A Comparison between Task Oriented and Client-Centred Task-Oriented Approaches to Improve Upper Limb Functioning in People with Sub-Acute Stroke
Received: 26-Aug-2015 / Accepted Date: 24-Sep-2015 / Published Date: 30-Sep-2015 DOI: 10.4172/2165-7025.1000276
Keywords: Task-oriented training; Client-centred task oriented training; Goal setting; Upper limb function
361105Introduction
Stroke is the third leading cause of death after cancer and heart diseases, produces considerable morbidity and is an important public health problem all over the world. Stroke is a major public health concern, being among the most common causes of death and disability [1]. Motor impairments are most prevalent of all deficits seen after stroke, usually with involvement of the face, arm and leg alone or in various combinations. Motor impairments include involvement of cranial nerves, muscle power & tone, reflexes, balance, gait, coordination and apraxia [2].
The paretic upper limb is a common and undesirable consequence of stroke that increases activity limitation. The recovery process of upper extremity function is often slower than the recovery process of lower extremity function [3]. Upper limb dysfunction in stroke is characterised by paresis, loss of manual dexterity and movement abnormalities that may impact considerably on the performance of ADL’s. Grasping, holding and manipulating objects are daily functions that remain deficient in 55% to75% of patients 3 to 6 months post stroke [4].
In Physiotherapy, a number of interventions studies have been published evaluating the effect of various rehabilitation methods in improving upper-extremity motor control and functioning [5-17]. Task oriented training is commonly used method to retrain patients with hemiplegia.
Task oriented training is a therapeutic approach based on the system theory of motor control. This was given by Bernstein in 1967 to retain the patients with movement disorders. This approach utilizes a training program that focuses on specific functional tasks to engage the neuromuscular and musculoskeletal system. There is strong evidence that early, intense and task-related training improved motor recovery and cortical reorganization after stroke [11,18-22].
Goal setting in Neuro-rehabilitation
Goals are central to the process of rehabilitation. Individual members of a team are more likely to coordinate their contributions if they share common goals, therefore it is important to involve the patient in the goal-setting process [23].
Two important components of the goal setting process are identification of the patient’s problems and goal-setting [24]. Whiteneck states that the individual should be viewed as the primary focus of the rehabilitation process, and subjective perceptions are needed to fill in the gaps left by the traditional objective assessments [25]. Pollock claims that when the client participates in goal-formulation, planning and decision-making, the potential for active participation in the rehabilitation process has been shown to increase. Individuals must set the goals in order to be able to solve the problems, or else the feeling of control over their health is decreased [26].
Locke and Latham’s goal-setting theory asserts that goals are immediate regulators or causes of behaviour (e.g., task or work performance). It starts with situational, the specific, conscious, motivational factors closest to action: goalsand intentions. The theory then worked backward to determine what caused goals to beformed and what made them effective [27,28].
Goal Setting is defined as the process of agreeing on goals, this agreement usually being between the patient and all other interested parties. The process might include setting goals at various levels and in various time frames [29]. Goal setting is recommended as good clinical practice in stroke. Generally, two types of goal settings are used in clinical practice. In one type of goal setting, the rehabilitation team assesses the patient, identify the problems and set the goal accordingly. The second newer approach is client-centred approach in which the goal is set according to the client and his relatives’ needs and priorities [30].
Client-centred approach
Client-centred care has become an increasingly important health care concept in recent decades. The shift toward addressing clientcentred care has been influenced by factors including a rise in client expectations, changing culture, availability of information to the general public and the rise in consumerism [31,32]. Moreover, the emphasis on client-centred care reflects current western societal beliefs about independence, the rights of individuals, and the importance of access to information [33].
Client-centred approach promotes clients and health care providers as equal partners in the management of the client’s health care and rehabilitation process with an understanding of and respect for the clients’ individual needs. Moreover, adopting a client-centred approach strives to incorporate clients’ perspectives into the provision of services at the system level and to maximize the chance of a successful transition between rehabilitation programs and the community [32].
Studies reveal that Task oriented training and Client-centred care is both effective in rehabilitation for the stroke patient alone but there are few studies in which the task oriented training combined with client-centred goal setting for rehabilitation was used. So, to find out the better strategy for stroke rehabilitation, we combined the task oriented approach with client centred care and compared it with taskoriented training in which goals are set according to therapist’s clinical judgement.
Purpose of the study
To compare the different types of goal setting, one by physiotherapist and other by client himself in stroke rehabilitation, Client-centred goal setting combined with task-oriented approach to improve upper limb functioning in sub-acute stroke patients.
Methodology
Study design – a randomized clinical trial
• Sample: - Study consisting 40 participants (Males and Females) 20 in each group, with their first stroke.
• Sampling design- Simple Random Sampling
• Sampling method- Lottery method
• Source of subjects – M.M. Medical College and hospital and Private hospitals of Ambala. All the participants were residents of different cities of Haryana, who volunteered for the study.
