A Case of Kaposi's Sarcoma of the Rectum in a Homosexual Male with HIV–AIDS
Received: 04-Oct-2017 / Accepted Date: 20-Oct-2017 / Published Date: 26-Oct-2017 DOI: 10.4172/2332-0877.1000340
Abstract
Kaposi sarcoma (KS) is a locally aggressive endothelial tumor, commonly diagnosed among individuals with acquired immunodeficiency syndrome (AIDS). The most typical site of involvement by KS is the skin, but in some cases, it can also affect other tissues and organs. Most patients with gastrointestinal involvement of Kaposi's sarcoma remain asymptomatic and they are often diagnosed on endoscopy or autopsy. However, there are cases of KS mimicking ulcerative colitis (UC), whereby clinical manifestations can confuse physicians. We report a 31 y old homosexual man who presented with rectal pain and bleeding. Patient was diagnosed eight years ago with HIV/ AIDS, and despite highly active retroviral therapy, he developed extensive skin lesions. Because of expressive rectal pain and bleeding, he underwent rectoscopy, which revealed ulcerous and hemorrhagic lesions. The rectoscopic and clinical presentation mimicked acute flare of UC, which was patient initial diagnosis. Tissue samples were collected for microscopical examination. After histological, histochemical and immunhistochemical examination of the sampled tissue, KS diagnosis was confirmed. The clinical manifestations of Kaposi sarcoma can be confused with acute exacerbation of ulcerative colitis often delaying the diagnosis. Therefore, early endoscopic evaluation with adequate biopsies could help in timely diagnosis and management of gastrointestinal KS (GI-KS) in patients with HIV/AIDS, even if they do not have skin lesions.
Keywords: Kaposi sarcoma; AIDS; HIV; Ulcerative colitis; Gastrointestinal KS
Introduction
Kaposi sarcoma (KS) is a locally aggressive endothelial tumor that typically presents with cutaneous lesions in the form of multiple patches, plaques or nodules, but may also involve mucosal sites, lymph nodes and visceral organs [1]. The main cause of KS is Human Herpesvirus-8 (HHV-8), a large double-stranded DNA virus [2].
The most typical site of involvement by KS is the skin. Recognizing HIV-related skin changes may lead to the diagnosis of HIV infection in the early stages, allowing initiation of appropriate antiretroviral therapy. Many associated skin diseases are more severe in this group. The most common cutaneous infections caused by Staphylococcus aureus especially MRSA that is one of the most important health concerns is antimicrobial resistance [3-6].
The cutaneous lesions can be solitary, localized or disseminated. The involvement of a wide variety of tissues and organs has been also described, although KS is very rarely seen in skeletal muscles, brain and kidney [7].
Visceral involvement in acquired immune deficiency syndrome (AIDS) related Kaposi sarcoma is common, but it is rarely seen in the absence of cutaneous disease.
Most patients with gastrointestinal involvement of Kaposi's sarcoma remain asymptomatic and are often diagnosed on endoscopy or autopsy. However, there are cases of KS mimicking ulcerative colitis (UC), whereby clinical manifestations can confuse physicians [8,9]. Therefore, it could pose a serious diagnostic challenge.
We report a case of a KS in homosexual man with AIDS that was originally presented and diagnosed as UC.
Case Presentation
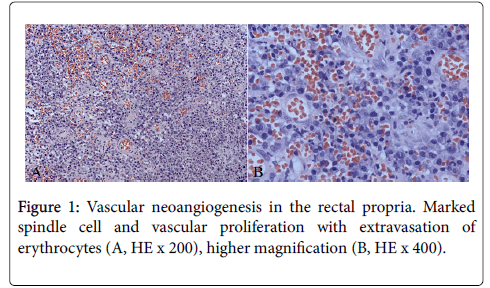
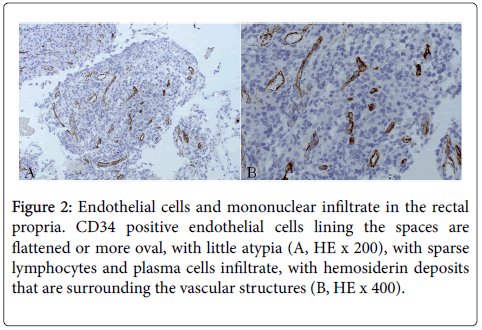
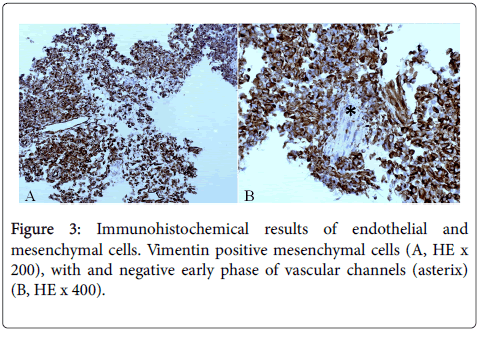
We report a 31-year-old homosexual man who presented with rectal pain and bleeding and was found to have Kaposi sarcoma in both skin and rectum. Patient was diagnosed eight years ago with HIV/AIDS, and was receiving highly active retroviral therapy (HAART). Despite treatment with HAART, he developed diffuse cutaneous, confluent and nodular red changes in the back, which were 1 cm in diameter, accompanied with pain and itching. During the last four months, he experienced rectal pain and bleeding. Patient also lost 15 kg of weight in the last six months, which he linked to vegan diet. During rectoscopy, confluent