A Case Report: Primary Sacral Hydatidosis and Literature Review
Received: 04-Apr-2022 / Manuscript No. roa-22-roa-22-61294 / Editor assigned: 06-Apr-2022 / PreQC No. roa-22-61294 (PQ) / Reviewed: 17-Apr-2022 / QC No. roa-22-61294 / Revised: 23-Apr-2022 / Manuscript No. roa-22-61294 (R) / Published Date: 30-Apr-2022 DOI: 10.4172/2167-7964.1000375
Abstract
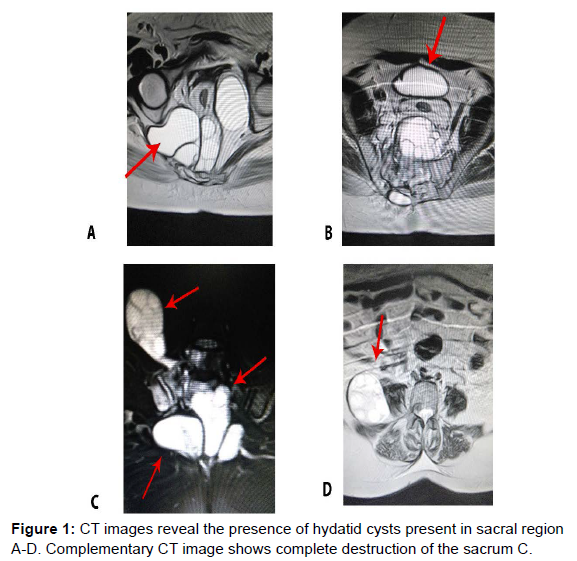
Echinococcus granulosis is a zoonotic parasite that is the major cause of hydatid cyst or commonly called hydatidosis. Liver and lungs are the primary site where hydatidosis pathology becomes prominent. In rare cases involvement of bone is less commonly diagnosed or reported. Here in this report we present a case of sacral hydatidosis in a female patient presenting with hyrestectomy and histopathology revealed cervicitis, adenomyosis, and leiomyoma. Beside these interventions she was not improving, follow-up ultrasound was done and it was found that multioculated cystic lesions in pelvis, one in presacral region and another in RIF close to psoas muscle this lesion in RIF was connected to the presacral lesion through a narrow pedicle. Complementary CT was done and it revealed that presacral lesion has invaded and destroyed the sacrum with intra spinal extension.
Keywords
Computed tomography; Right Illiac Fossa
Introduction
Tape worm, dog tape worm or hydatid worm also known as Echinococcus granulosus is a zoonotic parasite that penetrate into small intestines of animals, which then passes on to the intermediate host (such as livestock and humans) via stool. The life cycle of E. granulosus include dogs and wild animals as a definitive host for the adult tapeworm where parasites become mature and reproduce. Half of its life cycle completes in zoonotic animals and half occurs in intermediate host. The larval stage begins in intermediate host which results in echinococcal cysts [1, 2]. Though these cysts are slow growing but can cause serious clinical complications involving lungs, liver, skeleton (0.5-2%) and 50% of which involves spine. The infestation of Hydatid cyst occur by direct extension from pulmonary or pelvic region, spinal hydatid cyst manifest itself in thoracic region more commonly than lumber region, beside these infestations, sacral hydatid cysts which rarely presents in clinical settings are missed by most of the clinicians due to differential list of paralysis and rarity of the disease presentation [3].
Sacral hydatidosis in most of the cases are misdiagnosed in early stages, due to its chronicity and without any significant clinical manifestation. This eventually ends with loss of bone and destruction of the surrounding tissue [4]. Sacral hydatid disease should be highlighted as a differential when cystic lesion of the sacrum is experienced. We present an extremely rare case of sacral hydatid cyst. Osteolysis is usually seen sometimes related with expansion of the bone [4, 5].Case Presentation
A 50 years old female presented to us with low backache and lower limbs pain for last 5 years, previously she had hysterectomy and histopathology revealed cervicitis, adenomyosis, and leiomyoma. Her clinical symptoms did not improved as a result follow up ultrasound revealed multiloculated cystic lesions in pelvis, one in presacral region and another in RIF close to psoas muscle. This lesion in RIF was connected to the presacral lesion through a narrow pedicle. The presacral lesion has invaded and destroyed the sacrum (Figure 1) with intraspinal extension. The complementary CT images revealed almost complete destruction of the sacrum (Figure 1).