Inclusion criteria
1. Patients between ages 40-65 years of age.
2. Both Male and Female.
3. Paresis of Upper limb (MCA infarct).
4. Duration of stroke within 1-5 months, prior to commencement of study.
5. Patients had an ARAT score less than 52.
6. Able and willing to participate in 8 weeks study and to sign consent form.
Exclusion criteria
1. Any associated medical and high risk cardiovascular disorder.
2. Any neurological disorder or pain that might limits arm movement.
3. Chronic and secondary stroke.
4. Severe cognition impairment (MMSE<23).
5. Still enrolled in any form of physical therapy.
Independent variable
Task-oriented training
Client centred Goal setting
Dependent variable
Upper limb function
Instrumentation
Wooden blocks (2.5, 5, 7.5 and 10 cubic cm) Fig-3.2
Ball bearing of 6 mm.
Tubes (diameter- 1 and 2.25 cm)
Marble (diameter- 1.5 cm)
Cricket ball (diameter- 7.5 cm)
Knee hammer
Washer bolt (diameter 3.5 cm)
Stone
Bottle
Glass
Outcome measures
Action research arm test: The Action Research Arm Test (ARAT) is an evaluative measure to assess specific changes in Upper limb function among individuals with stroke. It assesses a client’s ability to handle objects differing in size, weight and shape and therefore can be considered to be an arm-specific measure of activity limitation. It was designed to assess recovery in the upper limb following cortical damage. The test consists of 19 items grouped in subtests (grasp, grip, pinch, and gross arm movement) and performance of each item is rated on a 4-point scale ranging from 0 (no movement possible) to 3 (movement performed normally). The maximum obtainable score is 57. The administration of the ARAT is quick and simple, and it has good reliability and validity [33-36].
Canadian occupational performance measure: The Canadian Occupational Performance Measure (COPM) is an individualized measure designed for use by occupational therapists to detect selfperceived change in occupational performance problems over time.
Administration -Completed through a five-step semi-structured interview individualized to each patient.
Step 1: Patient identifies problems in performance of daily activities.
Step 2: Patient determines priorities by rating the importance of each problem on a 10--‐point scale (from ‘not important at all’ to ‘extremely important’).
Step 3: Patient identifies the five most important problems he or she perceives during Daily activities.
Step 4: Patient rate on a 10--‐point scale the performance (from ‘not able to do it at all’ to able to do it extremely well’).
Step 5: Patient rates his or her satisfaction (from ‘not satisfied at all’ to ‘extremely satisfied’) with regard to each of the five prioritized problems.
The COPM focuses on patient-centered care and it Identifies patient-specific problems not assessed in other standardized measurements.
Similarly their present performance ability and satisfaction were assessed using scoring cards as provided with the COPM manual. Sum of the scores for Performance and Satisfaction for 5 identified problems were equated to baseline score on COPM for Performance & Satisfaction. The COPM having good reliability and validity [37-40].
Protocol: 40 patients of stroke who fulfilled the inclusion criteria were included in the study. All patients were evaluated by ARAT and COPM prior to the treatment and pre-test readings were recorded. The subjects were assigned into two groups i.e. Group A and Group B comprising with 20 subjects in each group.
Patients in Control group (group A) were treated with taskoriented program after deciding goals for rehabilitation therapeutically by physiotherapist himself. Firstly, the therapist assessed the patients, identified their problems and then set the goals for rehabilitation accordingly. Then Task-oriented training was given for 40 minutes per session.
In Experimental group (group B), client centred approach was used in setting the goals. Here the therapist plans therapy with the client and their relative as the decision-maker and implements therapy based on the goals and priorities identified by the clients themselves. After deciding the goals, task oriented program were given to the patients to enhance the physical performance components that were identified by the subjects as ‘important’ according to the COPM.
After 8 weeks of intervention, patients were again evaluated with Action Research Arm Test and COPM.
Client-centred task-oriented program: The client-centred approach is a newer approach in which goals are set according to clients and their relatives’ needs and priorities. Client-centred goal setting encourages the patient to identify their specific aims in relation to their recovery. These aims are then translated into relevant and meaningful goals and used as the basis for the individual’s rehabilitation. These goals are used as the rehabilitation framework for each patient.
The client centred approach includes three stages- patient priorities, current status and goal setting. Patient priorities were identified by the administered use of COPM scale. Current status was known by the proper assessment and goals are set by the client-centred. Then, according to previously set goals, task-oriented training was given by the physiotherapist to improve clients’ performance and satisfaction. The list contains both simple and more complex tasks and upper extremity functional exercises.
