Case Report Open Access
A Case of Choledochocele Unclassifiable by Sarris’s Classification Characterized by the Serial Images of Endoscopic Retrograde Cholangiopancreatography [ERCP]
Kenji Sasaki*
Department of Internal Medicine, Shiogama City Hospital, Shiogama, Japan
- *Corresponding Author:
- Kenji Sasaki
Department of Internal Medicine, Shiogama City Hospital
7-1, Kouzumachi, Shiogama, Miyagi, 985-0054, Japan
Tel: +81-22-364-5521
Fax: +81-22-364-5529
E-mail: kydosarnymai@aria.ocn.ne.jp
Received date: September 09, 2014; Accepted date: October 20, 2014; Published date: October 27, 2014
Citation: Sasaki K (2014) A Case of Choledochocele Unclassifiable by Sarris’s Classification Characterized by the Serial Images of Endoscopic Retrograde Cholangiopancreatography [ERCP]. J Gastrointest Dig Syst 4:234. doi:10.4172/2161-069X.1000234
Copyright: © 2014 Sasaki K, This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.
Visit for more related articles at Journal of Gastrointestinal & Digestive System
Abstract
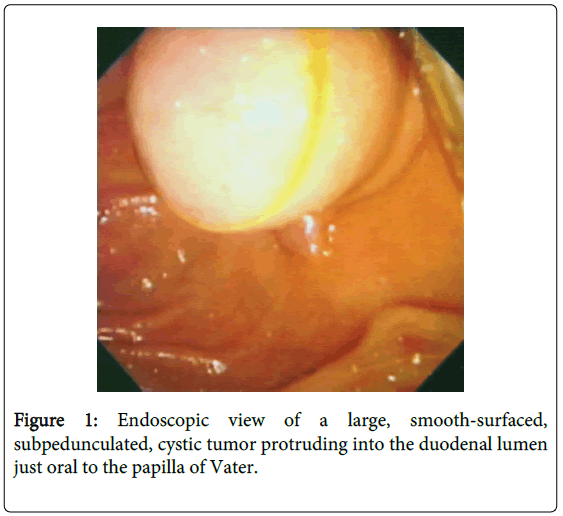
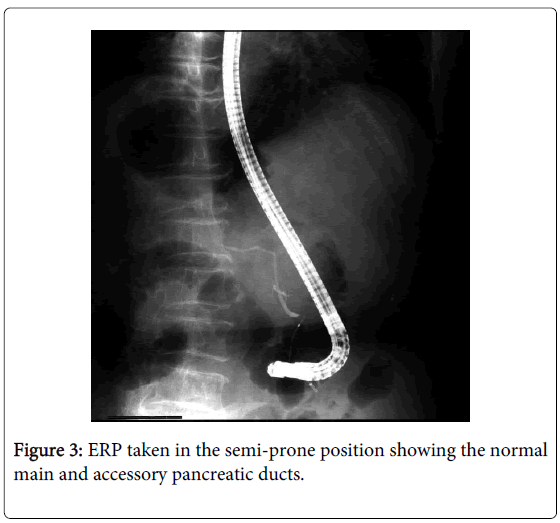
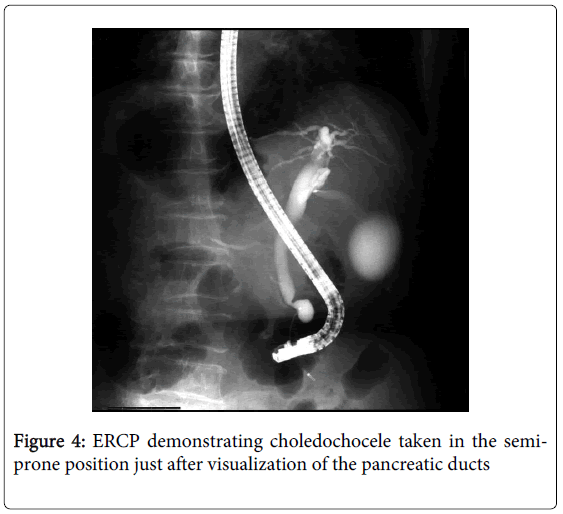
A 74-year-old Japanese housewife was shown to have a large, smooth-surfaced, protruding, subpedunculated tumor covered with the normal-appearing mucosa on the posteromedial wall of the mid descending part of the duodenum immediately oral to the papilla of Vater by endoscopy. ERCP demonstrated the normal main and accessory pancreatic ducts. Just after abruptly contracted, the terminal common bile duct [CBD] showed a piriform dilatation correspondent to the duodenal tumor and tapered off to drain into the duodenal lumen without forming a common channel but through the same papillary orifice with the main pancreatic duct [MPD]. She was diagnosed with choledochocele unclassifiable by Sarris’s categorization. Even fully distended by infusion of contrast medium, the cyst did not compress the MPD. Remaining asymptomatic, the lesion was left untreated. She has kept an uneventful course for 4 years ever since. It is important to characterize the topographic relationships of the cyst among the surrounding structures in order to definitely classify the anomaly and to predict development of probable complications by analyzing the serial images of ERCP.