ulcerous, necrotic and hemorrhagic mucosal surface of 9 cm in size, along the entire rectum was found. Initial diagnosis was UC and tissue samples were collected for pathological examination. By using histological (HE), histochemical (AB-PAS) and immunohistochemical stains (CD34 and vimentin antibodies) we have found the following characteristics: marked spindle cell and vascular proliferation with extravasation of erythrocytes (Figures 1A and 1B). Endothelial cells lining the spaces are flattened, or more oval, with little atypia (Figure 2A). Granulocyte leukocytes in necrobiosis, sparse lymphocytes and plasma cells admixed with deposits of hemosiderin surrounding the vascular structures (Figure 2B). Immunohistohemical verification of endothelial and mesenchymal cells confirmed the Kaposi angiosarcoma diagnosis (Figures 3A and 3B). Endothelial cells show solid proliferation in early phase of neoangiogenesis (Figure 3B).
Figure 2: Endothelial cells and mononuclear infiltrate in the rectal propria. CD34 positive endothelial cells lining the spaces are flattened or more oval, with little atypia (A, HE x 200), with sparse lymphocytes and plasma cells infiltrate, with hemosiderin deposits that are surrounding the vascular structures (B, HE x 400).
Discussion
Kaposi sarcoma (KS) is a systemic disease that can present itself with cutaneous lesions with or without internal involvement [10]. KS can have four epidemiological variants: classic, African or endemic, iatrogenic or related to immunosuppressive treatment, and epidemic or AIDS-related [11]. HHV-8 is the main etiological agent of the four clinical-epidemiological forms of KS. The highest HHV-8 prevalence is recorded in groups with a high incidence of KS, such as sub-Saharan Africans, individuals in Mediterranean countries, and individuals who are infected with HIV. HHV-8 is mainly transmitted through sexual contact, although parenteral (blood-borne, organ transplantation) and horizontal transmission have also been reported mainly in areas where KS is endemic [12]. Through unclear mechanisms, co-infection with HIV and HHV-8 dramatically increases the incidence and progression of KS [13]. The evolution of diseases depends on its clinical extent and may range from very indolent forms to a rapidly progressive disease. It is also modified by treatment that includes surgery, radio- and chemotherapy. Early lesions may be subtle, showing only increased number of vascular channels accompanied by plasma cell infiltration [14]. Cases with widespread visceral involvement are commonly poorly responsive to treatment.
UC is a chronic inflammatory bowel disease that affects large bowel, causing inflammation and ulcers. Several case reports have been published highlighting the association of KS and UC [15-17]. Like in our case, the patients were presented with bloody or watery diarrhea, abdominal pain and weight loss.
The majority of cases of gastrointestinal KS (GI-KS) is asymptomatic, and for this reason, remains undiagnosed. Although GI-KS disease can be identified easily on endoscopy, in some situations it may resemble common benign lesions as well as malignant neoplasms (gastrointestinal stromal tumor, spindle cell melanoma, angiosarcoma) [18]. Therefore, biopsy specimens should be obtained to allow confirmatory testing with histopathology and immunohistochemistry testing [19]. In our case, the patient was previously diagnosed with HIV/AIDS, and despite the HAART he developed the skin lesions which were most notable on his back. Because of expressive rectal pain and bleeding, he underwent rectoscopy, which revealed ulcerous and hemorrhagic lesions. The rectoscopic and clinical presentation mimicked acute flare of UC, which was patient initial diagnosis. After histological, histochemical and immunhistochemical examination of the sampled tissue, KS diagnosis was confirmed.
Conclusion
The clinical manifestations of Kaposi sarcoma can be confused with acute exacerbation of ulcerative colitis often delaying the diagnosis. Therefore, early endoscopic evaluation with adequate biopsies could help in timely diagnosis and management of GI-KS.
