A Case Report on Duplex Appendix in a Patient with Ileocolocolic Intussusceptions
Received: 22-Nov-2017 / Accepted Date: 27-Nov-2017 / Published Date: 28-Nov-2017 DOI: 10.4172/2161-069X.1000538
Abstract
Duplex cecal appendix is a rare anatomical variation. Approximately 100 cases of double cecal appendix have been described so far. Till now there is no report of duplex appendix serving as a lead point in a patient with intussusceptions. This case report presents the first case of such presentation for the first time. This 6 month old female child presented with vomiting and diarrhea of week duration. She was tachycaridic, tachypniec and febrile. On abdominal examination she had distended and tender abdomen with hyper tympanic sound on percussion. She was irritable and had a sunken eye ball. She had leaukocytosis (20.8 × 103), hypokalemia (3.3 mmol/l) and hyponatremia (125 mmol/l). Abdominal ultrasounds were suggestive of intussusception. After stabilizing the patient we operated her for possible pre-operative diagnosis of SBO secondary to Intussusception. Intra-operatively it was an Ileocolocolic intussusception with duplex appendix as a leading point. We did resection and anastomosis. Post operatively she was transfused with two units of blood (20 ml/kg), given IV antibiotics, analgesics and followed with vital sign sheet (Table 1). She started PO feeding after 36 hours post operation and discharged on the 7th day improved. The case is extremely important for the study of this possible anatomical variation and its association with intussusceptions. It also serves as an input for future studies in the area. Moreover, its association with the presence of other anatomical variations such as intestinal, genitourinary and bone is important. And reporting such a rare case is very essential in the development of surgical practice.
Keywords: Duplex appendix; Intussusceptions; Cecum; Lead point; Resection and anastomosis; Ileocolocolic; Anatomic variation
Abbreviation
MD: Medical Doctor; UOG: University of Gondar; SBO: Small Bowel Obstruction; DHN: Dehydration; IV: Intravenous; PR: Pulse Rate; RR: Respiratory Rate; CBC: Complete Blood Count; WBC: White Blood Cell; Hgb: Hemoglobin; Plt: Platelet; MUAC: Mid Upper Arm Circumference; IOF: Intra-operative Finding; Bpm: Breath/beats per minute
Background
Duplex cecal appendix is a rare anatomical variation, and found in 1:25,000 (0.004%) appendectomies [1]. Approximately 100 cases of double Cecal appendix have been described so far worldwide with no case reported in Africa in general and Ethiopia in particular [2]. Intussusceptions, which are defined by Treves in 1899, as the prolapse of one part of the bowel into the lumen of the immediately adjoining part, may have a lead point, drawing the proximal bowel into the distal bowel by peristaltic activity. This lead point can be anatomic or pathologic with appendix being an anatomic lead point.
Certain anatomic variations, like mobile cecum, intraperitoneal whole colon, are also risk factor for intussusceptions. Till now there is no report of duplex appendix as a lead point in a patient with intussusception. This case report presents the first case of such presentation for the first time. The case is extremely important for the study of this possible anatomical variation and its association with intussusceptions. It also serves as an input for future studies in the area. Moreover, its association with the presence of other anatomical variations such as intestinal, genitourinary and bone is important.
Case Presentation
History
A 6 month old female patient from rural areas presented with vomiting and diarrhea of a week duration. Initially she began to experience a non-projectile bilious vomiting of ingested matter 5-6 times per day which later associated with a foul smelling blood mixed diarrhea and intermittent crying with passage of stool. Her mother witnessed an abdominal distension. She had sunkening of eye ball and she was eager to drink. She sit supported and started social smile. She was vaccinated once, and she is on exclusive breast feeding. She is the first child for the family. She has low grade fever, but no history of cough.
Physical examination
General appearance: Acutely sick looking, irritable and she was in respiratory distress.
Vital sign: PR-120 bpm, RR-42 bpm, T-38.2 °C.
Anthropometry: Wt-6 kg, Ht-62 cm, MUAC-13.5 cm.
