A Clinical Study of a Woman with Chronic Vaginal Hemorrhaging
Received: 05-Jan-2023 / Manuscript No. jhcpn-23-85641 / Editor assigned: 07-Jan-2023 / PreQC No. jhcpn-23-85641 / Reviewed: 21-Jan-2023 / QC No. jhcpn-23-85641 / Revised: 23-Jan-2023 / Manuscript No. jhcpn-23-85641 / Accepted Date: 29-Jan-2023 / Published Date: 30-Jan-2023 QI No. / jhcpn-23-85641
Abstract
Background: Umbilical discharge in an adult is uncommon and raises a wide range of diagnostic questions. Due to inherited disease such umbilical hernias and congenital anomalies, umbilical anatomy varies. Endometriosis or primary or metastatic cancer may spread to the umbilicus.
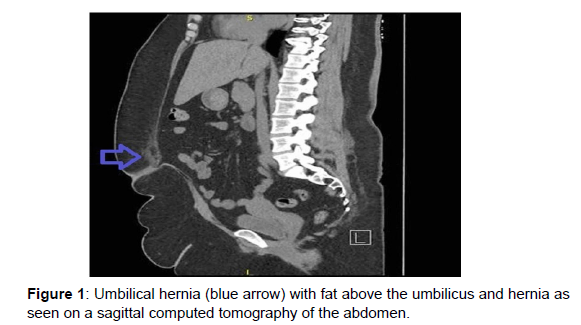
Present a case: A white American woman in her 40s who had been experiencing spontaneous umbilical bleeding for two days arrived at the clinic. Her periumbilical pain was accompanied by emesis and nausea. There were no skin abnormalities that could be seen, but a deep abdominal probing revealed a thin, watery serosanguineous fluid coming from the umbilicus. Five years before, she had a similar episode of unexplained umbilical haemorrhage. The results of the laboratory workup showed a slightly increased C-reactive protein. A full surgical excision of the umbilicus was required due to a fat-containing umbilical hernia with fat necrosis discovered by computed tomography imaging.
Conclusions: Adults with umbilical discharge should be evaluated for a rare disorder called an umbilical hernia with fat necrosis. Adults with spontaneous umbilical bleeding or discharge should also be evaluated for embryonal remains,omphalitis, and metastases as additional diagnostic possibilities. If the physical examination does not immediately reveal the cause, computed tomography imaging should be considered to check for hernias and embryonic defects.
Keywords
Umbilical; Abdominal hernias; Discharge
Introduction
The uncommon occurrence of spontaneous umbilical discharge in an adult patient raises a variety of diagnostic issues, including abdominal hernias, underlying medical problems, infections, and foreign bodies. The differential in the case of spontaneous umbilical bleeding in an adult patient is even more limited, and there is little research on the subject. Reported a case of incarcerated umbilical hernia with omental varices causing umbilical haemorrhage due to portal hypertension. a case of an umbilical nodule that was bleeding because of cutaneous endometriosis.
Present a case
A 40-year-old white American lady with nontraumatic umbilical haemorrhage who woke up to find her shirt saturated in blood from her umbilicus sought treatment from a primary care physician. She was able to halt the bleeding by applying pressure with a towel. The patient's intermittent umbilical bleeding and nonradiating periumbilical pain persisted, both of which were aggravated by movement and accompanied by nausea and emesis. Her umbilicus had been [1-3] occasionally cleaned in the shower with a cotton swab and peroxide; this occasionally left small spots of blood on the cotton swab. She (Figure 1) had been visited for non-painful umbilical haemorrhage five years earlier. She was given bacitracin and instructed to apply Vaseline for what was thought to be a minor irritation at the time; imaging was not done. She stopped using a cotton swab to wipe her umbilicus because she had no intermediate symptoms. Past medical history included significant depression, generalised anxiety disorder, class III obesity with a BMI of 45, hypertension, gastroesophageal reflux disease, etc. Patient's G1P1001 code. Only an elective caesarean section 12 years prior without difficulties stood out in the patient's surgical history.
Materials and Method
The patient worked in retail and was divorced. She didn't smoke, use illegal substances, or consume alcohol. Diabetes, Crohn's disease, diverticulitis, as well as breast, lung, and prostate cancer, ran in the family. The patient was taking a number of long-term prescription drugs, such as losartan 50 mg tablet by mouth daily, propranolol 60 mg tablet by mouth twice daily, escitalopram 20 mg tablet by mouth daily, bupropion 450 mg tablet by mouth daily, gabapentin 300 mg capsule by mouth three times daily, norethindrone-ethinyl estradiol 1 mg-35 g tablet by mouth daily, trazodone 100 mg. The patient had a pulse rate of 65 beats per minute and a blood pressure reading of 125/81 mmHg on the day of the presentation. She was unresponsive. A non-distended abdomen and entirely normal skin without erythema, fissures, or apparent discharge were discovered upon closer inspection, however there was some dried blood. Deep palpation revealed slight periumbilical discomfort. Deep palpation around the umbilicus resulted in the immediate release of a thin, watery, serosanguinous fluid.
