Research Article Open Access
A Case Report of ALPPS for Giant Hepatic Cancer Complicated with Perioperative Acute Renal Injury
Mohammad Abdul Mazid, Fu Zhen Wan, Gazi Shahinur Akter, Zheng Hui Ye, Hong Chuan Zhao and Xiao Ping Geng*Department of Hepatobiliary & Pancreatic Surgery and Liver Transplantation, The First Affiliated Hospital of Anhui medical University, Anhui Medical University, China
- *Corresponding Author:
- Xiao Ping Geng
Department of Hepatobiliary & Pancreatic Surgery and Liver Transplantation
the First Affiliated Hospital of Anhui Medical University
Anhui Medical University, 81 Meishan Road, Sushan District
Hefei 230032, Anhui, China
E-mail: xp_geng@163.net
Received date: April 06, 2017; Accepted date: May 02, 2017; Published date: May 09, 2017
Citation: Mazid MA, Wan FZ, Akter GS, Ye ZH, Zhao HC, et al. (2017) A Case Report of ALPPS for Giant Hepatic Cancer Complicated with Perioperative Acute Renal Injury. J Biol Med Science 1:101.
Copyright: © 2017 Mazid AM, et al. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.
Visit for more related articles at Journal of Biological and Medical Sciences
Abstract
Background: The aim of the study is to explore the safety and efficacy (outcomes) of two-step Associating liver partition and portal vein ligation for staged hepatectomy (ALPPS) combined with hepatic excision and portal vein ligation for the treatment of giant hepatocellular carcinoma. Methods: The clinical data of one patient case of giant right hepatocellular carcinoma treated by ALPPS at the first Affiliated Hospital of Anhui Medical University in April 2016 was analyzed retrospectively. Surgical regimen: For left anterior lobe, the left anterior lobectomy was performed and the hepatic remnant was covered with the artificial vessel suture. After 13 days, the right portal vein was ligated and the right and left hepatectomy were performed. Results: The right hepatic lobe tumor diameter was about 16 cm, and the standard total hepatic volume was 1256.60 m. The remaining proportion of left lobe volume about 347.15 ml weight 0.53 (l/kg), at the time of the second step of ALPPS which was increased to 865.7 ml. The first step operative time was 197 minutes and second operative time was 75 min respectively. The ALPPS first step intraoperative bleeding was 765 ml and 465 ml on the second step. The postoperative recovery of liver function was 6 days for step one and 3 days for step two. The first day after the first step surgery acute oliguria with acute renal injury, creatinine levels were high for 7 days which altered at the second postoperative day of the second step. There was no new complication in the second postoperative period. Conclusion: ALPPS provides a new therapeutic option for hepatocellular carcinoma with insufficient hepatic volume, but it may bring perioperative burden to related organs and cause related complications or even organ failure. The safety of ALPPS in hepatocellular carcinoma patients remain to be assessed and explored.
Keywords
ALPPS; Acute renal failure; Hepatocellular carcinoma
Abbreviations
ALPPS: Associating Liver Partition and Portal Vein Ligation; AST: Aspartate Transaminase; ALT: Alanine Transaminase; BUN: Blood Urea Nitrogen; ICG-R15: Indocyanine Green Retention Test; FLV: Future Liver Volume; PO: Post-operative; ARF: Acute Renal Failure
Introduction
Liver primary and secondary malignant tumors surgical resection is curative for patients because the capability of the liver is unique to regenerate itself. Induced chemotherapy liver injury the future liver remnant must be 30% of total volume, in cirrhosis liver the 40% of the future liver remnant is advisable [1].
Hepatectomy for hepatocellular carcinoma is by far the most important treatment for patients with liver cancer who have achieved radical treatment. In order to avoid liver failure, it is important to ensure that the patient has sufficient residual liver volume after hepatectomy. More patients with hepatocellular carcinoma are diagnosed with a huge tumor volume which makes patients often lose the opportunity to obtain radical treatment.