HEENT: Pink conjunctiva, sunken eye ball
Chest: Clear and resonant.
Cardiovascular system: S1 and S2 well heard no murmur or gallop.
Abdomen: Distended, flanks are full, tenderness over the right hemi abdomen and PR-blood mixed currant jelly stool on examining finger.
Integumentary: Skin pinch goes slowly.
CNS: Sleepy
Investigation
CBC: WBC- 20.8 × 103, Hgb-12.9 g/dl, Plt-131.9 × 103
Serum electrolyte: Na-125 mmol/dl, K-3.3 mmol/dl, Cl-93.9 mmol/dl
Abdominal ultrasound
There was a well-defined bowel mass located on the right lower abdomen arising from the midline and extending to the right hypochondria with bowel-in-bowel appearance. It measures 11 cm in length. On transverse section it has typical Donat sign and it has decreased flow along the intussesceptum and intussuscepiance.
Diagnosis and management
With the assessment of SBO secondary to intussusception+some DHN+hypokalemia+hyponatremia she was admitted. Two IV line secured and she was given 75 ml/kg NS (450 ml) to run over 4 hour at a rate of 38 dpm. She was followed with some DHN follow-up sheet (Table 1) for 4 hours with good response and then she was put on maintenance fluid 200 ml (67 ml Ns+113 ml D5w+20 ml D40) to run over 8 hour at rate of 8 dpm.
| Date (d/m/y) | Time | Pr (bpm) | rr (bpm) | T (°C) | Skin pinch | sunckning | Eagerness to drink | Mentation | Cap rifill | wt | Input | output |
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| 08-10-2017 | 7:00 AM | 126 | 26 | 38.3 | Slow | Yes | Yes | Conscious | Fast | 6kg | Ns | Adequate |
| 7:30 AM | 120 | 30 | 38.2 | Slow | Yes | Yes | Conscious | Fast | - | Ns | Adequate | |
| 8:00 AM | 122 | 28 | 37.8 | slow | Yes | Yes | Conscious | Fast | - | Ns | Adequate | |
| 8:30 AM | 118 | 24 | 38.1 | Slow | Yes | Yes | Conscious | Fast | - | Ns | Adequate | |
| 9:00 AM | 108 | 34 | 38 | Slow | Yes | Yes | Conscious | Fast | - | Ns | Adequate | |
| 9:30 AM | 116 | 36 | 37.4 | Fast | Yes | Yes | Conscious | Fast | - | Ns | Adequate | |
| 10:00 AM | 110 | 28 | 37.9 | Fast | Yes | Yes | Conscious | Fast | - | Ns | Adequate | |
| 10:30 AM | 106 | 30 | 38.3 | Fast | No | Yes | Conscious | Fast | - | Ns | Adequate | |
| 11:00 AM | 100 | 28 | 37.5 | fast | No | Yes | Conscious | fast | 6.3kg | Ns | 2ml/kg/minute |
Table 1: Some DHN follow-up sheet.
She was also given 3 meq of kcl in 50 ml of ns to run over 1 hour and antibiotics (Ceftriaxone 150 mg IV bid), Paracetamol suppository 90 mg qid preoperatively. After 5 hours of resuscitation she was operated.
IOF
• Around 200 cc thin pus all over the peritoneal cavity.
• An ileocolocolic intussusception with areas of patchy ischemia extending up to the sigmoid colon and involving 20 cm of distal ileum.
• Cecum, ascending colon, transvers colon, descending colon and sigmoid colon were intraperitoneal.
• Cecum was mobile.
• The whole small bowel proximal to the obstruction was dilated.
• All the other viscera look grossly normal.
Done
• Thin pus sucked out.
• Intussusception reduced and hot pack applied and part of the ischemia in the sigmoid colon, descending colon up to the distal transverse colon turned pink.
• 20 cm of distal ileum proximal to the ileocecal valve, cecum, ascending colon and proximal 2/3 of transverse colon resected out.
• End-to-end ileotransversostomy done in two layers using vicryl 3:0.
