Shaw EW, Combes B, et al. (1989) Methylprednisolone therapy in patients with severe alcoholic hepatitis: a randomized multicenter trial. Ann Intern Med 110: 685-690.
- Forrest EH, Evans CD, Stewart S, Phillips M, Oo YH, et al. (2005) Analysis of factors related to mortality in alcoholic hepatitis and the derivation and validation of the Glasgow alcoholic hepatitis score. Gut 54: 1174-1179.
- Forrest EH, Morris AJ, Stewart S, Phillips M, Oo YH, et al. (2007) The Glasgow alcoholic hepatitis score identifies patients who may benefit from corticosteroids. Gut 56: 1743-1146.
- Dunn W, Jamil LH, Brown LS, Wiesner RH, Kim WR, et al. (2005) MELD accurately predicts mortality in patients with alcoholic hepatitis. Hepatology41: 353-358.
- Srikureja W, Kyulo NL, Runyon BA, Hu KQ (2005) MELD is a better prognostic model than the Child-Turcotte-Pugh score or Discriminant Function in patients with alcoholic hepatitis. J Hepatol 42: 700-706.
- Dominguez M, Rincon D, Abraldes JG, Miquel R, Colmenero J, et al. (2008) A new scoring system for prognostic stratification of patients with alcoholic hepatitis. Am J Gastroenterol 103: 2747-2756.
- O'Shea RS, Dasarathy S, McCullough AJ; Practice Guideline Committee of the American Association for the Study of Liver D, Practice Parameters Committee of the American College of G (2010) Alcoholic liver disease. Hepatology 51:307-328.
- Louvet A, Naveau S, Abdelnour M, Ramond MJ, Diaz E, et al. (2007) The Lille model: a new tool for therapeutic strategy in patients with severe alcoholic hepatitis treated with steroids. Hepatology 45: 1348-1154.
- Mathurin P, O’Grady J, Carithers RL, Phillips M, Louvet A, et al. (2011) Corticosteroids improve short term survival in patients with severeealcoholic hepatitis: meta-analysis of individual patient data. Gut 60: 255-260.
- European Association for the Study of Liver (2012) EASL clinical practical guidelines: management of alcoholic liver disease. J Hepatol 57: 399-420.
- DeLong ER, DeLong DM, Clarke-Pearson DL (1988) Comparing the areas under two or more correlated receiver operating characteristic curves: a nonparametric approach. Biometrics 44: 837-845.
- Louvet A, Diaz E, Dharancy S, Coevoet H, Texier F, et al. (2008) Early switch to pentoxifylline in patients with severe alcoholic hepatitis is inefficient in non-responders to corticosteroids. J Hepatol 48: 465-470.
- Morris JM, Dickson S, Neilson M, Hodgins P, Forrest EH (2010) Granulocytapheresis in the treatment of severe alcoholic hepatitis. Eur J Gastroenterol Hepatol 22: 457-460.
- Boitard J, Louvet A, Bismuth B (2007) Tolerance and efficacy of the MARS system in patients with severe alcoholic hepatitis non-responder to steroids: a pilot study. Hepatology 46: 327.
- Mathurin P, Moreno C, Samuel D, Dumortier J, Salleron J, et al. (2011) Early liver transplantation for severe alcoholic hepatitis. N Engl J Med 365: 1790-1800.
- Caballeria J (2015) Is pentoxifylline still an option in severe alcoholic hepatitis? Hepatology 62: 1644.
- Mathurin P, Louvet A, Dao T, Nahon P, Diaz E, et al. (2011) Addition of pentoxifylline to prednisolone for severe alcoholic hepatitis does not improve 6-month survival: results of the Corpentox trial. Hepatology 54: 391.
- Thursz MR, Richardson P, Allison M, Austin A, Bowers M, et al. (2015) Prednisolone or pentoxifylline for alcoholic hepatitis. N Engl J Med 372: 1619-1628.
- Forrest EH, Fisher NC, Singhal S, Brind A, Haydon G, et al. (2010) Comparison of the Glasgow alcoholic hepatitis score and the ABIC score for the assessment of alcoholic hepatitis. Am J Gastroenterol 105: 701-702.
- SandahlTD, Jepsen P, Ott P, Vilstrup H (2011) Validation of prognostic scores for clinical use in patients with alcoholic hepatitis. Scand J Gastroenterol46: 1127-1132.
- Lafferty H, Stanley AJ, Forrest EH (2013) The management of alcoholic hepatitis: a prospective comparison of scoring systems. Aliment PharmacolTher38: 603-610.
- Altamirano J, Miquel R, Katoonizadeh A, Abraldes JG, Duarte-Rojo A, et al. (2014) A histologic scoring system for prognosis of patients with alcoholic hepatitis. Gastroenterology 146: 1231-1239.
Relevant Topics
- Constipation
- Digestive Enzymes
- Endoscopy
- Epigastric Pain
- Gall Bladder
- Gastric Cancer
- Gastrointestinal Bleeding
- Gastrointestinal Hormones
- Gastrointestinal Infections
- Gastrointestinal Inflammation
- Gastrointestinal Pathology
- Gastrointestinal Pharmacology
- Gastrointestinal Radiology
- Gastrointestinal Surgery
- Gastrointestinal Tuberculosis
- GIST Sarcoma
- Intestinal Blockage
- Pancreas
- Salivary Glands
- Stomach Bloating
- Stomach Cramps
- Stomach Disorders
- Stomach Ulcer
Recommended Journals
Article Tools
Article Usage
- Total views: 4263
- [From(publication date):
December-2016 - Apr 19, 2025] - Breakdown by view type
- HTML page views : 3398
- PDF downloads : 865