A Case Report and Literature Analysis of 49-Year-Old Male Patient with Neck Paraganglioma
Received: 01-May-2024 / Manuscript No. ocr-24-137339 / Editor assigned: 03-May-2024 / PreQC No. ocr-24-137339 / Reviewed: 17-May-2024 / QC No. ocr-24-137339 / Revised: 22-May-2024 / Manuscript No. ocr-24-137339 / Published Date: 29-May-2024 DOI: 10.4172/2161-119X.1000577 QI No. / ocr-24-137339
Abstract
Paraganglioma are rare neuroendocrine tumors arising from paraganglia derived from neural crest cells. They commonly occur in the head and neck region, with the carotid body being the most frequent site. Here, we present a case report of a 49-year-old male patient with a neck Paraganglioma. The patient presented with a painless neck mass, and further investigations led to the diagnosis of Paraganglioma. We discuss the clinical presentation, radiological findings, histopathological features, management, and prognosis of this rare entity. Additionally, we provide a literature analysis to enhance understanding and management strategies for neck Paraganglioma
Keywords
Paraganglioma; Neck; Neuroendocrine tumor; Case report; Literature analysis
Introduction
Paraganglioma are rare neuroendocrine tumors arising from extra-adrenal chromaffin cells derived from neural crest cells. They can occur anywhere along the autonomic nervous system, with the head and neck region being one of the most common sites [1]. Within the head and neck, Paraganglioma often arise from the carotid body, jugular vein, tympanic membrane, and vagus nerve. However, Paraganglioma originating from the neck are relatively uncommon. Here, we present a case report of a 49-year-old male patient with a neck Paraganglioma, highlighting the clinical presentation, diagnostic approach, management strategies, and literature review [2].
Case Report
A 49-year-old male patient presented to our clinic with a painless swelling in the right side of his neck that had been progressively increasing in size over the past six months. The patient denied any history of trauma, pain, dysphagia, dyspnea, or voice changes [3]. He had no significant past medical history and was not on any medications. Physical examination revealed a non-tender, firm, mobile mass measuring approximately 3 cm in diameter in the right lower neck region, just above the clavicle. There were no palpable cervical lymph nodes.
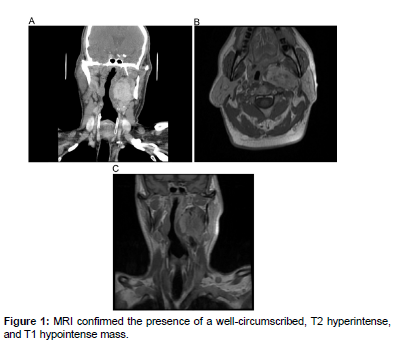
Given the suspicion of a neck mass, further investigations were pursued. Ultrasound examination of the neck revealed a well-defined, hypoechoic mass with internal vascularity, suggestive of a vascular lesion. Subsequent contrast-enhanced computed tomography (CT) scan of the neck demonstrated a homogeneously enhancing mass located poster lateral to the right common carotid artery, consistent with a Paraganglioma [4]. Magnetic resonance imaging (MRI) was performed for better soft tissue delineation and to assess the relationship of the tumor with adjacent structures. MRI confirmed the presence of a well-circumscribed, T2 hyperintense, and T1 hypointense mass, without evidence of invasion into surrounding structures (Figure 1).
Based on the clinical presentation and radiological findings, a fine-needle aspiration biopsy (FNAB) was performed, which yielded cytology consistent with a Paraganglioma. Subsequently, the patient underwent surgical resection of the neck mass [5]. Intraoperatively, the tumor was found to be intimately associated with the carotid artery, but without invasion into the vessel wall. Complete excision of the mass was achieved, and the patient had an uneventful postoperative course.
Histopathological examination of the excised specimen confirmed the diagnosis of a Paraganglioma, showing nests of polygonal cells with eosinophilic cytoplasm arranged in a characteristic "zellballen" pattern. Immunohistochemical staining was positive for chromogranin and synaptophysin, supporting the neuroendocrine nature of the tumor. The surgical margins were negative for tumor involvement [6].
Discussion
Paraganglioma are rare neuroendocrine tumors originating from paraganglia, which are dispersed neuroendocrine cells derived from neural crest cells. These tumors can occur sporadically or as part of hereditary syndromes such as multiple endocrine neoplasia type 2 (MEN2) and von Hippel-Lindau (VHL) syndrome [1]. In the head and neck region, paragangliomas most commonly arise from the carotid body, accounting for approximately 60% of cases, followed by the jugular vein (15-20%), tympanic membrane (5-10%), and vagus nerve (5-10%).
