Case Report Open Access
A Case Report of the Retrieval of a Duodenal Foreign Body from the Liver
Su-Ann Yeoh1*, Philip Boger1, Timothy Bryant2 and Trevor Smith1
1Department of Gastroenterology, Southampton General Hospital, University Hospital Southampton NHS Foundation Trust, Tremona Road, SO16 6DD, Southampton, UK
2Department of Radiology, Southampton General Hospital, University Hospital Southampton NHS Foundation Trust, Tremona Road, SO16 6DD, Southampton, UK
- *Corresponding Author:
- Su-Ann Yeoh
Department of Gastroenterology, Southampton General Hospital
University Hospital Southampton NHS Foundation Trust
Tremona Road, SO16 6DD, Southampton, UK
Tel: 44 7596192475
E-mail: su-ann.yeoh@nhs.net
Received date: November 26, 2015 Accepted date: December 26, 2015 Published date: December 31, 2015
Citation: Yeoh SA, Boger P, Bryant T, Smith T (2015) A Case Report of the Retrieval of a Duodenal Foreign Body from the Liver. J Gastrointest Dig Syst 5:368. doi:10.4172/2161-069X.1000368
Copyright: © 2015 Yeoh SA, et al. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.
Visit for more related articles at Journal of Gastrointestinal & Digestive System
Abstract
A 27-year-old female patient from a psychiatric unit presented with a two-week history of abdominal pain and worsening nausea. She admitted to swallowing a ballpoint pen five months prior. Endoscopy showed the tip of the pen impacted in the superior wall of the first part of the duodenum. The endoscopist elected not to retrieve the foreign object and a computed tomograph (CT) was organised. This showed migration of the pen into the liver with the tip in close proximity to the portal vein. Laparoscopic surgery was performed to remove the pen with minimal blood loss. The patient was discharged 12 days later. This case highlights the presence of guidelines to aid decision-making in retrieval of ingested foreign bodies and the value of additional imaging to guide management of foreign body ingestions.
Keywords:
Foreign body ingestion; Duodenum; Liver; Endoscopic Retrieval; Endoscopy
Introduction
Guidelines exist on the management of ingested foreign bodies including removal of sharp-pointed and long objects. The majority can be successfully removed within 24 hours, but less is known about the efficacy of endoscopic removal after an object has been present for a longer duration. This case illustrates the consequence of conservative management of an ingested sharp, long object and highlights the value of additional imaging prior to endoscopic removal when foreign objects have been present for uncertain or longer periods of time.
Case Report
A 27-year-old female patient from a low secure psychiatry unit presented to her doctor with a two-week history of abdominal pain, worsening nausea, inability to eat without vomiting and 19 kilograms of weight loss over the last three months. On questioning, she admitted to swallowing a ballpoint pen five months prior to this. She had a history of foreign body ingestion, Type 2 diabetes and asthma.
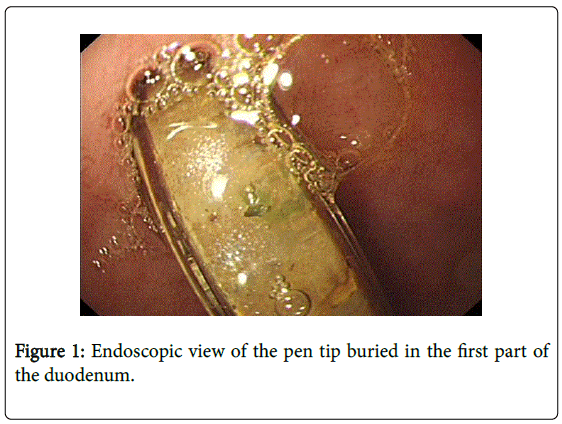
She was referred for an urgent oesophagogastroduodenoscopy (OGD) which revealed grade 2 oesophagitis, a hiatus hernia and a pen in the first part of the duodenum. She was then urgently referred to a tertiary referral hospital for removal of the pen. Her blood test result showed haemoglobin of 124 g/L, a mildly raised white cell count of 13.3 x 109/L, a mild neutrophilia of 11.9 x 109/L, C-reactive protein of 25 mg/L and renal function and electrolytes within normal range. Abdominal examination revealed a soft abdomen with mild generalized tenderness. The patient underwent a repeat OGD which showed the tip of the pen buried in the superior aspect of the first part of the duodenum (Figure 1).
Retrospective examination of hospital radiology records identified that she had a chest radiograph five months prior which showed a small metallic foreign body in the region of the fundus of the stomach. The patient however, was discharged from the Emergency Department. She also had an abdominal radiograph one month later for an unrelated indication which on closer retrospective examination showed the metallic foreign body in the region of the pylorus or the first part of the duodenum. Again, no action had been taken at the time of the radiograph.