Discussion
Till date in most of the reported cases the primary source of Hydatid cyst is liver and lungs [6]. Involvement of other organs especially lumber region is very rare. Neither surgical intervention nor medical treatment is generally effective for hydatid cyst of bone or more specifically sacrum. Presurgical use of albendazole is the drug of choice against the sporadic echinococcus infestations or it can reduce the risk of recurrence [7-9].
Conclusion
Till date five cases of hydatid cysts are reported which is associated with sacrum [2, 3, 9, 11-13]. Patient with symptoms such as sciatica, accompanied with lower backache, and with lower limb must be correlated with hydatid cyst confirm through CT scan combine with MRI, and it should be included in a differential diagnosis when such cases are encountered. A complete clinical history of the patient is a gold standard in radiological findings of such disease.
Acknowledgement
The authors are deeply grateful to the participants whose time and effort made this study possible. We also appreciate the patients for their willingness and providing us the history. We also acknowledge the Department of Radiology and its technical staff who provided us the CT and MRI films.
Conflicts of Interest
None
References
- Abbassioun K, Amirjamshidi A (2001) Diagnosis and management of hydatid cyst of the central nervous system: Part 2: Hydatid cysts of the skull, orbit, and spine. Neuro Quart 11: 10-16.
- Abdelhakim K, Khalil A, Haroune B, Oubaid M, Mondher M (2014) A case of sacral hydatid cyst. Int J Surg Case Rep 5: 434-436.
- Agnihotri M, Goel N, ShenoyA, Rai S, Goel A (2017) Hydatid disease of the spine: A rare case. J Craniovertebr Junction Spine 8: 159-160.
- Bhake A, Agrawal A (2010) Hydatid disease of the spine. J Neurosci Rural Pract 1: 61-62.
- Eckert J, Deplazes P (2004) "Biological, epidemiological, and clinical aspects of echinococcosis, a zoonosis of increasing concern." Clin Microbiol Rev 17: 107-135.
- Ergin A, Toker T, Yanarates O, Kurt E, Guzeldemir ME (2007) A typical low-back pain caused by an atypical etiology. Reg Anesth Pain Med 32: 89-92.
- Layadi F, Boubrik M, Ait El Qadi A, Ait Benali S (2005) Primary sacral epidural hydatid cyst: A case report. J Radiol 86: 1040-1042.
- Ndondo AP, Fieggen G, Wilmshurst JM (2003) Hydatid disease of the spine in South African children. J Child Neurol 18: 343-346.
- Patel D, Shukla D (2010) back bugged: A case of sacral hydatid cyst. J Neurosci Rural Pract 1: 43-45.
- Moro P, Schantz PM (2009) Echinococcosis: a review. Int J Infect Dis 13: 125-133.
- Singh S, korah Ip, Gibikote SV, Shyam NK, Nair A, et al. (1998) Sacral hydatidosis: value of MRI in the diagnosis. Skeleton Radio 27: 518-521.
- Unal VM, Ozdemir N, Karadag A, Oguzoglu S, Celik H (2017) Primary Sacral Hydatid Cyst Causing Cutaneous Fistula. J coll Physicians Surg Pak 27: 311-312.
- Yilmaz N, Ozgocmen S, Kocakoc E, Kiris A (2004) Primary hydatid disease of sacrum affecting the sacroiliac joint: A case report. Spine (Phila Pa 1976) 29: E88-90.
Indexed at,Google Scholar,Crossref
Indexed at,Google Scholar,Crossref
Indexed at,Google Scholar,Crossref
Indexed at,Google Scholar,Crossref
Indexed at,Google Scholar,Crossref
Indexed at,Google Scholar,Crossref
Indexed at,Google Scholar,Crossref
Indexed at,Google Scholar,Crossref
Indexed at,Google Scholar,Crossref
Citation: Begum T, Khan V, Janan Z (2022) A Case Report: Primary Sacral Hydatidosis and Literature Review. OMICS J Radiol 11: 375. DOI: 10.4172/2167-7964.1000375
Copyright: © 2022 Begum T, et al. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.
Share This Article
Open Access Journals
Article Tools
Article Usage
- Total views: 1509
- [From(publication date): 0-2022 - Feb 22, 2025]
- Breakdown by view type
- HTML page views: 1154
- PDF downloads: 355