A Case Report on Post-Operative Intussusceptions in Adult
Received: 17-Mar-2018 / Accepted Date: 26-Mar-2018 / Published Date: 03-Apr-2018 DOI: 10.4172/2161-069X.1000559
Abstract
Intussusception is the prolapse of one part of the bowel into the lumen of the immediately adjoining part. Intussusceptions in adults are much less common, representing 5% of all intussusceptions, 1% of all bowel obstructions, and 0.08% of all abdominal surgery. Surgery as a possible cause of intussusceptions in children is very rare (0.05%) and in adult, there are very few reports. In a report in a mayo clinic only 73 cases were seen within 23 year. This case report will be one of the few case reports on the subject matter. This is a 30 year old female from rural areas who underwent laparotomy and cystectomy for the diagnosis of left side ovarian cystic torsion after she presented with right side abdominal pain of sixth days duration which was squeezing in type. On the fourth post-operative day she started to have abdominal distention, and vomiting which was non projectile bilious matter 4-5 times/day. She came after 4 days of these symptoms with failure to pass both feces and flatus. On the day of admission she has 3-4 episodes of watery diarrhea which was blood tingled. Physical examination she was acutely sick looking and dehydrated. Abdominally she has centrally distended abdomen with palpable bowel loops and visible peristalsis. We investigated her with abdominal X-ray and ultrasound which suggested SBO 2ry to intussusceptions. After stabilizing the patient we did laparotomy. Intraoperativly we found viable ileo- ileal intussusceptions at two sites with distended bowel loops proximal and collapsed bowel loops distal to the intussusceptions. She had smooth post op course and discharged improved. The case is extremely important for the study of this possible differential in post-operative period because a delayed or incorrect diagnosis of acute intussusceptions can have serious consequences. Moreover it serves as an input for future studies in the area.
Keywords: Intussusceptions; Post-operative intussusceptions; Ovarian cyst; Ovarian cystic torsion; Cystectomy; Ileo-ileal intussusceptions
Abbreviation
PR-per-rectal; PO-per-os; UOG-University of Gondar; SBO-small bowel obstruction
Background
Intussusceptions, which are defined by Treves in 1899, as the prolapse of one part of the bowel into the lumen of the immediately adjoining part, drawing the proximal bowel into the distal bowel by peristaltic activity. It was first reported in 1674 by Barbette of Amsterdam. Two hundred years later, Sir Jonathan Hutchinson performed the first successful operation on a child with this condition in 1871 [1]. Intestinal intussusceptions in adult are a rare entity that differs greatly in etiology from its pediatric counterpart [2] with an incidence of 1.5-4 cases per 1000 livebirths [3]. Intussusceptions in adults are much less common, representing 5% of all intussusceptions, 1% of all bowel obstructions, and 0.08% of all abdominal surgery and 0.003–0.02% of all hospital admissions (Figure 1). The overall incidence of intussusceptions in adulthood has been estimated to be around 2–3 cases/1,000,000 population/year [4,5]. Most of the cause of intussusceptions is idiopathic in children (95%), whereas 80–90% of intussusceptions in adults have identifiable etiology [6]. Surgery as a possible cause of intussusceptions in children is very rare (0.05%) and in adults, as to my knowledge, there are very few reports.
This group of patient will not have those classic triads of intussusceptions (abdominal mass, abdominal pain and bloody stool) which make it very difficult for physician to diagnose it early [7]. This case report will be one of the few case reports on the subject matter. The case is extremely important for the study of this possible differential in post-operative period because a delayed or incorrect diagnosis of acute intussusceptions can have serious consequences. Moreover it serves as an input for future studies in the area.
Case Presentation
History
This is a 30-year-old Para three all alive mother from rural areas. She initially underwent laparotomy and cystectomy for the diagnosis of left side ovarian cystic torsion after she presented with right side abdominal pain of sixth days duration which was squeezing in type. On the second post-operative day she was discharged improved. On the fourth post-operative day she started to have abdominal distention, and vomiting which was non projectile bilious matter 4-5 times/day. She came after 4 days of these symptoms with failure to pass both feces and flatus. On the day of admission she has 3-4 episodes of watery diarrhea which was blood tingled [8].
Physical examination
General appearance: Acutely sick looking dehydrated.
Vital sign: BP-110/70, PR-90, RR-18, T-36.7.
HEENT: Pink conjunctiva, dry oral mucosa.
Chest: Clear and resonant.
CVS: S1 and S2 well heard. No murmur or gallop.
