A Case of Bronchiectasis in Patient with Ulcerative Colitis
Received: 21-Jun-2018 / Accepted Date: 30-Jul-2018 / Published Date: 06-Aug-2018
Keywords: Intestinal disease; Inflammatory disease; Ulcerative colitis; Respiratory disease; Bronchiectasis; Inhaled corticosteroids therapy.
Introduction
The association of respiratory disorders with enteric diseases (Crohn’s disease (CD) and ulcerative colitis (UC)) is uncommon but well recognized. Patients with ulcerative colitis may have a presentation dominated by extra-intestinal manifestations. Pulmonary manifestations of ulcerative colitis have been reported, but incidence of bronchiectasis is rare.
Case Observation
A 57-year-old non-smoker male was admitted to the intensive care unit for a moderate acute respiratory failure secondary to an exacerbation of his chronic pulmonary disease. The patient is known to have a chronic respiratory failure resulting from bronchiectasis evolving since 15 years with a chronic dyspnea stage 4 SADOUL. He also have had an ulcerative colitis discovered 13 years ago stabilized with salazopyrin without colectomy and he has been nephrectomized since 5 months because of an atrophic kidney with no clear etiology.
This patient has been splenectomized 43 years ago following a road accident. One week ago, he presented an acute exacerbation of his pulmonary disease triggered by a tracheobronchitis with increased sputum purulence and volume. On examination, he had fever and bronchial yellowish secretions with signs of respiratory distress: dyspnea, polypnea at 30 c/min and bilateral wheezing at the auscultation and edema of the lower limbs.
The hemogram showed no anemia (hemoglobin: 13.5 g/dl), leukocytosis (WBC/ 18800 with predominance of PNN) and normal platelets (373000). Ddimer assey results perform at the emergency room before admission for a suspicion of pulmonary embolism showed normal range with 420 μgr/l. Arteriel blood gases measured at room air revealed a moderate respiratory alcalosis with pH 7.44, PaCO2 27 mm Hg, HCO3: 24 mmol/l, and there was no hypoxemia (PaCO2 72 mm Hg, oxygen saturation of 94%) . concerning gazometry, the patient was in a moderate acute respiratory failure with obstructive disorder (attested by wheezing) so the PH was initially perturbated (alcalosis: compensation with polypnea) and in front of the work of breath non-invasive ventilation was performed.
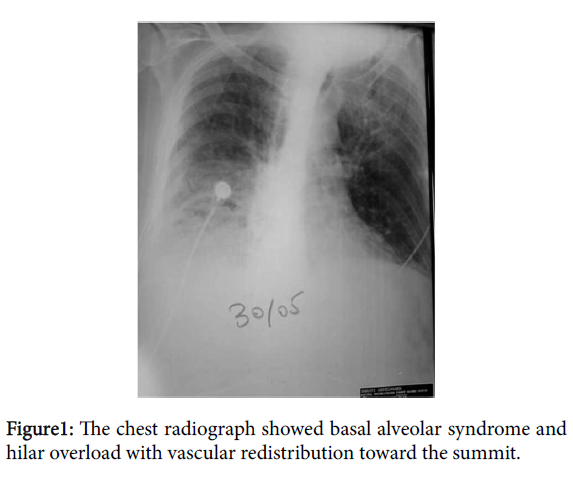
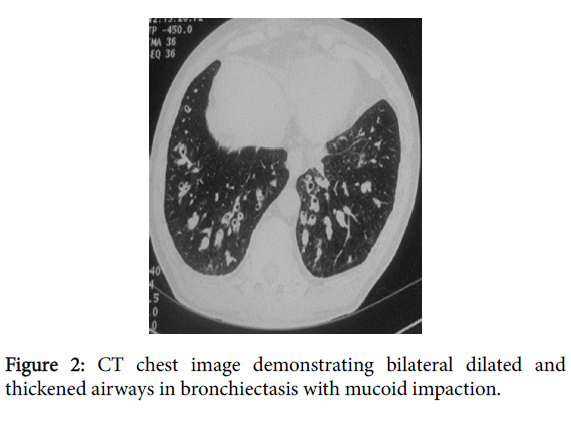
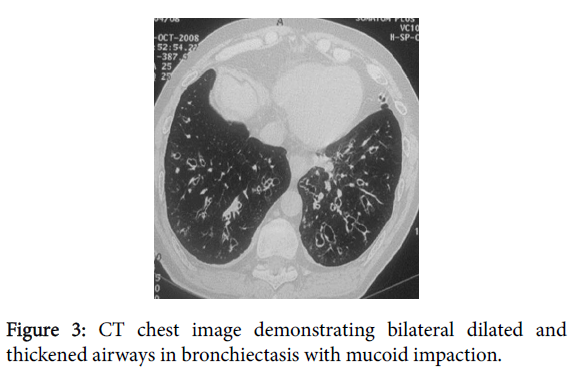
The chest x-ray taken upon admission revealed basal alveolar syndrome and hilar overload with vascular redistribution toward the summit related probably to an acute edema of the lungs (Figure 1). Thoracic computed tomography (CT) examination performed 24 hours before admission in the emergency room to eliminate pulmonary embolism objectived bilateral bronchial dilatations some of which are filled with mucoid impaction and having thickened walls Figure 2, associated with trendy micronodules evidence of superinfected bronchial dilatation (Figure 3).