The clinical presentation of neck paragangliomas varies depending on the size and location of the tumor. Patients may present with a painless neck mass, as seen in our case, or with symptoms related to compression of adjacent structures such as dysphagia, dyspnea, or hoarseness [7]. The diagnosis of paragangliomas relies on a combination of clinical, radiological, and histopathological findings. Imaging modalities such as ultrasound, CT, and MRI are helpful in delineating the extent of the tumor and its relationship with adjacent structures. Fine-needle aspiration biopsy may be performed to obtain cytological material for diagnosis, although the definitive diagnosis is established by histopathological examination of the surgical specimen. Surgical resection remains the mainstay of treatment for neck paragangliomas [8]. The goal of surgery is complete excision of the tumor while preserving vital structures such as the carotid artery and cranial nerves. Preoperative embolization may be considered in larger tumors to minimize intraoperative bleeding. Adjuvant radiotherapy or chemotherapy may be indicated in cases of unresectable tumors, metastatic disease, or as a palliative measure. Long-term follow-up is essential due to the risk of recurrence and the potential for the development of metachronous or synchronous tumors, particularly in patients with hereditary syndromes [9,12].
Conclusion
Neck paragangliomas are rare neuroendocrine tumors that require a multidisciplinary approach for diagnosis and management. Clinical suspicion, coupled with appropriate imaging studies and histopathological examination, is crucial for accurate diagnosis. Surgical resection remains the cornerstone of treatment, with the goal of complete excision while preserving neurovascular structures. Long-term follow-up is essential to monitor for recurrence and to manage patients with hereditary syndromes predisposing to paraganglioma development. Further studies are needed to elucidate the molecular mechanisms underlying paraganglioma pathogenesis and to optimize treatment strategies for this rare entity.
Acknowledgement
None
Conflict of Interest
None
References
- Nelaturi P, Nagarajan P, Sabapathy SK, Sambandam R (2021)Swarna Bindu Prashana-an Ancient Approach to Improve the Infant’s Immunity.Bio Tra Ele Res 199: 2145-2148.
- Asai T, Nagata A, Shingu K (2008)Awake tracheal intubation through the laryngeal mask in neonates with upper airway obstruction. Paediatr Anaesth 18: 77-80.
- Sivanandan S, R Agarwal, A Sethi (2017)Respiratory distress in term neonates in low-resource settings.Semin Fetal Neonatal Med 22: 260-266.
- Randolph AG (2009)Management of acute lung injury and acute respiratory distress syndrome in children.Crit Care Med 37: 2448-2454.
- Liu J (2010)Clinical characteristics, diagnosis and management of respiratory distress syndrome in full-term neonates.Chin Med J 123: 2640-2644.
- Niesłuchowska-Hoxha A (2018)A retrospective study on the risk of respiratory distress syndrome in singleton pregnancies with preterm premature rupture of membranes between 24+ 0 and 36+ 6 weeks, using regression analysis for various factors.Biomed Res Int 15: 67-71.
- Alfarwati TW (2019)Incidence, risk factors and outcome of respiratory distress syndrome in term infants at Academic Centre, Jeddah, Saudi Arabia.Medical Archives, 73: 183.
- Wang J (2015)Analysis of neonatalrespiratory distress syndrome among different gestational segments.Int J Clin Exp 8: 16273.
- Jing L, Y Na, L Ying (2014)High-risk factors of respiratory distress syndrome in term neonates: a retrospective case- control study.Balkan Med J 5: 64-68.
- Al Riyami N (2020)Respiratory distress syndrome in neonates delivered at term-gestation by elective cesarean section at tertiary care hospital in Oman.Oman Med J 17: 133.
- Tochie JN (2020)The epidemiology, risk factors, mortality rate, diagnosis, etiologies and treatment of neonatal respiratory distress: a scoping review.
- Raha BK, MJ Alam, MAQ Bhuiyan (2019)Risk Factors and Clinical Profile of Respiratory Distress in Newborn: A Hospital Based Study in Bangladesh Army.Bangladesh Med J 48: 21-27.
Indexed at, Google Scholar, Crossref
Indexed at, Google Scholar, Crossref
Indexed at, Google Scholar, Crossref
Indexed at, Google Scholar, Crossref
Indexed at, Google Scholar, Crossref
Indexed at, Google Scholar, Crossref
Indexed at, Google Scholar, Crossref
Indexed at, Google Scholar, Crossref
Indexed at, Google Scholar, Crossref
Indexed at, Google Scholar, Crossref
Citation: Miao X (2024) A Case Report and Literature Analysis of 49-Year-OldMale Patient with Neck Paraganglioma. Otolaryngol (Sunnyvale) 14: 577. DOI: 10.4172/2161-119X.1000577
Copyright: © 2024 Miao X. This is an open-access article distributed under theterms of the Creative Commons Attribution License, which permits unrestricteduse, distribution, and reproduction in any medium, provided the original author andsource are credited.
Share This Article
Recommended Journals
Open Access Journals
Article Tools
Article Usage
- Total views: 375
- [From(publication date): 0-2024 - Apr 07, 2025]
- Breakdown by view type
- HTML page views: 205
- PDF downloads: 170