In recent years, there is a new technique of hepatic resection performed in two stages called Associating Liver Partition and Portal vein ligation (ALPPS) for Staged hepatectomy has been depicted [2]. The first step of this procedure associates the intraoperative ligation of the right portal branch to the partition of the liver, usually following the scheme of an extended right hepatectomy. In contrast to a classical hepatectomy, the diseased part of the liver is left in situ and remains vascularized by the right hepatic artery only, while the biliary and systemic venous drainage through the right biliary duct and hepatic veins, respectively, are preserved [3]. In the second step of the methodology that is normally performed inside 7 to 15 days after the principal, the diseased part of the liver is evacuated by basically separating the remaining biliary, hepatic blood vessel and systemic venous pedicles.
Right now, the surgery has been utilized by specialists to treat patients with liver metastasis of colon malignancy, however, patients with primary liver cancer, the operation for huge hepatocellular carcinoma resection is still being investigated and considered. Currently, the surgery has been utilized by specialists to treat patients with liver metastasis of colon cancer, but for patients with primary liver cancer, the operation for large hepatocellular carcinoma resection indications are still being explored and studied.
Acute renal injury (AKI), or formerly known as acute renal failure (ARF), is usually caused by a slowing or decreasing blood flow to the kidneys. This happens because the renal urine outflow tract (ureter) is blocked and waste product cannot leave the body through the urine. After liver surgery, decreased kidney blood flow, monocytemacrophage function, coagulation and fibrinolysis system dysfunction, granulocyte elastase release and other factors can lead to renal damage. Therefore, in the liver resection process, the protection of renal function is very important [4].
Methods
The clinical data of one case of giant right hepatocellular carcinoma treated by ALPPS at the first Affiliated Hospital of Anhui Medical University in April 2016 was analyzed retrospectively. The safety and effectiveness of the procedure was evaluated by perioperative indicators and follow-up data. The surgical regimen is as follow: For left anterior lobe, the left anterior lobectomy was performed and the hepatic remnant was covered with the artificial vessel suture. After 13 days, the right portal vein was ligated and the right and left hepatectomy were performed. Recently, the domestic giant liver cancer ALPPS after acute kidney injury was reported in the literature, but international studies have pointed out that ALPPS can lead to perioperative severe organ damage and failure [5]. In April 2016, we performed an ALPPS on a patient with a huge tumour in the right lobe of the liver. The patient was discharged on the 10th day after step 2 and had no obvious abnormalities at 6 months follow-up.
Results
Pre-operative findings
A 48 years old male with abdominal mass and distention from last two weeks (BMI: 21.72 kg/m2, 65 kg/1.73 m) came for treatment. There was no history of diabetes and hypertension. Blood routine examination revealed that biochemical serum albumin and coagulation test and renal function were all in the normal range. Other results are as follows: HBV-DNA: 2 × 105 copies/ml, tumor marker AFP: 100.7 ng/ml, Child-Pugh score A level, and ICG R15 2.7% (preoperative).
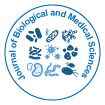
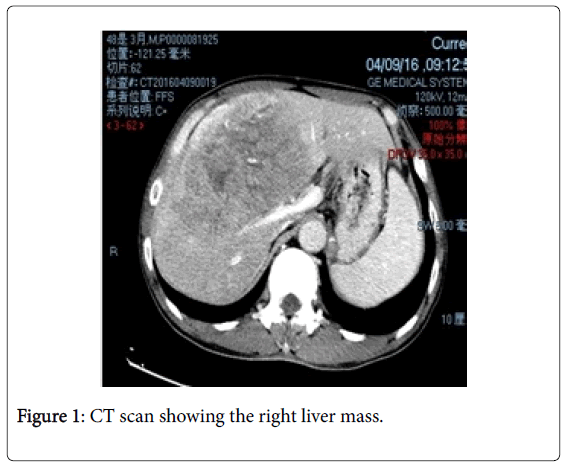
Radiologic examination abdominal ultrasound, CT scans, and an MRI result showed massive mass at the right liver lobe as shown in Figure 1 and 2 (which is hepatocellular carcinoma as confirmed by pathology results later), Splenomegaly, inferior vena cava, and significantly narrow adrenal vein with right renal atrophy.