Task-oriented training: Task-oriented intervention, inspired by Alon et al, was a standardized programme15 which was modified from that recommended by Carr and Shepherd (Table 1). This program was conducted for 40 minutes per session for 5 days for 8 weeks. Components of task oriented training include range of motion exercises, weight bearing and supportive reactions, reaching, grasping, holding and release activities upper extremity ADL activities (Table 1).
| Passive or Active ROM | Passive ROM: wrist/elbow/shoulder, self or by family member. Active/assistive ROM: wrist/elbow/shoulder. Active ROM: wrist/elbow/shoulder in sitting and standing. Active ROM with resistance: wrist/elbow/shoulder in sitting and standing. |
| Weight bearing and supportive reactions | Seated weight bearing (forearm on table top) with affected upper extremity. Extending arms, seated or standing with bilateral upper extremity weight bearing on table. Extended arms with transitional movements side lying to sit, sit to stand. Extended arms and wrist/hand on wall with change in base of support, e.g. weight shifting, single lower extremity support, lateral wall walking. |
| Reaching activities | Forward supported reach bilaterally with cane on table top (elbow extension). Forward supported reach with shoulder elevation, elbow/wrist extension. Reaching against gravity in frontal and sagittal planes. Reaching overhead with active wrist/hand movements. Dynamic reaching to a target, e.g. catches a ball. |
| Grasping, holding and release | Grasp, hold and release containers with gravity minimized (on table). Pick up and move/release small object on table. Pick up and move/release large objects without proximal support. Incorporate key and pinch grips in hold and release. |
| Upper extremity ADLs | Dressing, grooming. Carrying objects with affected upper extremity. Opening bottles, stabilizing with paretic extremity for reaching. Writing, drawing and manipulating small objects. Folding and hanging towels. Self-feeding. |
Table 1: Exercise programme (Received by both the groups).
The number and complexity of the exercises were adjusted by the research therapist for each patient so that he or she was able to practice independently or with assistance from a family member. The specific exercises were further modified by the research therapist as upper extremity performance continued to improve throughout the 8 week study period. Patients practiced their individually tailored task oriented program with the attending therapists (40- minute session, given once a day) 5 days each week.
Ethical approval and informed consent: Before implementing the study, an approval from university ethical committee was taken. All the subject who participated in study received a written explanation about the trial before entry into study and the Informed consent was taken from all the subjects with Stroke, who were willing to participate in study.
Data analysis: The data analysed using SPSS version 22 .0 software package. Descriptive statistics were used for subject’s demographic characteristics. The p-value was set at 0.05. Paired ‘T’ test was used to analyse within group analysis. Unpaired ‘T’ was used to analyse between group analyses. Levene’s Test is used to calculate for Equality of Variances.
Result
Demographic profile
Total 58 subjects assessed for study, out of that 15 were unable to fulfill the inclusion criteria (5 medically unstable, 3 had cognitive dysfunction, 4 had flaccidity and mild spasticity so unable to initiate the movements and 3 were refused to participate).There was 3 drop out because they unable to complete the total intervention period, so total 40 subject of stroke included in this study.The patientswere divided into two equal groups (20 patients in each group) asgroup A (Taskoriented PT program), group B (Client-centred goal setting with Taskoriented PT intervention). Firstly, baseline data was measured in terms of age, gender and side affected.
Above table shows demographic data of the population of group A and group B Flow chart 1. The groups did not differ regarding age, gender and side affected. Difference in Age of both groups was not significant with p-value o.133.
Discussion
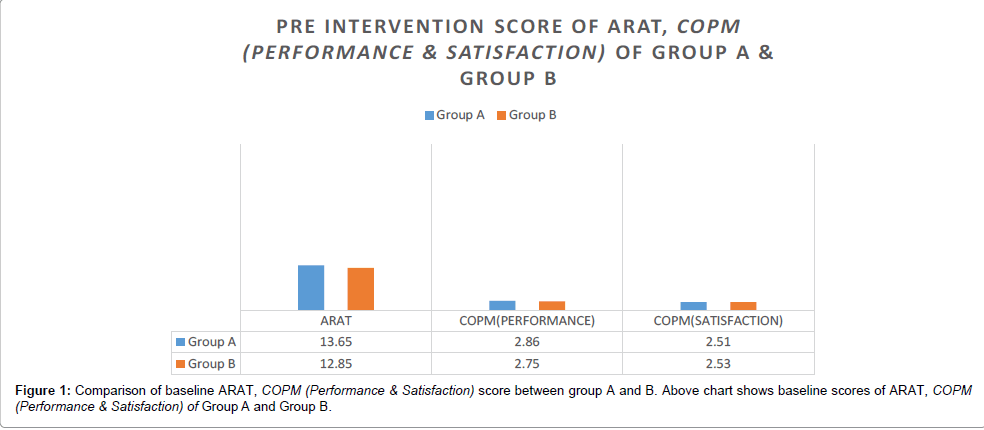
The main objective of the present study was to compare the different types of goal setting, one by physiotherapist and another by active involvement of client and their relatives in client-centred goal setting combined with task-oriented approach for both the groups to improve upper limb functioning in sub-acute stroke patients. Analysis was done at three levels, first as baseline level between the groups, 2nd from pre to post intervention level within group and later at post intervention level. When analysis was done at baseline level it was found that there was no statistically significant difference between both the groups as it is shown in Tables 2 and 3 and Figure 1 which shows that both the groups were matched at baseline level.