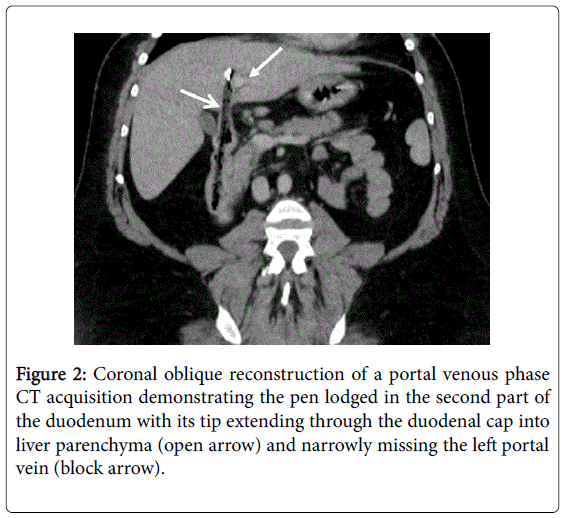
The endoscopist elected not to retrieve the pen as it was deemed hazardous due to risk of trauma and duodenal perforation. A computed tomography (CT) scan of the abdomen was organised which showed migration of the pen with the tip lying 2mm lateral to the left branch of the portal vein within segment IV of the liver and still partially within the lumen of the second part of the duodenum (Figure 2). No intra-abdominal free fluid or free gas was seen. The patient was referred to the hepatobiliary surgical team.
The patient underwent a 73-minute laparoscopic procedure. Adhesions and fibrosis were seen in the hepatoduodenal ligament with the tip of the pen located within the liver. The track was identified and opened and the pen was removed from the liver without bleeding or bile leak. The duodenal defect was primarily closed using interrupted sutures with an omental patch sutured over the repair line. Blood loss was estimated at 20 ml.
The patient was admitted to the surgical high dependency unit overnight. A nasogastric tube was inserted for drainage of gastric contents and the patient was on an intravenous insulin infusion for a few days post-operatively. She developed a chest infection post-operatively and was discharged from hospital 12 days later having made a full recovery.
Discussion
Here, we have described a case of ingestion of a 15 cm pen in a patient with recurrent intentional foreign body ingestions, none of which required surgical management previously.
Foreign body ingestion is a common problem presenting to the emergency endoscopist. It occurs more often in children due to unintentional ingestion. In adults, it is more likely to be intentional with one study reporting rates of up to 92% [1]. Higher rates of foreign body ingestion are seen in certain populations such as prisoners and patients with psychiatric illness. In these cases, foreign body ingestions tend to be intentional, recurrent and are more likely to involve longer and sharper objects [2].
Ingestion of foreign bodies can be managed conservatively, endoscopically or surgically. This decision is made based on size and nature of the object, potential harm caused by the object, length of time since ingestion, symptoms and clinical findings i.e. location of foreign body and suspicion of perforation. It has been suggested that 80-90% of foreign bodies will pass spontaneously, 10-20% require endoscopic intervention and surgical intervention in 1%. However, patients who intentionally ingest objects are more likely to require endoscopic intervention as opposed to conservative management [3].
The American Society for Gastrointestinal Endoscopy (ASGE) guidelines recommend that sharp objects or objects longer than 6cm such as the pen ingested by this patient should be urgently removed endoscopically [4]. This is because, as seen in this case, passage of the duodenal curve by longer objects is difficult. Also, foreign bodies which are left in the body run the risk of causing obstruction, fistulae/perforation and abscesses. However, endoscopic removal of longer and sharper objects is associated with higher failure rates and an increased risk of complications, prompting consideration of surgical removal [3,5,6]. Radiography is used to locate and monitor progress of foreign bodies through the gastrointestinal tract and also to aid surgical planning. It is important to note that not all ingested foreign bodies are radio-opaque [7].
The challenge in management arises when the ingested foreign body causes perforation of a viscus. Endoscopic removal of a 12 cm-long foreign body perforating the duodenum has been described by Boskoski et al where the perforation was repaired endoscopically with clips and fibrin glue. The patient developed diffuse subcutaneous emphysema during the procedure but ultimately achieved a good clinical outcome [8]. Another case was reported where a 19 cm-long toothbrush was removed endoscopically and the perforation closed with haemoclips with antibiotic cover [9].
In this case, further imaging after endoscopic visualisation of the foreign body was utilised to characterise further the location of the pen and a laparoscopic mode of extracting the pen was used after careful consideration of its risks and benefits.
Alternatively, laparoscopic removal of a fork from the duodenum has been described by Karcz et al. after endoscopy showed the fork perforating the duodenal wall [10]. A similar case to our patient has been described whereby the duodenal perforation due to a ballpoint pen was investigated using plain radiographs and a barium swallow following which the patient underwent laparoscopic removal of the foreign body and endoscopy was only used intra-operatively to assess for leaks [11].