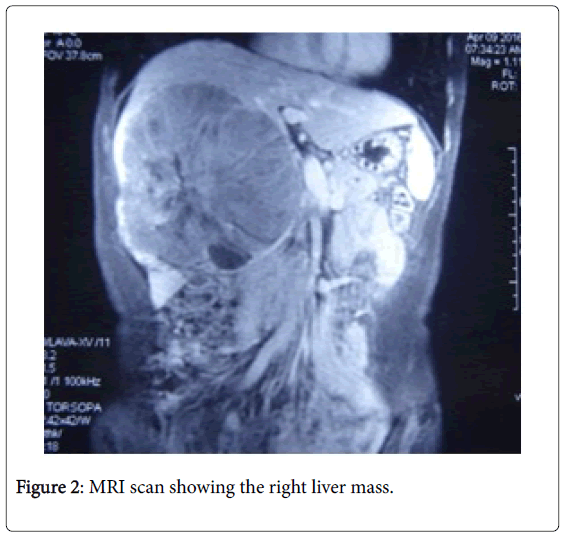
On the basis of CT scan and MRI imaging data to reconstruct the 3D imaging showing hyperplasia of the right lobe of the liver as shown can be seen in Figure 3, for further consideration. The future liver remnant volume (FLR) was 347.15 ml, which was 27.63% of the total liver volume. The ratio of L/Kg was 0.53%. Upon overall assessment of the patient's intolerance to one-stage resection of the tumor, we considered PVE. Because PVE might increase the risk of tumor progression, especially in the Non-embolized side and the first stage of operation might further stimulate tumor growth due to the increased release of growth factors, we decided to adopt ALPPS procedure for this patient.
Procedure and intraoperative findings first step alpps
We made an “L” shaped incision with midline extent. After exploration of the peritoneum, a right branch of portal vein was ligated and transecting the liver parenchyma was done. An intraoperative ultrasound examination was performed to assess the attributes of the neoplastic neoplasm and their association with the vascular and biliary tree. Intraoperative liver ultrasound showed mild liver cirrhosis at the right liver lobe.
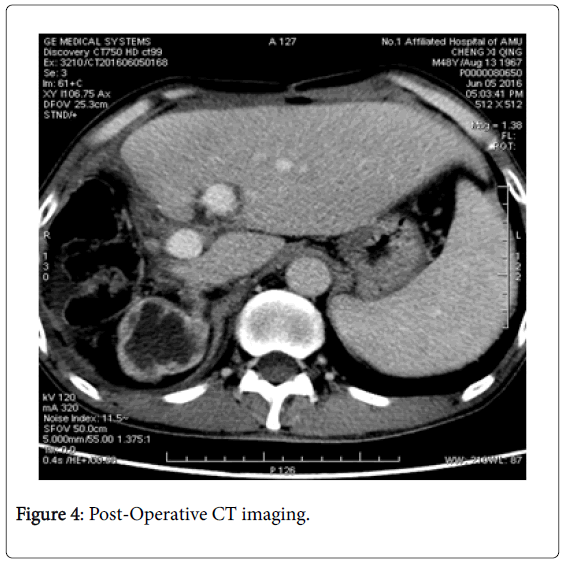
Tumor size about 16 × 13 × 11 cm, occupying V, VI, VIII and part of the VII segment of the liver. A large number of hyperplasia invaded the blood vessels, hilar tissue, and the left lobe of the liver left. The smaller liver lobe measured about 13 × 13 cm with ligation of the right portal vein, right hepatic artery with a narrow line, one hundred grams of CUSA+titanium clamping performed on left and right parenchyma (Figure 4).