| GROUP A | GROUP B | DEGREE OF FREEDOM | T-TEST | P VALUE | ||
| AGE | 56.75 ±4.58 | 54.40± 5.07 | 38 | 1.537 | .133(NS) | |
| GENDER | MALE | 13 | 11 | |||
| FEMALE | 7 | 9 | ||||
| SIDE AFFECTED | RIGHT | 12 | 8 | |||
| LEFT | 9 | 11 | ||||
Table 2: Demographic Characteristics of the Population.
| GROUP A (MEAN ± SD) |
GROUP B (MEAN ± SD) |
DEGREE OF FREEDOM | T-VALUE | P VALUE | |
| ARA TEST | 13.65 ± 2.36 | 12.85 ± 2.34 | 38 | 1.073 | .290(NS) |
| COPM(PERFORMANCE) | 2.86 ± .36 | 2.75 ± .41 | 38 | .894 | .377(NS) |
| COPM(SATISFECTION) | 2.51 ± .40 | 2.53 ± .45 | 38 | -.147 | .884(NS) |
P<0.05* shows a statistically significant result
The above table shows that groups are matched for their baseline characters. The baseline values for ARAT, COPM (Performance & Satisfaction) are not significant with p-values 0.290, 0.377 and 0.884 respectively.
Table 3: Baseline Comparison of Group A and B.
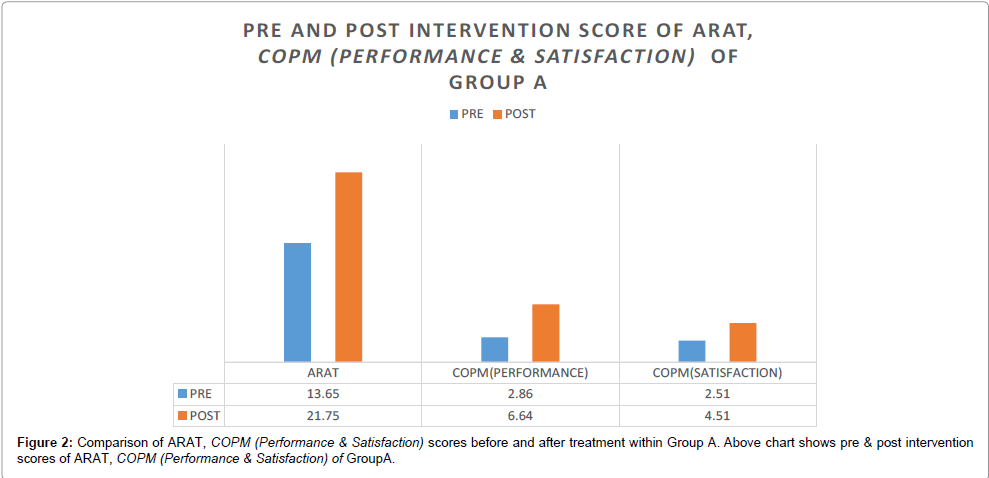
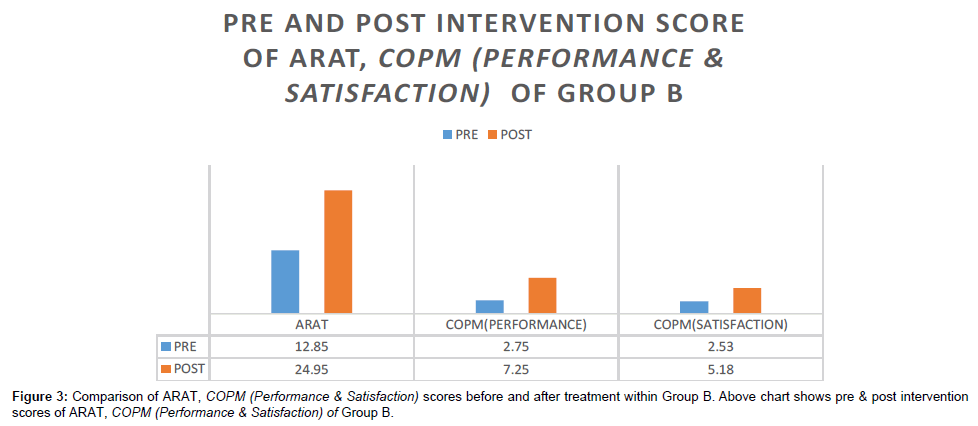
When analysis was done from pre to post intervention level, results show that there is statistically significant difference between both the groups. Both the groups improve significantly in ARAT and COPM (performance and satisfaction) as it is shown in Tables 4 and 5, and Figures 2 and 3, Which suggest that task oriented training is an effective intervention strategies for stroke rehabilitation.