Keywords
Choledochal cyst; Choledochocele; ERCP; Classification of choledochocele
Introduction
Choledochal cyst in general is a relatively rare, congenital anomaly with particular female predominance [1-4]. Though used to be characteristically diagnosed in infancy and childhood [2,3], it has currently been more commonly recognized in adults [3,4]. It is classified into 5 types according to the anatomical location and shape of the cyst [5]. Type III cyst or choledochocele has peculiar characteristics among them: it is depicted as a dilatation of the distal CBD protruding to the duodenal lumen [6-8], it is extremely rare [2], and it has no gender preponderance [8]. It sometimes engenders pancreatitis [7-13], obstructive jaundice [7,8,11-15], cholangitis [12-14], and cholelithiasis [6,11,13,16] and rarely intestinal intussusception [16] and intracystic carcinoma [17,18]. It is categorized according to its anatomical relationships among the CBD, MPD, and papilla of Vater [6-8], which influence development of the complications mentioned above.
This report presents a case of choledochocele explicitly characterized by the serial images of ERCP, which is not interpreted as falling under Sarris’s classification.
Case Report
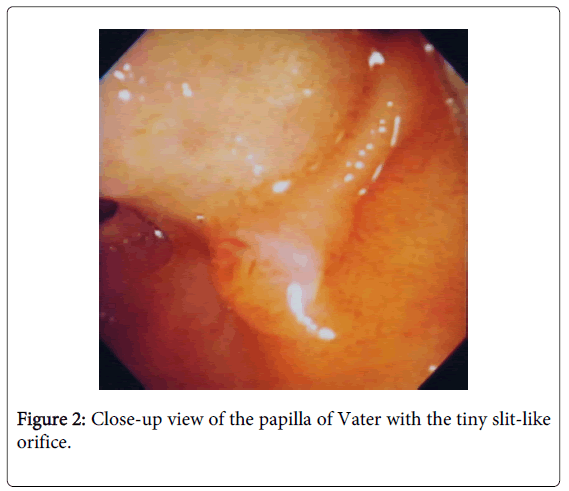
A 74-year-old Japanese housewife was shown to have a white ulcer scar on the superior wall of the duodenal bulb and a large, smooth-surfaced, bulging, subpedunculated, cystic tumor covered with the normal-appearing mucosa on the posteromedial wall of the mid descending part of the duodenum at the location of the oral protrusion (Figure 1) just oral to the small papilla of Vater with the tiny slit-like orifice (Figure 2) by esophagogastroduodenoscopy. A diagnosis of choledochocele was entertained.
She had a subpedunculated tumor on the medial wall of the distal ascending colon endoscopically excised several days before. Pathological examination revealed it to be a moderately differentiated adenocarcinoma invading 2,000 µm into the submucosa with an adenomatous component in the periphery. The horizontal and vertical margins were free of malignancy and no venous or lymphatic invasion was detected. Since 12.5% of such a cancer has lymph node metastasis according to the statistical data [19], she was undergoing the preoperative examinations for additional colectomy with lymph node dissection.
Though she had hypertension, type 2 diabetes mellitus, and post-hepatitic cirrhosis attributed to hepatitis C virus [HCV] she was presumed infected with through transfused blood, when she was hysterectomized for myoma uteri at her 5th decade, and suffered from duodenal ulcer at the age of 70, her other past history was non-contributory. She had no family history of pancreatobiliary diseases, either. Laboratory data showed mild liver dysfunction, pancytopenia, and high-titered circulating 1b-typed HCV RNA but no hyperamylasemia or hyperbilirubineia.