• Peritoneal cavity was shed thoroughly with warm normal saline.
• Abdomen closed in layer.
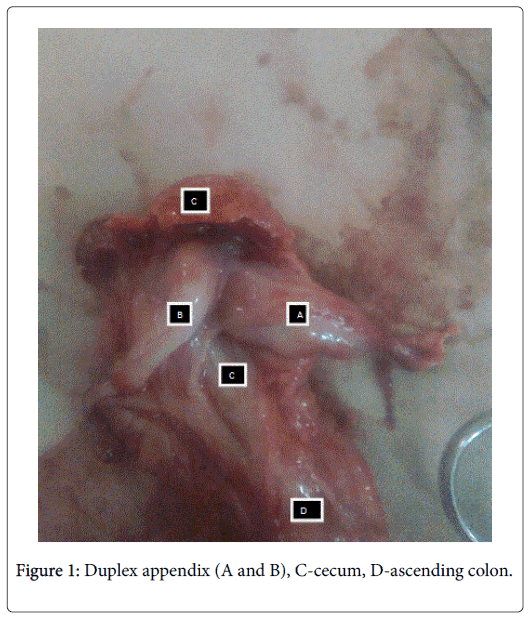
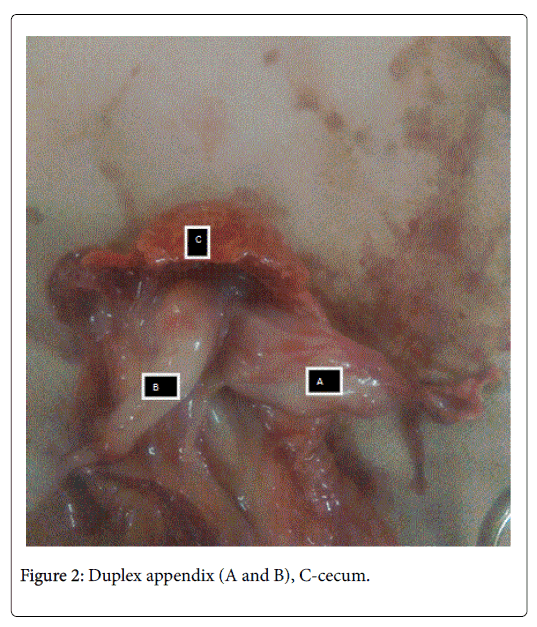
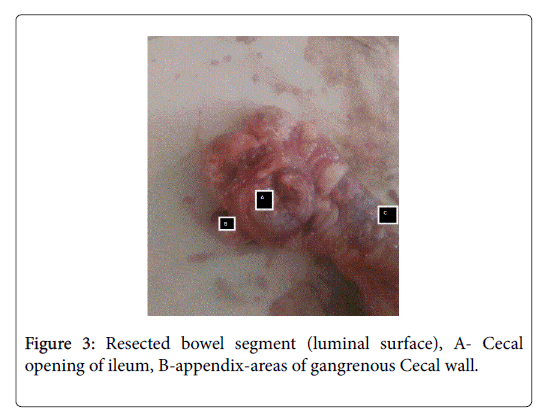
• At the end of the operation we explored the resected bowel segment (Figures 1-3).
Result
• It contains appendix which was two, each having their own mesentery and enter separately in to the cecum. There was inflammatory change in the duplex appendix, there was no fecoliths or mass (Figures 1 and 2).
• Cecum, ascending colon, proximal transverse colon had areas of patchy gangrenous bowel wall (Figure 3).
• The resected distal ileum was also gangrenous.