| GROUP A | PRE (MEAN ± SD) | POST (MEAN ± SD) |
DEGREE OF FREEDOM | T-VALUE | P VALUE |
| ARA TEST | 13.65 ± 2.36 | 21.75 ± 4.11 | 19 | 15.80 | .000(S) |
| COPM(PERFORMANCE) | 2.86 ± .36 | 6.64 ± .66 | 19 | 21.642 | .000(S) |
| COPM(SATISFECTION) | 2.51 ± .40 | 4.51 ± .57 | 19 | 15.41 | .000(S) |
P<0.05* shows a statistically significant result
The above table shows pre & post intervention values of ARAT, COPM (Performance & Satisfaction) of group A. The post intervention values for ARAT, COPM (Performance & Satisfaction) are significant with p-values 0.000, 0.000 and 0.000 respectively.
Table 4: Pre and post intervention comparison of ARAT and COPM (Performance & Satisfaction) within Group A.
| PRE (MEAN ± SD) |
POST (MEAN ± SD) |
DEGREE OF FREEDOM(df) |
T-VALUE | P VALUE | |
| ARA TEST | 12.85 ± 2.34 | 24.95 ± 3.94 | 19 | -16.94 | .000(S) |
| COPM(PERFORMANCE) | 2.75 ± .41 | 7.25 ± .56 | 19 | -36.17 | .000(S) |
| COPM(SATISFECTION) | 2.53 ± .45 | 5.18 ± .61 | 19 | -14.82 | .000(S) |
P<0.05* shows a statistically significant result
The above table shows pre & post intervention values of ARAT, COPM (Performance & Satisfaction) of group B. The post intervention values for ARAT, COPM (Performance & Satisfaction) are significant with p-values 0.000, 0.000 and 0.000 respectively.
Table 5: Pre and post intervention comparison of ARAT and COPM (Performance & Satisfaction) within Group B.
The results of the present study are consistent with the findings of the study done by Blennerhasett et al. [41] who investigated the effects of additional practice of either upper limb or mobility tasks in stroke patients and concluded that additional task-related practice is effective in improving functional outcomes during in patient stroke rehabilitation, the results of the present study are consistent with the findings of this study.
Salbach et al. [42] reported that task oriented intervention did not improve voluntary movement or manual dexterity of affected arm in chronic stroke patients. The greater relative improvements reported in this study indicated that the effect of task oriented training is magnified if it is commenced during early rehabilitation.
Liepert et al. [43] examined the effects on dexterity and motor cortex function of a single task-oriented session focussed on improving dexterity of mildly to moderately paretic hand in patients early (4-8 weeks) after stroke. They observed that the size of the representation in contra-lateral motor cortex of paretic hand enlarged whereas that of the unaffected hand was unchanged. These changes are associated with increased activity in ipsilesional primary cortex and redistribution of activity in several areas of sensorimotor network.
In the current study, the subjects worked with the therapist to safely practice new movement strategies to improve their functional ability in intervention period that is pre requisite for returning to work and regaining the ability to perform routine activities necessary for an independent life style. The task-specific program was modified in accordance with the individual patient’s progress.
The finding of present study is also supported by Jang et al. [44] who described that task-oriented training focuses on practice of skilled motor performance is the critical link to facilitating neural reorganization and rewiring in the central nervous system. Furthermore Cook et al. [45] explained in their book “Motor Control- Translating research into clinical practice” that task-oriented approach is based on the system theory of motor control. This theory states that normal movement emerges as an interaction among many different systems, each contributing different aspects of motor control. In task oriented approach movement is organized around a behavioural goal; thus multiple systems are organized according to the inherent requirements of the task being performed.
In this approach, the patient is working on functional tasks rather than on movement patterns for movement sake alone. Feedback is a fundamental characteristic of this approach. As the patient getting feedback and the activities of daily living are emphasized so this goes to long term memory.
When analysis was done at post intervention level, it was found that there was no statistically significant difference between ARAT scores of both the groups which suggest that both the groups at similar level at post intervention level in terms of upper limb function. Client-centred Task-oriented group had significant higher COPM (performance and satisfaction) score as compared with control group as it is shown in Table 6 and Figures 4. The results obtained after the data analysis did not support the null hypothesis and thus, the null hypothesis was rejected and the alternate hypothesis was accepted in terms of COPM (performance and satisfaction).
| GROUP A (MEAN ± SD) |
GROUP B (MEAN ± SD) |
DEGREE OF FREEDOM | T-VALUE | P VALUE | |
| ARA TEST | 21.75 ± 4.11 | 24.95 ± 3.94 | 38 | -2.512 | .016(NS) |
| COPM(PERFORMANCE) | 6.64 ± .66 | 7.25 ± .56 | 38 | -3.147 | .003(S) |
| COPM(SATISFECTION) | 4.51 ± .57 | 5.18 ± .61 | 38 | -3.548 | .001(S) |
P<0.05* shows a statistically significant result
The above table shows pre & post intervention values of ARAT, COPM (Performance & Satisfaction) of group A & B. The post intervention values for ARAT, COPM (Performance & Satisfaction) are significant with p-values 0.016, 0.003 and 0.001 respectively.