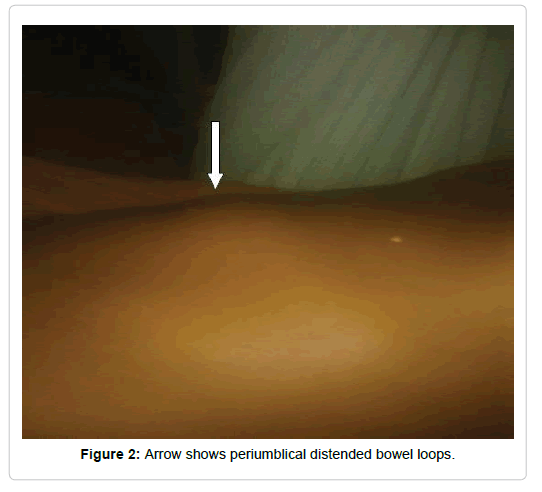
Abdomen: Central distention, flanks are full, pfannestial incision wound and visible peristalsis.
Non tender, boggy mass over the periumlical area (Figure 2).
PR: Watery stool on examining finger.
Investigation: Initial admission
Laboratory:
Full blood count: WBC- 3.73
HCT- 42.8
PLT- 196
Stool examination:
No O/P seen
Urine HCG: negative
BG/Rh: o+
Imaging:
Abdominal ultrasound
Liver gall bladder spleen pancreas appears normal.
Both kidneys have normal size and echo pattern.
Normal UB and uterus.
Normal looking bowel and appendix.
A thin walled cyst at the left adnexa 4.2 × 3.2 cm.
Second admission
Laboratory: Serum electrolyte-Na: 143, K: 3.7, Cl: 104.5, M.HCT: 38%, S/M: full of RBCs and bacteria.
Imaging
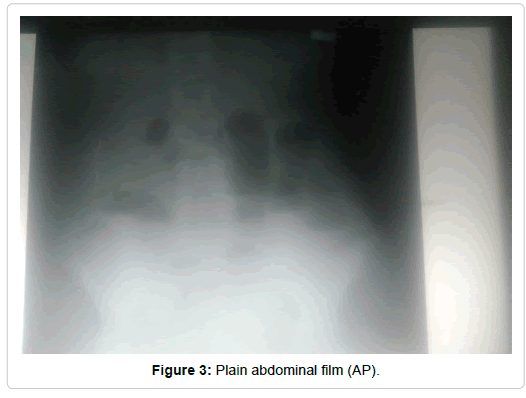
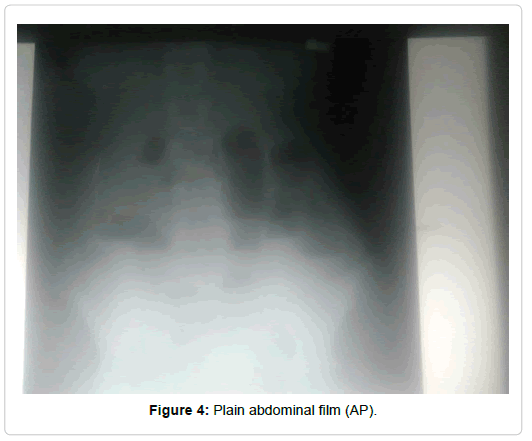
Plain abdominal X-ray: multiple air-fluid level in central abdomen with mildly dilated bowel loops (3.5 cm), rectal gas shadow seen (Figures 3 and 4).
Abdominal ultrasound: liver gall bladder, spleen, pancreas UB and Uterus appear normal. Both kidneys have normal size and echo pattern. There is a bowel in bowel pattern likely ilea-colic intussusceptions with normal Doppler flow within the wall. Minimal fluid collection in the pelvis with no septation or echo debris. No adnexal mass seen.
Diagnosis and Management
With the diagnosis of SBO 2ry to ileocolic intussusceptions she was admitted. IV line secured and resuscitated with normal saline. NG-tube inserted, catheterized and she was kept NPO, prophylactic antibiotics given. After taking an informed consent with the above preoperative diagnosis we did laparotomy through midline incision [9].