The rest of the physical examination included tests for the heart, lungs, and nervous [4-7] system, all of which came back clean. The patient was submitted for a CT scan of the abdomen and pelvis the same day, which showed a tiny umbilical hernia containing fat and possibly a small region of necrosis directly above the hernia. A slightly higher high-sensitivity CRP of 13.8 during the laboratory workup was noteworthy. Complete blood count (CBC) with differential, electrolytes, renal function, and liver function were among the other lab tests that came back within normal ranges. The parameters of coagulation were not examined. The patient had an umbilectomy with open wound packing and an outpatient open umbilical hernia repair without mesh four weeks later. A 4.2 by 3.5 by 2.6 cm specimen with the hernia sac and urachal remains was removed and sent for pathologic analysis after the fascia was dissected down to. Since there was little reason to suspect infection, no cultures were submitted. At the 30-day postoperative checkup, all of her symptoms and bleeding had disappeared completely. She didn't get any prescription drugs for this ailment, including antibiotics. The results of the surgical pathology analysis included granulation tissue, suture material from a foreign body, ulcerated skin with abscess, and umbilical remnant. The patient denied experiencing any discomfort, nauseousness, or vomiting at the 1-month and 2-month wound check visits. When checked again six months after the surgery, the patient was still doing well and her symptoms hadn't returned.
Discussion& Result
To our knowledge, this case represents an uncommon manifestation of an umbilical hernia that resulted in spontaneous bleeding from the umbilicus. The diagnostic options are varied when an adult patient experiences spontaneous umbilical discharge. Other case reports have described disorders connected to embryologic features, such as mullerianosis and umbilical sinus communicating with peritonitis, and infections brought on by foreign bodies. Umbilical hernia with portal hypertension, rupture of umbilical varices resulting from recanalized umbilical and periumbilical veins, or contact between underlying omental varices and abdominal wall scars can all be potentially fatal causes of bleeding. Although CT imaging in our patient showed an umbilical hernia, there was no cirrhosis or any aberrant vasculature that may have suggested an umbilical varices rupture. Even though our patient's pathology did not reveal endometrial tissue [7-9] or malignancy, endometriosis with umbilical implantation and primary cancer or metastases could nonetheless result in bleeding. Our patient had a history of cleaning her umbilicus with a cotton swab, which might have led to an omphalitis brought on by a foreign body. A case of omphalitis brought on by an impacted lint ball was previously described by Sarma et al. Five years ago, our patient's first episode of umbilical haemorrhage may have been brought on by a similar foreign body, with obesity and a deep umbilicus acting as risk factors. Her second incidence of umbilical haemorrhage was not brought on by a triggering incident, and a physical examination turned up no foreign bodies or skin inflammation. The bleeding is assumed to have been spontaneous because there was no apparent cause. Only a higher BMI was a risk factor for umbilical hernia in the patient. It was unable to verify the source of the foreign suture body material reported on the pathology report, although it most likely represents an unintentional finding from the patient's previous C-section.
Conclusion
Umbilical discharge is a rare disorder that can be brought on by a variety of pathologies that vary in severity. When creating a differential diagnosis, one should take an umbilical hernia with fat necrosis into account.
Acknowledgement
We appreciate the staff at Hospital Pacifica Salud for helping to manage and support this case report.
Declaration of conflicting interests
No potential conflicts of interest were disclosed by the author(s) with regard to the research, writing, or publication of this paper.
Ethical approval
For reporting individual instances or case series, our institution does not require ethical approval.
References
- Ahmad S, Campos MG, Fratini F, Altaye SZ (2020) New insights into the biological and pharmaceutical properties of royal jelly. Int J Mol Sci 21: 382
- Chan GCF, Cheung KW, Sze DMY (2013) The immunomodulatory and anticancer properties of propolis. Clinical reviews in allergy 44:262-73
- Król W, Bankova V, Sforcin JM, Szliszka E, Czuba Z, et al. (2013) Propolis: properties, application, and its potential. Evidence-Based Complementary and Alternative Medicine.
- Khazaei M, Ansarian A, Ghanbari E (2018) New findings on biological actions and clinical applications of royal jelly: a review. J Diet Suppl 15: 757-775.
- Kocot J, Kiełczykowska M, Luchowska-Kocot D, Kurzepa J, Musik I (2018) Antioxidant potential of propolis, bee pollen, and royal jelly: possible medical application. Oxidative medicine and cellular longevity .
- Marcucci MC (1995) Propolis: chemical composition, biological properties and therapeutic activity. Apidologie 26: 83-99.
- Mishima S, Suzuki KM, Isohama Y, Kuratsu N, Araki Y, et al. (2005) Royal jelly has estrogenic effects in vitro and in vivo. Journal of ethnopharmacology 101: 215-220.
- Oryan A, Alemzadeh E, Moshiri A (2018) Potential role of propolis in wound healing: Biological properties and therapeutic activities. Biomedicine & pharmacotherapy 98: 469-483.
- De Groot AC (2013) Propolis: a review of properties, applications, chemical composition, contact allergy, and other adverse effects. Dermatitis 24: 263-282.
Indexed at, Google Scholar, Crossref
Indexed at, Google Scholar, Crossref
Indexed at, Google Scholar, Crossref
Indexed at, Google Scholar, Crossref
Indexed at, Google Scholar, Crossref
Indexed at, Google Scholar, Crossref
Indexed at, Google Scholar, Crossref
Citation: Hun Y (2023) A Clinical Study of a Woman with Chronic VaginalHemorrhaging. J Health Care Prev, 6: 182.
Copyright: © 2023 Hun Y. This is an open-access article distributed under theterms of the Creative Commons Attribution License, which permits unrestricteduse, distribution, and reproduction in any medium, provided the original author andsource are credited.
Share This Article
Recommended Journals
Open Access Journals
Article Usage
- Total views: 752
- [From(publication date): 0-2023 - Feb 23, 2025]
- Breakdown by view type
- HTML page views: 564
- PDF downloads: 188