Table 6: Post Intervention comparison of ARAT, COPM (Performance & Satisfaction) scores of Group A and B.
The significant improvement of COPM (performance and satisfaction) in experimental group is due to combined Task-oriented approach and goal setting which is decided by the patient with the help of COPM. When analysis was done between components of COPM (Performance and Satisfaction), it is seen that satisfaction score is more than performance. The Client-centred approach, which requires the active role of the clients in treatment implementation, enables them to see the improvements by themselves, even there is no significant difference in both the groups in upper extremity function assessed by ARAT.
The above finding is supported by a similar study done in a Neurorehabilitation setting by Bodiam et al [46] in which it was seen that the change in ‘satisfaction’ score is more than that in the ‘performance’. This could be attributed to the fact that subject’s expectancies regarding ‘performance’ differ. Further as put forth by Pound et al. [47] that if the client is not taking an active role in the post stroke treatment it can reduce the client’s self-determination and sense of control over health. An active role played by client centred task oriented group subjects in deciding goal and activities may lead to higher score in COPM (Performance and Satisfaction).
Gauggel et al. [30] contradicts the efficacy of client- centred approach as it is shown in their study, the effect of goal origin (i.e., self-set vs. assigned) was assessed in a simple arithmetic task. Patients were randomly assigned to one of three conditions: (1) one that set a specific, difficult goal, (2) one that set a “do-your-best” goal, and (3) one in which patients stated their own goal. The results indicate that assigned, difficult goals lead to better performance than assigned easy goals or self-set goals. The reason that participants with self-set goals did not perform better is that they chose only moderately difficult goals, and their actual performance approximated the goal that they had set. These findings indicate that although brain-damaged patients are responsive to goals that they set for themselves, letting patients self-set their performance goals does not always lead to maximal performance.
These findings imply that a client-centred approach in physiotherapy is an effective and a feasible approach as emphasized by Gilbertson et al. [48] in a randomized controlled trial involving 138 subjects from the Glasgow Royal Infirmary, U.K. These findings led to the need for investigating the efficacy of such an intervention in the Indian context. Also convincing results were obtained by Clarke et al. [49]; Corr et al. [50], Drummonds et al. [51] in their earlier trials that stroke survivors can benefit from a client-centred program of physiotherapy.
Clinical implication
Approximately 70% to 80% patients who sustained stroke have upper extremity impairment which can lead to difficulties in daily living and engage in social life. Active involvement of client in goal setting combined with task oriented training will help the patients to enhance the functional recovery of upper extremity in stroke patients and increased functional recovery will in turn improve the quality of life. This treatment can be used clinically as it will be much convenient, safer and easy to perform by the patients and it provides better client satisfaction and performance.
Limitations of the study
Substantial number of patients had to be excluded because of the strict inclusion criteria and the study population is probably not enough to generalize the results. Secondly, these kinds of pragmatic trials cannot be blinded, as the intervention is specific to individual groups.
Third limitation of study is that in earlier studies, the Task oriented training combined with Client centred approach was not used, so there is not much literature to support the findings of this trial. Fourth limitation of the study is that subjects could not be followed up after study.
Future suggestions
Study can be carried out with large sample size. Follow-ups can be done to see long term effects of this training.Study can be replicated by increasing the duration of intervention.
Conclusion
Both task-oriented training and client-centred task oriented training are effective in improving functional recovery of upper limb after stroke. Improvement is more statistically significant in clientcentred task oriented training group only on COPM (performance and satisfaction) but there was no statically difference in upper extremity function in both groups of stroke patients.
References
- Dhamija, Mittal, Bansal (2004) Trends in Clinico- Epidemiological Correlates of Stroke in the Community. Journal of Indian Academy of Clinical Medicine 5:27-31.
- Collin C (1996) Wade. Assessing motor impairment after stroke. J Neurol Neurosurg Psychiatry 49:11-16.
- Barreca S, Wolf S L, Fasoli S, Bohannon R (2003) Treatment interventions for the paretic upper limb of stroke survivors: A critical review. Neurorehabilitation& Neural Repair 17:220-226.
- Sveen U, Bautz-Holter E, Sødring KM, Wyller TB, Laake K (1999) Association between impairments, self-care ability and social activities 1 year after stroke. DisabilRehabil 21: 372-377.