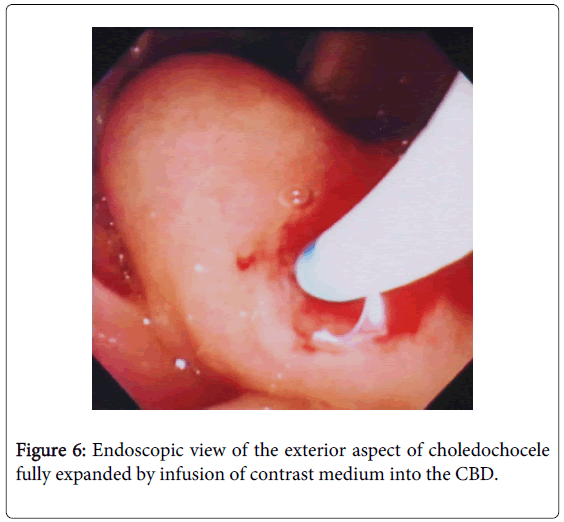
Endoscopic retrograde pancreatography [ERP] taken in the semi-prone position demonstrated the normal main and accessory pancreatic ducts (Figure 3). Endoscopic retrograde cholangiography [ERC] photographed in the same position just after ERP clearly visualized a piriform dilatation of the terminal CBD correspondent to the cystic tumor of the duodenum immediately subsequent to abrupt constriction in the duodenal wall (Figure 4). The topographic relationships of the cystic dilatation among its surrounding structures were thoroughly revealed by the photograph taken in the supine position immediately after completion of infusion of contrast medium (Figure 5): the terminal CBD, after shaping a pear-shaped cyst protruding into the duodenal lumen just like a diverticulum, which was observed getting expanded beyond the papilla by infusion of contrast medium into the CBD during ERC (Figure 6), tapered off to drain out into the duodenal lumen without forming a common channel but through the same papillary orifice with the smoothly tapering MPD. Even totally distended, the cyst did not compress the MPD at all (Figures 4 and 5). No pancreatobiliary malunion [PBM] was detected (Figure 5). Though the gallbladder was remarkably dilated, no other abnormalities were detected in the biliary system. She was definitely diagnosed as having choledochocele unclassifiable by Sarris’s categorization.
Computed tomography [CT] showed no hepatic or lymph node metastases. Since she had severe thrombocytopenia attributed to cirrhosis, she finally refused to undergo additional colectomy. Remaining asymptomatic, the choledochocele was also left untreated. She has had an uneventful course during the 4-year follow-up period.
Discussion
Choledochocele is an extremely rare, congenital anomaly, classically depicted as a dilatation of the distal CBD bulging to the duodenal lumen [6-8]. Distension of the cyst would lead to colicky pain and stasis of bile in the lesion would result in obstructive jaundice, cholangitis, or cholelithiasis. Contingent on the anatomical relationships of the cyst among the CBD, MPD, and papilla of Vater, interference with flow of the pancreatic secretion or its regurgitation into the biliary system would be likely to occur, which predisposes a subject to develop pancreatitis or malignancy, respectively.
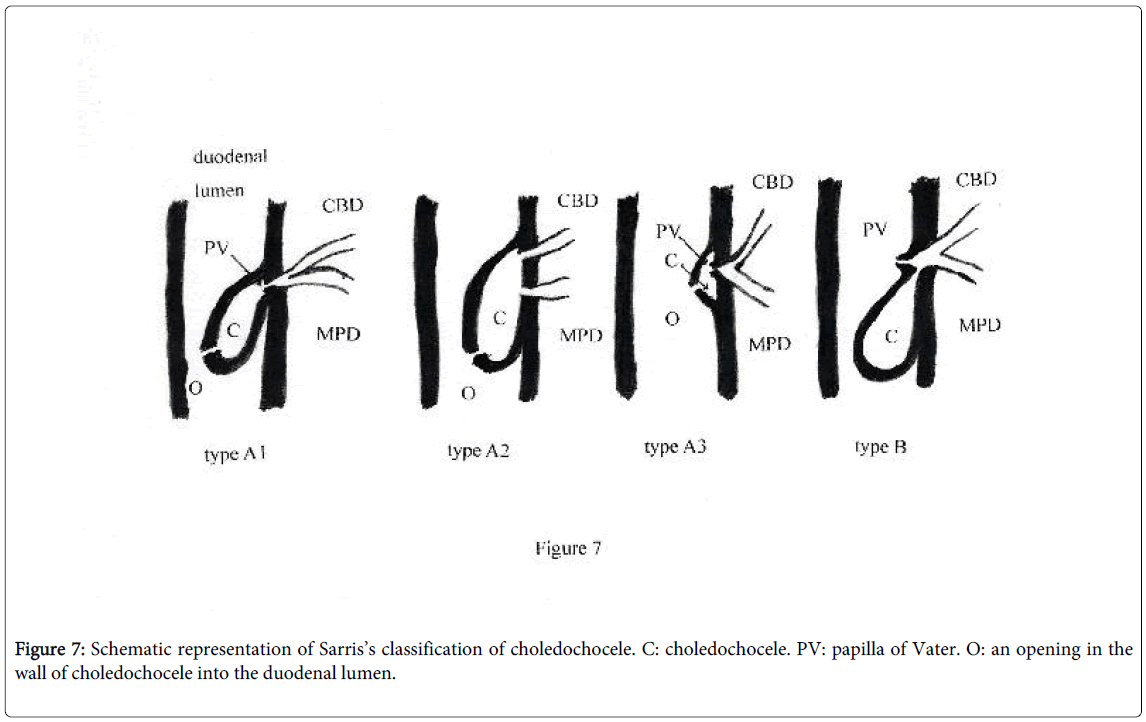
Scholz et al. defined the anomaly as herniation of the CBD into the duodenum, classifying it into 2 types according to its anatomical pattern [6]. Then Greene et al. subdivided Scholz’s type A into 3 groups, recommending sphincteroplasty for management of the third type [intramural choledochocele] associated with recurrent pancreatitis [7]. Combining the above 2 classifications, Sarris et al. categorized the lesion into 4 groups with therapeutic implications [8] (Figure 7). The MPD and CBD terminate in choledochocele which drains directly into the duodenal lumen through the aperture in its wall other than the papilla of Vater in type A. It is further subdivided into A1 to A3. While types A1 and A2 present themselves in the intraluminal duodenum, type A3 is contained within the intramural portion of the duodenum. The MPD and CBD, after forming a common channel, drain into choledochocele in type A1, whereas they have separate openings into it in type A2. In type B, choledochocele protruding into the duodenal lumen drains into the intramural portion of the common channel and out through the papilla of Vater. Partial cyst excision, sphincteroplasty, or both are recommended for treatment of the anomaly depending on the anatomical type [8].