Postoperative course
She was followed with vital sign sheet. She was given intranasal oxygen, antibiotics (Ceftriaxone, Metronidazole), paracetamol and maintenance fluid. Clinically she had pale conjunctiva and her postoperative HCT was 37%. Despite her post-operative HCT we transfused her with two units of blood (20 ml/kg) with follow-up using transfusion follow-up sheet (Tables 2 and 3). She was also investigated with serum electrolyte, CBC and OFT all in the normal range. After 36 hours of the operation she started to pass flatus and the bowel sounds were active and we stared her PO feeding (Table 4). On the 3rd day she passed faeces and she was able to maintain her saturation, abdomen was soft except the wound. The surgical wound is healthy looking (Table 4). On the 7th day we discharged her with an advice on danger sign and linked to surgical referral clinic.
| Date (d/m/y) | Time | Pr (bpm) | Rr (bpm) | T (°C) | Edema | Itching | Rash | S3 gallop |
|---|---|---|---|---|---|---|---|---|
| 09/10/2017 | 8:00 PM | 132 | 30 | 36.8 | No | No | No | No |
| 9:00 PM | 140 | 34 | 36.9 | No | No | No | No | |
| 10:00 PM | 128 | 30 | 37 | No | No | No | No | |
| 11:00 PM | 152 | 32 | 37.2 | No | No | No | No | |
| 12:00 PM | 130 | 30 | 36.9 | No | No | No | No |
Table 2: Blood transfusions follow-up sheet.
| Date (d/m/y) | Time | Pr (bpm) | Rr (bpm | T (°C) | Rbs | Input | Output | SpO2 | Skin pinch | Sign |
|---|---|---|---|---|---|---|---|---|---|---|
| 08/10/2017 | 7:00 am | 126 | 26 | 38 | 103 mg/dl | Ns | adequate | 85% | slow | - |
| 7:30 am | 120 | 30 | 38.2 | - | Ns | adequate | - | - | - | |
| 8:00 am | 122 | 28 | 37.8 | - | Ns | adequate | - | - | - | |
| 8:30 am | 118 | 24 | 38.1 | - | Ns | adequate | - | - | - | |
| 9:00 am | 108 | 34 | 38 | - | Ns | adequate | 95% | - | - | |
| 9:30 am | 116 | 36 | 37.4 | - | Ns | adequate | - | Fast | - | |
| 10:00 am | 110 | 28 | 37.9 | - | Ns | adequate | 98% | Fast | - |
Table 3: Pre-operative vital sign sheet.
| Date | Time | pr | rr | T (°C) | Skin pinch | SpO2 | Vomiting | Bowel sounds | Input | Output |
|---|---|---|---|---|---|---|---|---|---|---|
| 09/10/2017 | 6:00 PM | 138 | 30 | 36.8 | Fast | - | No | - | Mf | - |
| 7:00 PM | 136 | 32 | 36.7 | - | - | - | - | Mf | - | |
| 10/10/2017 | 2:00 AM | 130 | 30 | 36.9 | - | - | - | - | Mf | - |
| 4:00 AM | 140 | 33 | 36.3 | Fast | 96% | - | - | - | - | |
| 8:00 AM | 136 | 31 | 36.7 | - | - | - | active | - | - | |
| 12:00 AM | 132 | 30 | 35.9 | - | - | no | - | - | - | |
| 11/10/2017 | 3:00 PM | 120 | 32 | 36.7 | - | - | - | - | - | - |
Table 4: Post-operative vital sign sheet.
Discussion And Conclusion
Since the time of first case report of double appendix, less than 100 cases have been reported on United States national library of medicine [3]. Till now there is no report of double appendix in a patient with intussusceptions on United States national library of medicine, and on PubMed. Most anomalies of the appendix have been observed during surgery not primarily involving the appendix [4]. This shows the rarity of the case and why the current reported case is the first one to be described. Overtime, some authors have presented classification to categorize anatomical variation of cecal appendix [5]. The first classification was developed by Cave which later modified by Wellbridge [6,7]. The classification categorize double appendix in to three types. Type A, B and C. Our case has Type B duplex appendix:
• Type A: Single cecum with one normally localized appendix exhibiting partial duplication.
• Type B: Single cecum with two completely separate Appendixes divided in to two.
• Type C: Double cecum each bearing its own appendix.