- Yavuzer G, Selles R, Sezer N, Sütbeyaz S, Bussmann JB, et al. (2008) Mirror therapy improves hand function in subacute stroke: a randomized controlled trial. Arch Phys Med Rehabil 89: 393-398.
- Ruth Dickstein, ShragaHocherman, Thomos Pillar, Rachel Shaham (1986) Stroke Rehabilitation: Three Exercise Therapy Approaches. PhysTher66: 1233-1238.
- Kollen BJ, Lennon S, Lyons B, Wheatley-Smith L, Scheper M, et al. (2009) The effectiveness of the Bobath concept in stroke rehabilitation: what is the evidence? Stroke 40: e89-97.
- Kwakkel G, Wagenaar RC, Twisk JW, Lankhorst GJ, Koetsier JC (1999) Intensity of leg and arm training after primary middle-cerebral-artery stroke: a randomised trial. Lancet 354: 191-196.
- Platz T, Eickhof C, van Kaick S, Engel U, Pinkowski C, et al. (2005) Impairment-oriented training or Bobath therapy for severe arm paresis after stroke: a single-blind, multicentre randomized controlled trial. ClinRehabil 19: 714-724.
- Combs SA, Kelly SP, Barton R, Ivaska M, Nowak K (2010) Effects of an intensive, task-specific rehabilitation program for individuals with chronic stroke: a case series. DisabilRehabil 32: 669-678.
- Wolf SL, Winstein CJ, Miller JP, Taub E, Uswatte G, et al. (2006) Effect of constraint-induced movement therapy on upper extremity function 3 to 9 months after stroke: the EXCITE randomized clinical trial. JAMA 296: 2095-2104.
- Page SJ, Levine P, Leonard A (2007) Mental practice in chronic stroke: results of a randomized, placebo-controlled trial. Stroke 38: 1293-1297.
- Glanz M, Klawansky S, Stason W, Berkey C, Shah N, et al. (1995) Biofeedback therapy in poststroke rehabilitation: a meta-analysis of the randomized controlled trials. Arch Phys Med Rehabil 76: 508-515.
- Chae J, Bethoux F, Bohine T, Dobos L, Davis T, et al. (1998) Neuromuscular stimulation for upper extremity motor and functional recovery in acute hemiplegia. Stroke 29: 975-979.
- Gad Alon, Alan F. Levitt, Patricia A. McCarthy (2007) Functional Electrical Stimulation Enhancement of Upper Extremity Functional Recovery during Stroke Rehabilitation: A Pilot Study. Neuro Rehabil Neural Repair 21:207-215.
- Masiero S, Celia A, Rosati G, Armani M (2007) Robotic-assisted rehabilitation of the upper limb after acute stroke. Arch Phys Med Rehabil 88: 142-149.
- Summers JJ, Kagerer FA, Garry MI, Hiraga CY, Loftus A, et al. (2007) Bilateral and unilateral movement training on upper limb function in chronic stroke patients: A TMS study. J Neurol Sci 252: 76-82.
- Ivey FM, Hafer-Macko CE, Macko RF (2008) Task-oriented treadmill exercise training in chronic hemiparetic stroke. J Rehabil Res Dev 45: 249-259.
- Jang SH, Kim YH, Cho SH, Lee JH, Park JW, et al. (2003) Cortical reorganization induced by task-oriented training in chronic hemiplegic stroke patients. Neuroreport 14: 137-141.
- Outermans JC, van Peppen RP, Wittink H, Takken T, Kwakkel G (2010) Effects of a high-intensity task-oriented training on gait performance early after stroke: a pilot study. Clin Rehabil 24: 979-987.
- Schaechter JD (2004) Motor rehabilitation and brain plasticity after hemiparetic stroke. Prog Neurobiol 73: 61-72.
- Gerald V. Smith, Kenneth H. C. Silver, Andrew P. Goldberg, Richard F. Macko (1999) Task-Oriented Exercise Improves Hamstring Strength and Spastic Reflexes in Chronic Stroke Patients. Stroke 30:2112-2118.
- Wade DT (1998) Evidence relating to goal planning in rehabilitation. Clin Rehabil 12: 273-275.
- Wade DT, de Jong BA (2000) Recent advances in rehabilitation. BMJ 320: 1385-1388.
- WhiteneckGG (1994) The 44th annual John Stanley Coulter Lecture. Measuring what matters: key rehabilitation outcomes. Arch Phys Med Rehabil 75: 1073-1076.
- Pollock N (1993) Client-centered assessment. Am J OccupTher 47: 298-301.
- Locke EA, Latham GP (2002) Building a practically useful theory of goal setting and task motivation. A 35-year odyssey. Am Psychol 57: 705-717.
- Mento AJ, Steel RP, Karren RJ (1987) A meta-analytic study of the effects of goal setting on task performance. Organizational Behaviour and Human Decision Processes 39:52-83.