In the present case, the terminal CBD, immediately after abruptly contracted in the duodenal wall, showed a piriform dilatation protruding into the duodenal lumen just like a diverticulum distinctly corresponding to the cystic tumor of the duodenum, which was stretched particularly more anally by infusion of contrast medium into the CBD, and then tapered off to drain out into the duodenal lumen separately from without forming a common channel but via the same papillary orifice with the MPD. Though definitely fulfills the diagnostic criterion of choledochocele, it is by no means covered by the above classification. Ohtsuka et al. classified the anomaly into 2 types [18] and Kagiyama et al. into 5 types [20], adding 3 new types to Scholz’s classification, to none of which the present case belongs.
Horaguchi et al. classified choledochocele into 2 types, interpreting the serial images during ERCP [21]. In type I, the distal CBD, after forming choledochocele, drains out into the duodenal lumen separately from or just after forming a common channel with the MPD, whereas in type II, both the MPD and CBD terminate in choledochocele, which, serving as a common channel, opens into the duodenal lumen through the papilla of Vater. The present case comes under their type I because, after shaping choledochocele, the CBD opens into the duodenal lumen separately from without forming a common channel but through the same papillary orifice with the MPD. They reported increased amylase content in the CBD not only in type II but also in some cases of type I, speculating upon the presence of abnormal functional arrangement in the pancreatobiliary ductal system in the latter type [21]. It is absolutely obligate to document the presence or absence of a common channel, however difficult it may be. Reflux of the pancreatic secretion into the CBD is not considered to occur in the absence of a common channel.
The anatomical relationships of choledochocele among the surrounding structures were explicitly depicted by the serial images of ERCP in the present case. From the topographic perspective, the present case has no theoretical possibility of developing malignancy because of pancreatobiliary reflux through the nonexistent PBM or pancreatitis, because the cyst, even maximally dilated, is located too distant from the MPD to interfere with flow of the pancreatic secretion. It is considered remaining less swollen in the usual state, as expected from the findings during ERCP. Further expansion of choledochocele during infusion of contrast medium into the CBD was also reported [10] so that obstruction of the pancreatic secretion or bile should be evaluated under the circumstances, in which the cyst is maximally distended. Since the present case had no possibility of developing complications except those due to possible bile stagnation in the light of the topographic relationships and remained asymptomatic, the cyst was left untreated and followed up. Such a strategy is warranted for management of the asymptomatic cases [10,13].
In conclusion, the present case is not covered by Sarris’s classification. It is critically important to characterize the topographic relationships of the anomaly among the surrounding structures in order to precisely classify the cyst and to predict development of probable complications by analyzing the serial images of ERCP exquisitely taken.
References
- Jones PG, Smith ED, Clarke AM, Kent M (1971) Choledochal cysts: experience with radical excision. J Pediatr Surg 6: 112-120.
- Yamaguchi M (1980) Congenital choledochal cyst. Analysis of 1,433 patients in the Japanese literature. Am J Surg 140: 653-657.