Disclosure Statement
No competing financial interests exist
References
- Lamovec J, Knutila S (2002) Pathology and Genetics of Tumours of Soft Tissue and Bone. IARC Press 170-173.
- Boshoff C, Weiss R (2002) Aids-related malignancies. Nat Rev Cancer 2: 373–382.
- Rezaei M, Chavoshzadeh Z, Haroni N, Armin S, Navidinia M, et al. (2013) Colonization with Methicillin Resistant and Methicillin Sensitive Staphylococcus aureus Subtypes in Patients with Atopic Dermatitis and Its Relationship with Severity of Eczema. Arch Pediatr Infect Dis 1: 53-56.
- Navidinia M, Fallah F, Lajevardi B, Shirdoost M, Jamali J, et al. (2015) Epidemiology of Methicillin-Resistant Staphylococcus aureus Isolated From Health Care Providers in Mofid Children Hospital. Arch Pediatr Infect Dis 3: e16458.
- Navidinia M (2015) Detection of inducible clindamycin resistance (MLSBi) among methicillin-resistant Staphylococcus aureus (MRSA) isolated from health care providers. J Paramed Sci 6: 91-96.
- Navidinia M (2016) The clinical importance of emerging ESKAPE pathogens in nosocomial infections. J Paramed Sci 7: 43-57.
- Ioachim HL, Adsay V, Giancotti FR, Dorsett B, Melamed J (1995) Kaposi's sarcoma of internal organs. A multiparameter study of 86 cases. Cancer 75: 1376-1385.
- Kumar V, Soni P, Garg M, Abduraimova M, Harris J (2017) Kaposi Sarcoma Mimicking Acute Flare of Ulcerative Colitis. J Investig Med High Impact Case Rep 5: 2324709617713510.
- Biggs BA, Crowe SM, Lucas CR, Ralston M, Thompson IL, et al. (1987) AIDS related Kaposi’s sarcoma presenting as ulcerative colitis and complicated by toxic megacolon. Gut 28: 1302-1306.
- Penn I (1997) Kaposi’s sarcoma in transplant recipients. Transplantation 64: 669-673.
- Bhutani M, Polizzotto MN, Uldrick TS, Yarchoan R (2015) Kaposi sarcoma associated herpes virus-associated malignancies: Epidemiology, pathogenesis, and advances in treatment. Semin Oncol 42: 223–246.
- RodrÃguez-Peláez M, Fernández-GarcÃa MS, Gutiérrez-Corral N, de Francisco R, Riestra S, et al. (2010) Kaposi’s sarcoma: an opportunistic infection by human herpesvirus-8 in ulcerative colitis. J Crohns Colitis 4: 586-590.
- Schulz TF, Cesarman E (2015) Kaposi sarcoma-associated herpesvirus: Mechanisms ofoncogenesis. Curr OpinVirol 14: 116–218.
- Lubin J, Rywlin A (1971) Lymphoma-like lymph node changes in Kaposi's sarcoma. Two additional cases. Arch Pathol 92: 338-341.
- Kang MJ, Namgung KY, Kim MS, Ko BS, Han CS, et al. (2004) A case of Kaposi’s sarcoma associated with ulcerative colitis [in Korean]. Korean J Gastroenterol 43: 316-319.
- Meltzer SJ, Rotterdam HZ, Korelitz B (1987) Kaposi’s sarcoma occurring in association with ulcerative colitis. Am J Gastroenterol 82: 378-381.
- Kumar V, Soni P, Garg M, Abduraimova M, Harris J (2017) Kaposi Sarcoma Mimicking Acute Flare of Ulcerative Colitis. J Investig Med High Impact Case Rep 5: 1-4.
- Taccogna S, Crescenzi A, Stasi R, Turrini L, Gallo A, et al. (2009) Kaposi sarcoma of the stomach: a case report. BMJ Case Rep.
- Lee AJ, Brenner L, Mourad B, Monteiro C, Vega KJ, et al. (2015) Gastrointestinal Kaposi’s sarcoma: Case report and review of the literature. World J Gastrointest Pharmacol Ther 6: 89-95.
Citation: Katic V, Todorovic J, Nagorni A, Nagorni I, Micev M, et al. (2017) A Case of Kaposi's Sarcoma of the Rectum in a Homosexual Male with HIV–AIDS. J Infect Dis Ther 5:340. DOI: 10.4172/2332-0877.1000340
Copyright: © 2017 Katic V, et al. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.
Share This Article
Recommended Journals
Open Access Journals
Article Tools
Article Usage
- Total views: 6175
- [From(publication date): 0-2017 - Apr 28, 2025]
- Breakdown by view type
- HTML page views: 5313
- PDF downloads: 862