Intraoperative bleeding was 765 ml; however, no intraoperative blood transfusion was required. Pringle maneuver duration was 27 minutes to minimize the blood loss. The specimen was sent for pathology of the remaining liver tissue covered with Johnson's SURGICEL® bio-hemostatic yarn with only single drainage tube placed for volume.
The patient's body temperature began to rise to 38.8°C and WBC reached 21.46 × 109/L. Three-dimensional reconstruction of the simulation data suggested that the left liver volume of 865.7 ml compared with preoperative 347.5 ml increased by 149.12%.
The average growth rate was 43.2 ml/day. Occupancy volume was 1646.8 ml compared to preoperative 1867.05 ml (11.79% reduction). Also on the same day, ICG R15 was 14.9%. Considering that the residual liver function of the patient was sufficient to tolerate surgical resection, we performed the second phase of ALPPS surgery on the 13th postoperative day.
Second step alpps
Right hemi hepatectomy: Upon reopening the abdominal cavity along the incision, we found the first original operating site with a small amount of ascitic fluid in the abdominal cavity.
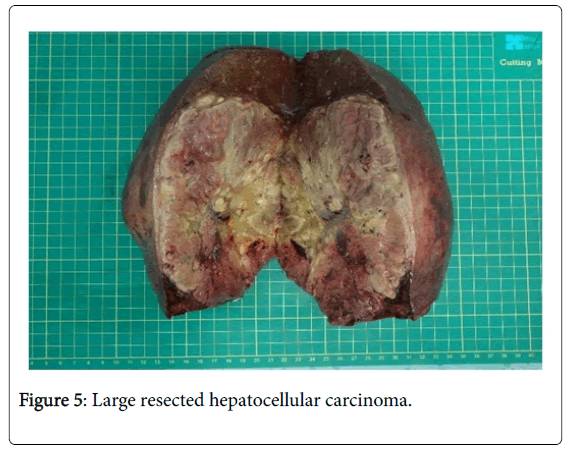
Although test reports were negative for the ascetic tap, the right hepatic duct separated with left hepatic parenchyma and the right hepatic vein was cut off and the venous stump was cut with 4-0 Prolene suture. From the right liver capsule, we removed the specimen weighing 2062 g.
A drainage tube and a negative pressure ball were set during the second stage of operation (time 75 minutes, estimated blood loss of 465 ml). The patient received a postoperative infusion of plasma is 400 ml.
Histopathological examination of resected specimens suggested that 17 × 12 × 11 cm hepatocellular carcinoma as shown in Figure 5 (WHO classification grade II) was associated with extensive necrosis and tumor thrombus formation within the vessel.
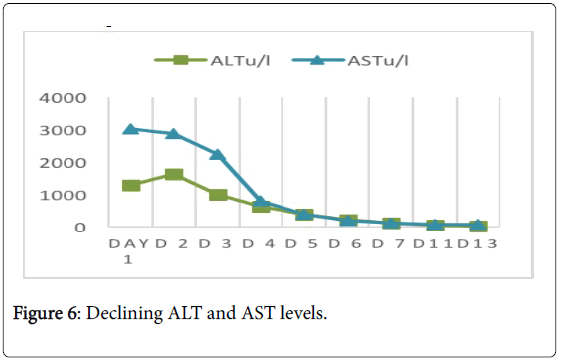
The patient's general condition improved the day after eating and activities. Also, transaminase and total bilirubin levels did not increase after surgery as shown in Figure 6.