- Lopez RR, Pinson CW, Campbell JR, Harrison M, Katon RM (1991) Variation in management based on type of choledochal cyst. Am J Surg 161: 612-615.
- Lipsett PA, Pitt HA, Colombani PM, Boitnott JK, Cameron JL (1994) Choledochal cyst disease. A changing pattern of presentation. Ann Surg 220: 644-652.
- Todani T, Watanabe Y, Narusue M, Tabuchi K, Okajima K (1977) Congenital bile duct cysts: Classification, operative procedures, and review of thirty-seven cases including cancer arising from choledochal cyst. Am J Surg 134: 263-269.
- Scholz FJ, Carrera GF, Larsen CR (1976) The choledochocele: correlation of radiological, clinical and pathological findings. Radiology 118: 25-28.
- Greene FL, Brown JJ, Rubinstein P, Anderson MC (1985) Choledochocele and recurrent pancreatitis. Diagnosis and surgical management. Am J Surg 149: 306-309.
- Sarris GE, Tsang D (1989) Choledochocele: case report, literature review, and a proposed classification. Surgery 105: 408-414.
- Goldberg PB, Long WB, Oleaga JA, Mackie JA (1980) Choledochocele as a cause of recurrent pancreatitis. Gastroenterology 78: 1041-1045.
- Venu RP, Geenen JE, Hogan WJ, Dodds WJ, Wilson SW, et al. (1984) Role of endoscopic retrograde cholangiopancreatography in the diagnosis and treatment of choledochocele. Gastroenterology 87: 1144-1149.
- Marshall JB, Halpin TC (1982) Choledochocele as the cause of recurrent obstructive jaundice in childhood: diagnosis by ERCP. Gastrointest Endosc 28: 88-90.
- Martin RF, Biber BP, Bosco JJ, Howell DA (1992) Symptomatic choledochoceles in adults. Endoscopic retrograde cholangiopancreatography recognition and management. Arch Surg 127: 536-538.
- Masetti R, Antinori A, Coppola R, Coco C, Mattana C, et al. (1996) Choledochocele: changing trends in diagnosis and management. Surg Today 26: 281-285.
- Yamaoka K, Tazawa J, Koizumi K, Asahina Y, Tajiri K, et al. (1994) Choledochocele with obstructive jaundice: a case report and a review of the Japanese literature. J Gastroenterol 29: 661-664.
- Cohen F, Bernstein JR (1981) Choledochocele presenting with jaundice. Diagnosis by percutaneous cholangiogram. Dig Dis Sci 26: 667-670.
- Ramos A, Castelló J, Pinto I (1990) Intestinal intussusception as a presenting feature of choledochocele. Gastrointest Radiol 15: 211-214.
- Ozawa K, Yamada T, Matumoto Y, Tobe R (1980) Carcinoma arising in a choledochocele. Cancer 45: 195-197.
- Ohtsuka T, Inoue K, Ohuchida J, Nabae T, Takahata S, et al. (2001) Carcinoma arising in choledochocele. Endoscopy 33: 614-619.
- Japanese Society for Cancer of the Colon and Rectum (2014) JSCCR guidelines 2014 for the treatment of colorectal cancer. Kanahara Shuppan, Tokyo. (in Japanese)
- Kagiyama S, Okazaki K, Yamamoto Y, Yamamoto Y (1987) Anatomic variants of choledochocele and manometric measurements of pressure in the cele and the orifice zone. Am J Gastroenterol 82: 641-649.
- Horaguchi J, Fujita N, Kobayashi G, Noda Y, Ito K, et al. (2005) Clinical study of choledochocele: is it a risk factor for biliary malignancies? J Gastroenterol 40: 396-401.
Relevant Topics
- Constipation
- Digestive Enzymes
- Endoscopy
- Epigastric Pain
- Gall Bladder
- Gastric Cancer
- Gastrointestinal Bleeding
- Gastrointestinal Hormones
- Gastrointestinal Infections
- Gastrointestinal Inflammation
- Gastrointestinal Pathology
- Gastrointestinal Pharmacology
- Gastrointestinal Radiology
- Gastrointestinal Surgery
- Gastrointestinal Tuberculosis
- GIST Sarcoma
- Intestinal Blockage
- Pancreas
- Salivary Glands
- Stomach Bloating
- Stomach Cramps
- Stomach Disorders
- Stomach Ulcer
Recommended Journals
Article Tools
Article Usage
- Total views: 16202
- [From(publication date):
December-2014 - Apr 03, 2025] - Breakdown by view type
- HTML page views : 11612
- PDF downloads : 4590