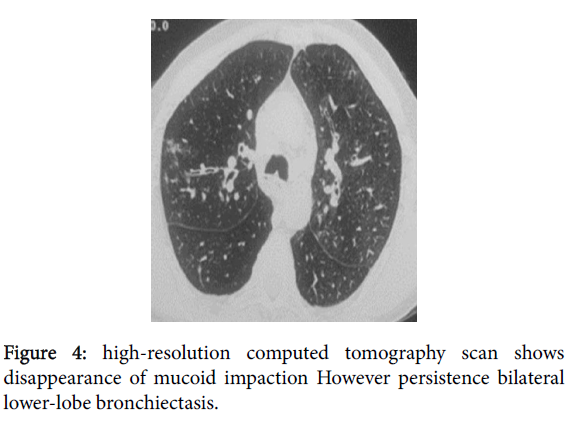
The patient was initially treated with non-invasive ventilation (NIV), antibiotherapy by cefotaxime and ciprofloxacin and corticosteroids. In front of the failure of NIV the patient was intubated and sedated with propofol and remifentanyl.the weaning procedure was difficult in front of the persistence of pulmonary edema, the low urinary output and a tachycardia at a mean of 120b/min; an echocardiography was performed and showed a moderate low left ventricular ejection at 45% leading to the adjunction of digoxin as inotrop agent. A significant improved was obtained and the patient was successfully ex-tubated 3 days after. The suites were favourable and the patient left the hospital after 20 days of hospitalization with beclomethasone diproprionate by aerosol. Chest CT control objectified a radiological cleaning of mucoid impaction (Figure 4).
Discussion
Various respiratory manifestations have been reported in association with ulcerative colitis, albeit in a sporadic pattern. These include bronchiolitis obliterans, bronchitis, pleuritis, lung vascular involvement, bronchiectasis, inflammatory tracheal stenosis, chronic pneumonia and interstitial pneumonia [1]. Drug induced pneumonia due to sulfasalazin and mesalamin are so exceptional [2]. The first respiratory manifestation which has been reported was by Kraft in 1976 [3]. In a review of the literature including 33 well detailed cases with inflammatory bowel disease (IBD) and pulmonary manifestations, bronchiectasis was seen in six of the 28 patients with ulcerative colitis, including three who developed severe bronchopulmonary suppuration a few days or weeks after colectomy [4,5]. Complications and extra intestinal manifestations may precede or follow the diagnosis of IBD and may occur either with exacerbations of bowel symptoms or independently [1]. Generally, they occur after the onset of the colitis, particularly after colectomy [2]. It has been suggested that, following colectomy, the bronchial tree (which has the same embryological origin as the bowel) becomes the new epitopic target for the immune system [5]. The pathogenesis of respiratory complications in IBD without colectomy is largely unknown though postulated links including infiltration of the air way by immune effector cells such as lymphocytes enhanced immune activity as a part of the underlying disease [1]. The causal relationship between bronchiectasis and UC is always difficult to prove. In favour of this relationship, the late onset of bronchiectasis in adults, the occurrence after the discovery of the UC and especially after colectomy, lack of respiratory history and smoking and favourable outcome with corticosteroids. Bronchoscopy usually shows an inflammatory aspect of the mucosa, sometimes associated with bronchial stenosis secondary to edema and inflammation. The identification of histological lesions in the lungs recalling the intestinal lesions of UC is consoliding this relationship. Finally, the presence of antinuclear antibodies would be more common in UC with respiratory illness. However, the significance of their demonstration to be determined [6,7].
Conclusion
Considering this observation, we recommend that in approach to a bronchiectatic patient, every clinical history of abdominal pain or rectorrhagy must necessitate ruling out the inflammatory bowel disease. Early detection is important as both the pulmonary and gastrointestinal manifestations often respond well to steroids. Furthermore, the diagnosis of bronchiectasis should be considered in any newly installed and persistent respiratory symptoms in a patient with ulcerative colitis.
References
- Xiao-Qing Ji, Li-Xia W, De-Gan Lu (2014) Pulmonary manifestations of inflammatory bowel disease. World J Gastroenterol 20: 13501-13511.
- Abbas Ali O, Davood A, Saeedeh SS, Hooman T (2005) An Unusual Presentation of Ulcerative Colitis in a Young Girl: A Case Report. Tanaffos 4: 71-74.
- Charfi MR, Dougui MH, Bazar NB, Boubaker S, Zbiba M, et al. (1999) Belalgia. Bronchectasies chez un patient porteur d'une rectocolite ulcéro-hémorragique. Revue des Maladies Respiratoires 16: 846.
- Kraft SC, Earle RH, Roesler M, Esterly JR (1976) Unexplained bronchopulmonary disease with inflammatory bowel disease. Arch Intern Med 136: 454-459.
- Camus P, Piard F, Ashcroft T, Gal AA, Colby TV (1993) The lung in inflammatory bowel disease. Medicine (Baltimore) 72:151–183.
- Eaton TE, Lambie N, Wells AU (1998) Bronchiectasis following colectomy for Crohn’s disease. Thorax 53: 529-531.
- Alcázar Navarrete B, Quiles Ruiz-Rico N, González Vargas F, Cabrera Torres L (2005) Bronchiectasis Following Colectomy in a Patient WithUlcerative Colitis and Factor V Leiden Mutation. Arch Bronconeumol. 41: 230-232.
Citation: Majdoub S, Bouzayene F, Chouchene I, Gargouri I, Zaghouani H, et al. (2018) A Case of Bronchiectasis in Patient with Ulcerative Colitis. J Respir Med 2: 108.
Copyright: © 2018 Majdoub S, et al. This is an open-access article distributed under the terms of the Creative Commons Attribution License; which permits unrestricted use; distribution; and reproduction in any medium; provided the original author and source are credited.
Share This Article
Recommended Journals
Open Access Journals
Article Usage
- Total views: 4266
- [From(publication date): 0-2018 - Dec 31, 2024]
- Breakdown by view type
- HTML page views: 3564
- PDF downloads: 702