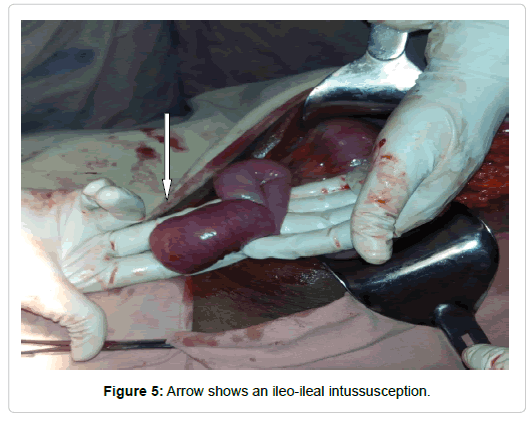
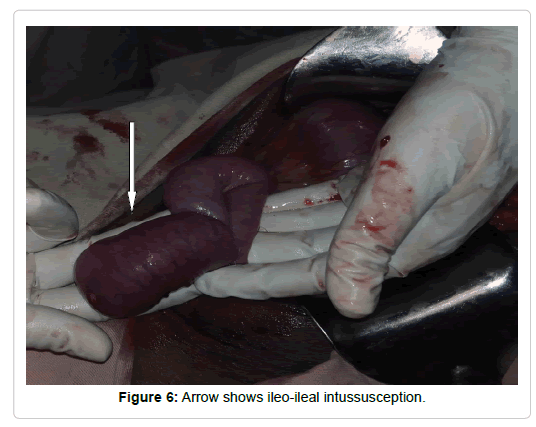
IOF
300 cc reactive fluid all over the peritoneal cavity. A viable Ileo ileal intussusceptions (around 10 cm of proximal bowel invaginated in to the distal bowel lumen) around 200 cm distal to the ligament of Trietz with proximal small bowel dilatation and distal small bowel collapse (Figures 5 and 6).
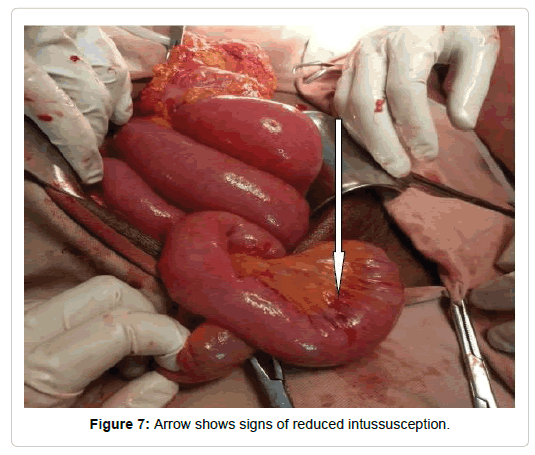
Another site, around 50 cm distal to the proximal intussusceptions site, reduced ileoileal intussusceptions with contused bowel wall and mesentery (Figure 7). All other viscera’s looks grossly normal.
Done
Reactive peritoneal fluid sucked out.
Ileo-Ileal intussusceptions reduced manually
Peritoneal cavity washed with warm normal saline, abdomen closed in layer.
Post-operative course
She was kept NPO, given analgesics regularly, we encouraged her ambulation. On her first post op day she passed flatus, bowel sounds were active and we started her on PO feeding. She was followed with vital sign sheet and abdominal examination. On her 2nd post op day she started to have watery diarrhea for which she was investigated but none were revealing. We put her on ORS, dewormed her and on her 4th post op day she got improved and discharged with an appointment to follow up clinic.
Discussion and Conclusion
Intussusceptions, which are defined by Treves in 1899, as the prolapse of one part of the bowel into the lumen of the immediately adjoining part, drawing the proximal bowel into the distal bowel by peristaltic activity. It was first reported in 1674 by Barbette of Amsterdam. Two hundred years later, Sir Jonathan Hutchinson performed the first successful operation on a child with this condition in 1871. Intestinal intussusceptions in the adult are a rare entity that differs greatly in etiology from its pediatric counterpart with an incidence of 1.5-4 cases per 1000 livebirths. Intussusceptions in adults are much less common, representing 5% of all intussusceptions, 1% of all bowel obstructions, and 0.08% of all abdominal surgery and 0.003–0.02% of all hospital admissions. The overall incidence of intussusceptions in adulthood has been estimated to be around 2–3 cases/1,000,000 population/year. Most of the cause of intussusceptions is idiopathic in children (95%), whereas 80–90% of intussusceptions in adults have identifiable etiology. Surgery as a possible cause of intussusceptions in children is very rare (0.05%) and in adults, there are very few reports. This one will be the first to be reported in our institution.
Postoperative intestinal obstruction usually occurs due to ileus, post op adhesion, volvulus and post-operative intussusceptions being the rare cause (accounting for 5-10% of post-operative bowel obstruction in children). Some of the possible Factors that may be related to postoperative intussusceptions are altered peristalsis and vigorous intestinal manipulation, intestinal injury, foreign body, or neurogenic factors. The vast majority of cases are small bowel intussusceptions, accounting for up to 87.2%, with the majority ileoileal, followed by jejunojejunal. Ileocolic intussusceptions are present in up to 12.8% of reported cases. In our case it is ileo-ileal intussusceptions.