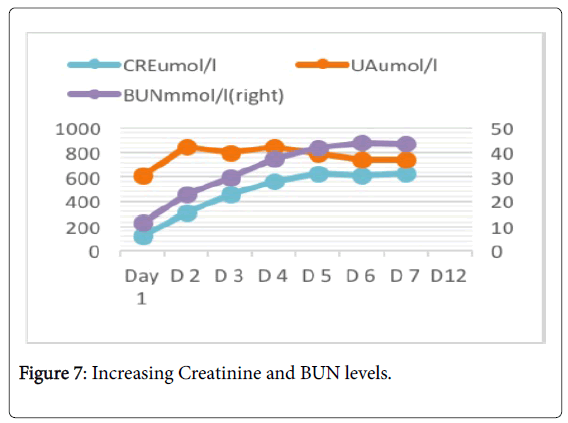
Renal function had been declining as shown in Figure 7. On the second day after surgery, creatinine dropped to normal levels. On the fourth day after surgery, leukocytes fell to normal levels. The patient started eating liquid food the next day and started bedside activities. However, at the first postoperative day, laboratory results showed very high levels AST and ALT (3017 u/l and 1619 u/l).
Also, patient had oliguria (24-hour urine output 380 ml), then gradually increased in the eighth day to the highest peak (4395 ml) followed by stability (2000 ml). Creatinine also began to rise from 124 umol/l to 630 umol/l on the first day (post-operative day 7), then gradually decreased to 214 umol/l before the second stage (postoperative day 13). No dialysis was performed during this period. We reviewed the ultrasound on the fifth day after surgery, the results suggested renal atherosclerosis. On the 12th day, Figure 4 postoperatives CT scan showed a small pleural effusion associated with pneumonia in both sides of lungs.
Other laboratory tests showed no abnormalities. ICG R15 was 16.8% after the eighth day. The patient was discharged on day 10 postoperatively.
Follow up treatment
The patients were treated with entecavir 0.5 mg QD anti-hepatitis B virus drug continuously. At 6 week check-up after discharge, the results were AFP: 7.2 ng/ml, ICG R15 15.6%, normal liver and kidney function and residual liver volume LLV: 898.46 (Table 1).
| Preoperative | PO Result: Day 9 |
PO Result: D 13 |
PO Result: D 21 (D 8 after 2nd operation) |
PO Result: D 50 (D 40 after 2nd operation) |
|
|---|---|---|---|---|---|
| ICG R15 | 2.7 | 14.9 | 16.8 | 15.6 | |
| FLV (mL) | 317.17 | 816.3 | 865.7 | 898.46 |
Table 1: Chart for ICG R15 and FLV.
At 3 months check-up after discharge, results were AFP: 6.94 ng/ml, normal liver, and kidney function, HBV-DNA <1000 copies / ml. At more than 6 months after surgery, no symptoms were reported; weight increased 3 Kg than before surgery and the quality of life was good.
Discussion
The advantage of ALPPS in residual liver hyperplasia has been widely recognized, and the literature has shown that the residual liver volume can proliferate by 61% to 93% during the first 9-14 days of median follow-up [6,7]. About 95%-100% of patients completed the overall operation, of which 86%-100% of patients received R0 resection.
In about 70% of the cases, ALPPS is currently used to treat colorectal cancer liver metastases (CRLMs), according to data from the International ALPPS Registry [8-11]. Some scholars [12] on the international registration of ALPPS liver cancer and colorectal cancer liver metastases (CRLM) analyzed the results. The results showed that the residual liver volume of hepatocellular carcinoma grew more rapidly and widely, but in the patients with colorectal cancer liver metastases was lower than 90 days after operation. The liver cancer patients were significantly higher than those in the treatment of colorectal cancer patients with liver metastases, almost five times the latter. The scholars believe that ALPPS used in the treatment of liver cancer should be treated with caution.
Biliary fistula and infection is the main complication after ALPPS. It is also the most common cause of postoperative death. How to prevent serious complications and reduce mortality is still an urgent problem to be solved. Reported in the literature of experienced hepatobiliary surgery center, serious complications rate was reduced to 13-14%, mortality was reduced to 0-6% [13]. The analysis of surgical techniques, learning curve and the standardization of ALPPS are the main factors affecting morbidity and mortality.
For this patient, we have considered the complications to be more likely due to liver surgical trauma caused by the release of inflammatory factors and exacerbating the deterioration of renal function. Other important factors in this case were that the patient had right renal arteriosclerosis, significantly narrowed renal vein, and right renal atrophy. Because of lack of research and long-term efficacy, prognosis of patients with ALPPS is not known and needs more research. Our patient is symptom free with good quality of life after 6 months of surgery with ALPPS.