The horseshoe anomaly of the appendix might be considered a type D anomaly [8]. According to research outputs, most of the patient with duplex appendix had no complaints related with their duplex appendix until the occurrence of certain pathologies, Most of the time acute appendicitis. There was no report of intussusceptions associated with duplex appendix, which is the case in our patient. Intussusceptions due to identifiable lead point are rare in children constituting about 2-12%. The commonest anatomic leading point in paediatric intussusceptions is Meckel’s diverticulum. Appendix serving as a lead point for intussusceptions is 0.01% [9] certain anatomic variations like mobile cecum and intraperitoneal colon is also said to be a risk factor for intussusceptions. There is no report of duplex appendix serving as a lead point on United States national library of medicine. Associated intestinal anatomic variation, like mobile cecum, intraperitoneal colon, could be predisposing factor for intussusceptions.
Duplex appendix, intraperitoneal colon, mobile cecum, which was found in this patient, could be the predisposing factor for intussusceptions. Despite the rarity of anatomical variations in the ceacal appendix, the awareness of them is of great importance to surgeons. Anticipating this variation will help in avoiding misdiagnosis, missing appendix, diagnostic difficulties, and medico legal problems. An unnoticed second appendix may result in serious clinical and medico-legal consequences due to high risk of perforation [10]. In addition identifying it, will guide us for additional investigation to look for other associated anatomical variations described above. Finally having an anatomic variation in caecal appendix might be the cause for intussusceptions and such a report will help researcher as an input for further research and investigation. At last reporting such a rare case is very essential in the development of surgical practice.
Declaration
Ethical approval: Not applicable
Consent for publication: Taken from the patient and you can access it from the authors
Availability of data and materials: The datasets generated during and/or analysed during the current study are available from the corresponding author on reasonable request. The full data is available on chart number-680241, Gondar university hospital, Gondar, Ethiopia.
Authors’ Contribution
Dr. Yitagesu Aberra, author of this case report, is a senior resident in the department of surgery, UOG, who was the leading surgeon in the management of this patient. There were OR nurses, junior residents and master anaesthetist involved in the surgery of this patient. On both pre-operative and post-operative period residents and consultants from the paediatric side were involved in the management of this patient too. Consultant from our side was involved in every step of management of this patient.
Acknowledgment
I would like to thank the department of surgery and paediatrics who deed a lot in the management of this patient. My kind gratitude goes to OR nurses and anaesthetist above all, my assistant surgeon Dr. Bereket for their good deed and active participation.
Author’s information
Dr. Yitagesu Aberra is a final year surgical resident in the department of surgery, UOG, Gondar, Ethiopia. He is a graduate from Gondar University and worked as a general practitioner for two years in the same university hospital. He is currently practicing surgery in Gondar university hospital.
References
- Griffiths EA, Jagadeesan J, Fasih T, Jones MM (2006) Bifid vermiform appendix: A case report. Curr Curg 63: 176-178.
- Khanna AK (1983) Appendix vermiformis duplex. Postgrad Med J 59: 69-70.
- Eroglu E, Erdogan E, Gundogdu G (2002) Duplication of appendix vermiformis: A case in a child. Tech Coloproctol 6: 55-57.
- Basu R, Forshal I, Rickham PP (1959) Duplication of the alimentary tract. British J Surg. 47: 477.
- Mesko T (1989) Horseshoe anomaly of the appendix: A previously undescribed entity. Surg 106: 563-566.
- Yanar H, Ertekin C, Unal ES, Taviloglu, Guloglu R, Mete O (2004) The case of acute appendicitis and appendicial duplication. Acta Chir Belg 104: 736-738.
Citation: Aberra Y (2017) A Case Report on Duplex Appendix in a Patient with Ileocolocolic Intussusceptions. J Gastrointest Dig Syst 7: 538. DOI: 10.4172/2161-069X.1000538
Copyright: © 2017 Aberra Y. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.
Share This Article
Recommended Journals
Open Access Journals
Article Tools
Article Usage
- Total views: 4365
- [From(publication date): 0-2017 - Dec 20, 2024]
- Breakdown by view type
- HTML page views: 3686
- PDF downloads: 679