Post-operative intussusceptions remains a diagnostic challenge to physicians, and is often overlooked due to its rarity as a complication and nonspecific symptoms, which may mimic a postoperative ileus. In our case we faced diagnostic difficulty because we ascribed the symptoms for post-operative ileus. Abdominal pain may be masked by pain medication. An abdominal mass may be difficult to palpate due to the laparotomy incision and its associated tenderness. Rectal bleeding rarely occurs. In postoperative intussusceptions, abdominal distention and increased bilious drainage from Nasogastric tube are most common signs. Abdominal pain is less common. The majority of patients, up to 90%, present within the first two weeks following surgery. In our case she had diarrhea with blood tingled, abdominal distention and vomiting but no abdominal pain. And she presented after 4 days of operation.
Because of its rarity as a possible cause of post-operative bowel obstruction, most of the patients will be diagnosed lately.
The majority of postoperative obstructions result from intestinal adhesions, but the possibility of intestinal intussusceptions should not be overlooked. Clinical signs and symptoms of postoperative intussusceptions are nonspecific; therefore, abdominal plain films and laboratory data are of little diagnostic value in these cases. However, ultrasound and computed tomography are capable of delineating the features of intestinal intussusceptions. Clinicians should be aware of this uncommon complication in children in the early postoperative period.
The management options depend on the site of intussusceptions and presence of complication related with intussusceptions.
Postoperative intussusceptions should be suspected in adult surgical patients who showed signs of intestinal obstruction in the early postoperative period. Awareness and early diagnosis are key to reducing the morbidity associated with postoperative intussusceptions.
The clinical symptoms of postoperative ileoileal intussusceptions after operations are not typical. Postoperative (ileoileal) intussusceptions should be kept in mind in a patient with post-operative obstruction in adults. In any atypical postoperative ileus, a sonographic study should be done to rule out the diagnosis of postoperative intussusceptions. Once this condition is diagnosed, surgical treatment should be performed as soon as possible.
Ethical Approval
Not applicable
Consent for Publication
Taken from the patient and you can access it from the authors
Availability of Data and Materials
The datasets generated during and/or analyzed during the current study are available from the corresponding author on reasonable request. The full data is available on chart number-721049, Gondar university hospital, Gondar, Ethiopia.
Authors Contribution
Yitagesu Aberra, author of this case report, is a senior resident (chief resident) in the department of surgery, UOG, Who was the leading surgeon in the management of this patient.
Acknowledgment
I would like to thank the department of surgery and gynecology and obstetrics who did a lot in the management of this patient. My kind gratitude goes to the OR nurses and anesthetist above all my assistant Surgeon Dr.Meron Birhanu for their good did and active participation.
Author’s Information
Dr. Yitagesu Aberra is a final year surgical resident in the department of surgery, UOG, Gondar, Ethiopia. He is a graduate from Gondar University and worked as a general practitioner for two Years in the same University hospital. He is currently practicing surgery in Gondar University Hospital.
References
- Sarma D, Prabhu R, Rodrigues G (2012) Adult intussusception: A six-year experience at a single center. Ann Gastroenterol 25: 128–132.
- Eisen LK, Cunningham JD, Aufuses AH (1999) Intussusception in adults: Institutional review. J Am Coll Surg 188: 390–395.
- Huang WS, Changchien CS, Lu SN (2000) Adult intussusception: A 12-year experience, with emphasis on etiology and analysis of risk factors. Chang Gung Med J 23: 284–290.
- Mandal S, Kawatra V, Dhingra KK (2010) Lipomatous polyp presenting with intestinal intussusception in adults: report of four cases. Gastroenterol Res 3: 229–231.
- Mollitt DL, Ballantine TV, Grosfeld JL (1979) Postoperative intussusception in infancy and childhood: Analysis of 119 cases. Surgery 86: 402-408.
- Doody DP (1997) Intussusception: Surgery of infant and children. [1 Edn] Philadelphia Lippincott-Raven Company, 1247-1248.
- Yang G, Wang X, Jiang W, Ma J, Zhao J, et al. (2013) Postoperative intussusceptions in children and infants: a systematic review. Pediatr Surg Int 29: 1273-1279.
- Bai YZ, Chen H, Wang WL (2009) A special type of postoperative intussusception: Ileoileal intussusception after surgical reduction of ileocolic intussusception in infants and children. J Pediatr Surg 44: 755-788.
Citation: Aberra Y (2017) A Case Report on Post-Operative Intussusceptions in Adult. J Gastroint Dig Syst 8: 559. DOI: 10.4172/2161-069X.1000559
Copyright: © 2017 Aberra Y. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.
Share This Article
Recommended Journals
Open Access Journals
Article Tools
Article Usage
- Total views: 6053
- [From(publication date): 0-2018 - Dec 19, 2024]
- Breakdown by view type
- HTML page views: 5323
- PDF downloads: 730