Potential complications of foreign body removal by endoscopy include mucosal trauma, bleeding and perforation. Complication rates post-endoscopic removal reported have ranged from 1-41.5% but it is important to bear in mind that these rates vary depending on the types of foreign bodies ingested, location in the gastrointestinal tract and definition of complication [1,5,12]. If a perforation is present, closure of the perforation is an added requirement and failure to do this in a timely manner will risk spillage of viscus contents into the peritoneum causing peritonitis. Endoscopic removal of a perforating foreign body which has migrated to other organs or spaces runs other risks such as major bleeding, abscesses and bile leakage.
Laparoscopic surgery allows a better view of the peritoneal cavity and intra-abdominal organs and there is more operating space compared to the narrow confines of endoscopy. However, this involves risks such as bleeding, damage to internal organs and infection. This is especially more difficult in patients who have had previous surgeries in particular, those with a history of foreign body ingestions requiring surgical management.
Conclusion
This case therefore highlights the importance of urgent removal of ingested sharp, long objects from the gastrointestinal tract to prevent potentially serious complications. Endoscopic visualization of the object does not necessarily make endoscopic removal the most appropriate method and therefore a surgical opinion should be considered if an endoscopic removal is deemed hazardous and further imaging such as computed tomography should be considered to further guide management decisions of foreign body removal.
References
- Palta R, Sahota A, Bemarki A, Salama P, Simpson N, et al. (2009) Foreign-body ingestion: characteristics and outcomes in a lower socioeconomic population with predominantly intentional ingestion. GastrointestEndosc 69: 426-433.
- Malick KJ (2013) Endoscopic management of ingested foreign bodies and food impactions. GastroenterolNurs 36: 359-365.
- Webb W (1995) Management of foreign bodies of the upper gastrointestinal tract:update. GastrointestEndosc 14: 39-51.
- Ikenberry SO, Jue TL, Anderson MA, Appalaneni V, Banerjee S, et al. (2011) ASGE Standards of Practice Committee Management of ingested foreign bodies and food impactions. GastrointestEndosc 73: 1085-1091.
- Cho JH, Chun SW, Choi JS, Choi JY, Kang BD, et al. (2013) Risk Factor for Complications Associated With Endoscopic Removal of Ingested Foreign Body in Upper GI Tract. GastrointestEndosc 77: 5S.
- Gracia C, Frey CF, Bodai BI (1984) Diagnosis and management of ingested foreign bodies: a ten-year experience. Ann Emerg Med 13: 30-34.
- Guelfguat M, Kaplinskiy V, Reddy SH, DiPoce J (2014) Clinical guidelines for imaging and reporting ingested foreign bodies. AJR Am J Roentgenol 203: 37-53.
- Boakoski I, Tringali A, Landi R, Familiari P, Contini AC, et al. (2013) Endoscopic retrieval of a duodenal perforating teaspoon. World J GastrointestEndosc 5: 186-188.
- Lee TH, Lee SH, Park JH, Park DH, Park JY, et al. (2008) Endoscopic management of duodenal perforation secondary to ingestion of an uncommon foreign body. GastrointestEndosc 67: 730-731.
- Karcz WK, Kulemann B, Seifert GJ, Schrag HJ, Küsters S, et al. (2011) Video. Laparoscopic extirpation of a fork from the duodenum. SurgEndosc 25: 2363.
- Golffier C, Holguin F, Kobayashi A (2009) Duodenal perforation because of swallowed ballpoint pen and its laparoscopic management: report of a case. J PediatrSurg 44: 634-636.
- Emara MH, Darwiesh EM1, Refaey MM1, Galal SM1 (2014) Endoscopic removal of foreign bodies from the upper gastrointestinal tract: 5-year experience. ClinExpGastroenterol 7: 249-253.
Relevant Topics
- Constipation
- Digestive Enzymes
- Endoscopy
- Epigastric Pain
- Gall Bladder
- Gastric Cancer
- Gastrointestinal Bleeding
- Gastrointestinal Hormones
- Gastrointestinal Infections
- Gastrointestinal Inflammation
- Gastrointestinal Pathology
- Gastrointestinal Pharmacology
- Gastrointestinal Radiology
- Gastrointestinal Surgery
- Gastrointestinal Tuberculosis
- GIST Sarcoma
- Intestinal Blockage
- Pancreas
- Salivary Glands
- Stomach Bloating
- Stomach Cramps
- Stomach Disorders
- Stomach Ulcer
Recommended Journals
Article Tools
Article Usage
- Total views: 10464
- [From(publication date):
December-2015 - Apr 05, 2025] - Breakdown by view type
- HTML page views : 9647
- PDF downloads : 817