Conclusions
• ALPPS provides a new therapeutic option for hepatocellular carcinoma with insufficient hepatic volume, but it may bring peroperative burden to related organs and cause-related complications or even organ failure.
• The safety of ALPPS in hepatocellular carcinoma Patients remain to be assessed and explored.
References
- Adams RB, Aloia TA, Loyer E, Pawlik TM, Taouli B, et al. (2013) Selection for hepatic resection of colorectal liver metastases: Expert consensus statement. HPB (Oxford) 15: 91-103.
- Alvarez FA, Ardiles V, Sanchez Claria R, Pekolj J, et al. (2013) Associating liver partition and portal vein ligation for staged hepatectomy (ALPPS): Tips and tricks. J Gastrointest Surg 17: 814-821.
- Schnitzbauer AA, Lang SA, Goessmann H, Nadalin S, Baumgart J, et al. (2012) Right portal vein ligation combined with in situ splitting induces rapid left lateral liver lobe hypertrophy enabling 2-staged extended right hepatic resection in small-for-size settings. Ann Surg 255: 405-414.
- Xiaoping C, Wenguang Z (2001) Ulinastatin in liver resection perioperative experience. Chinese Journal of Hepatobiliary Surgery 60-61.
- Torres OJ, Moraes-Junior JM, Lima e Lima NC, Moraes AM (2013) Associating liver partition and portal vein ligation for staged hepatectomy (ALPPS): A new approach in liver resections Arq Bras Cir Dig 25: 290-292.
- Nadalin S, Capobianco IJ (2014) Indications and limitations of the ALPPS procedure. Experiences with 15 cases in the individual center, Zeitschrift fur Gastroenterologie 52: 35-42.
- Cai X, eng S, Duan L, Wang Y, Yu H, et al. (2014) Completely laparoscopic ALPPS using round-the-liver ligation to replace parenchymal transection for a patient with multiple right liver cancers complicated with liver cirrhosis. J Laparoendosc Adv Surg Tech A 24: 883-836.
- Ariizumi S, Kotera Y, Katagiri S, Nakano M, Nakanuma Y, et al. (2014) Long-term survival of patients with cholangiolocellular carcinoma after curative hepatectomy. Ann Surg Oncol 21: S451-458.
- Hackl C, Neumann P, Gerken M, Loss M, Klinkhammer-Schalke M, et al. (2014) Treatment of colorectal liver metastases in germany: A ten-year population-based analysis of 5772 cases of primary colorectal adenocarcinoma. BMC Cancer 14: 810.
- Sadot E, Koerkamp GB, Leal JN, Shia J, Gonen M, et al. (2015) Resection margin and survival in 2368 patients undergoing hepatic resection for metastatic colorectal cancer: Surgical technique or biologic surrogate? Ann Surg 262: 476-485.
- Zhong JH, Ke Y, Gong WF, Xiang BD, Ma L, et al. (2014) Hepatic resection associated with good survival for selected patients with intermediate and advanced-stage hepatocellular carcinoma. Ann Surg 260: 329–340.
- D'Haese JG, Neumann J, Weniger M, Pratschke S, Björnsson B, et al. (2016) Should alpps is used for liver resection in intermediate-stage hcc? Ann Surg Oncol 23: 1335-1343.
- Hernandez-Alejandro R, Bertens KA, ineda-Solis K, Croome KP (2015) Can we improve the morbidity and mortality associated with the associating liver partition with portal vein ligation for staged hepatectomy (ALPPS) procedure in the management of colorectal liver metastases. Surgery 157: 194-201.
Relevant Topics
Recommended Journals
Article Tools
Article Usage
- Total views: 2685
- [From(publication date):
June-2017 - Jul 12, 2025] - Breakdown by view type
- HTML page views : 1764
- PDF downloads : 921