- Wade DT (1998) Evidence relating to goal planning in rehabilitation. Clin Rehabil 12: 273-275.
- Gauggel S, Hoop M, Werner K (2002) Assigned versus self-set goals and their impact on the performance of brain-damaged patients. J Clin ExpNeuropsychol 24: 1070-1080.
- Guilcher S, Lee J, Prosperi C, Winter J, Rosenthal T (2003)The investigation of rehabilitation program differences in client-centeredness using the Client Centred Rehabilitation Questionnaire. Toronto (ON).
- Cott CA (2004) Client-centred rehabilitation: client perspectives. Disabil Rehabil 26: 1411-1422.
- Carroll D (1965) A Quantitative Test of Upper Extremity Function. J Chronic Dis 18: 479-491.
- Rabadi MH, Rabadi FM (2006) Comparison of the action research arm test and the Fugl-Meyer assessment as measures of upper-extremity motor weakness after stroke. Arch Phys Med Rehabil 87: 962-966.
- Van der Lee JH, De Groot V, Beckerman H, Wagenaar RC, Lankhorst GJ, et al. (2001) The intra- and interrater reliability of the action research arm test: a practical test of upper extremity function in patients with stroke. Arch Phys Med Rehabil 82: 14-19.
- Lang CE, Wagner JM, Dromerick AW, Edwards DF (2006) Measurement of upper-extremity function early after stroke: properties of the action research arm test. Arch Phys Med Rehabil 87: 1605-1610.
- Cup EHC, Scholte op Reimer WJM, Thijssen MCE, vanKuyk-Minis MAH (2003) Reliability and validity of the Canadian occupational performance measure in stroke patients. Clinical Rehabilitation 17:402-409.
- Dedding C, Cardol M, Eyssen IC, Dekker J, Beelen A (2004) Validity of the Canadian Occupational Performance Measure: a client-centred outcome measurement. ClinRehabil 18: 660-667.
- Eyssen IC, Beelen A, Dedding C, Cardol M, Dekker J (2005) The reproducibility of the Canadian Occupational Performance Measure. ClinRehabil 19: 888-894.
- Verkerk GJ, Wolf MJ, Louwers AM, Meester-Delver A, Nollet F (2006) The reproducibility and validity of the Canadian Occupational Performance Measure in parents of children with disabilities. ClinRehabil 20: 980-988.
- Blennerhassett J, Dite W (2004) Additional task-related practice improves mobility and upper limb function early after stroke: a randomised controlled trial. Aust J Physiother 50: 219-224.
- Higgins J, Salbach NM, Wood-Dauphinee S, Richards CL, Côté R, et al. (2006) The effect of a task-oriented intervention on arm function in people with stroke: a randomized controlled trial. ClinRehabil 20: 296-310.
- LiepertJ, Graef S, Uhde I, Leidner O, Weiller C (2000) Training-induced changes of motor cortex representations in stroke patients. ActaNeurolScand 101: 321-326.
- Jang SH, Kim YH, Cho SH, Lee JH, Park JW, et al. (2003) Cortical reorganization induced by task-oriented training in chronic hemiplegic stroke patients. Neuroreport 14: 137-141.
- Shumway Cook A, Woolcott MH. Motor Control- Translating Research into Clinical Practice. 4th edition 2011.
- Bodiam, Carolyn (1999)he Use of the Canadian Occupational Performance Measure for the Assessment of Outcome on a Neurorehabilitation Unit. The British Journal of Occupational Therapy 62:123-126.
- Pound P, Bury M, Gompertz P, Ebrahim S (1994) Views of survivors of stroke on benefits of physiotherapy. Qual Health Care 3: 69-74.
- Gilbertson, Louise, Langhorne, Peter (2000) Home-Based Occupational Therapy: Stroke Patients' Satisfaction with Occupational Performance and Service Provision. The British Journal of Occupational Therapy 63:464-468.
- PA Clarke, H. Collins, Jrf. Gladman (1995) Occupational therapy for stroke patients at home. ClinRehabil 9:91-96.
- Susan Corr, Antony Bayer (1995) Occupational therapy for stroke patients after hospital discharge — a randomized controlled trial. ClinRehabil 9:291-296.
- Aer Drummond, MF Walker (1995) A randomized controlled trial of leisure rehabilitation after stroke. ClinRehabil 9:283-290.
Citation: Kumar C, Gupta N (2015) A Comparison between Task Oriented and Client-Centred Task-Oriented Approaches to Improve Upper Limb Functioning in People with Sub-Acute Stroke. J Nov Physiother 5: 276 DOI: 10.4172/2165-7025.1000276
Copyright: © 2015 Kumar C, et al. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.
Share This Article
Recommended Journals
Open Access Journals
Article Tools
Article Usage
- Total views: 23974
- [From(publication date): 10-2015 - Apr 02, 2025]
- Breakdown by view type
- HTML page views: 18883
- PDF downloads: 5091