A Case of Anti-N-Methyl-D-Aspartate Receptor Encephalitis Triggered by Herpes Simplex Virus Encephalitis
Received: 24-Nov-2017 / Accepted Date: 05-Dec-2017 / Published Date: 07-Dec-2017 DOI: 10.4172/2314-7326.1000270
Abstract
In recent years, more and more medical researchers realized that anti-N-methyl-D-aspartate receptor (NMDAR) encephalitis can be triggered by herpes simplex encephalitis (HSE), which can lead to an immune-mediated relapse. There are some different characteristics of Anti-NMDAR encephalitis after HSE and viral encephalitis. Here we report a case of Anti-NMDAR encephalitis after HSE who with movement disorders, autonomic nervous dysfunction and extreme delta brush (EDB) in electroencephalogram (EEG).
Keywords: Herpes simplex virus; Immune-mediated relapse; Autonomic nervous dysfunction
Introduction
Anti-N-Methyl-D-Aspartate receptor encephalitis is a type of in lammation of brain which can be lethal if remains untreated. Whereas herpes simplex encephalitis (HSE) is the encephalitis caused by virus infection in central nervous system. Here we report a case of a 20-year-old Chinese male student where anti-N-methyl-D-aspartate receptor (NMDAR) encephalitis as triggered by herpes simplex encephalitis.
Case Report
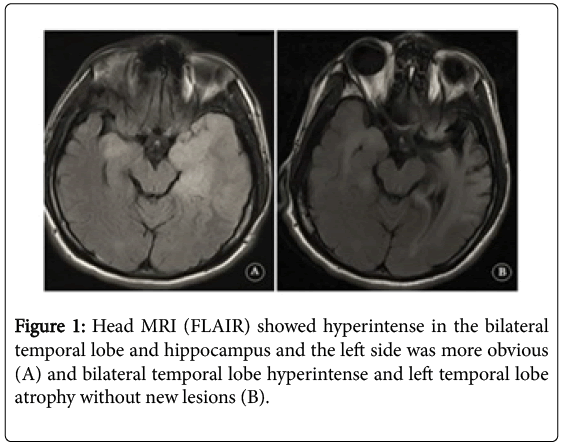
A 20-year-old Chinese male student developed a sense of smell disorder and fatigue a ter exercising. T e oral temperature was 38.3 degrees centigrade and serum leukocyte was 10.79 × 109/L (neutral 80.4%), so he was given oral antibiotics. T e next day he appeared headache, vomiting, coma and cerebrospinal luid (CSF) showed pressure 260 mmH2O, 8 leukocytes/ul (88% lymphocytes), 6 erythrocytes/ul, protein 923 mg/L, glucose 3.2 mmol/L. Head MRI showed hyperintense on T2-weighted imaging
(T2WI)/ luid attenuated inversion recovery (FLAIR) in the bilateral temporal lobe and hippocampus and the le t side was more obvious (Figure 1A). Anti-N-methyl-D-aspartate (NMDA) receptor antibody in serum and CSF were negative. Electroencephalogram (EEG) showed slow waves. He was diagnosed with herpes simplex virus encephalitis (HSE) and given dexamethasone, ganciclovir, and mannitol for two weeks and recovered with a slightly lower memory.
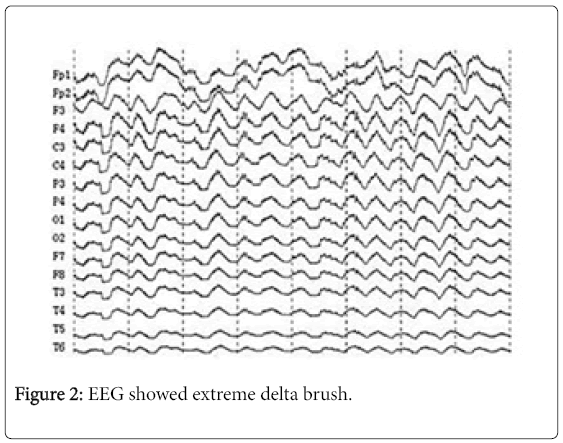
A ter 19 days, he developed insomnia and speech disorder and the next day he was silent. His right hand was moving disorderly and mouth was squirming “rabbit like“mouth movement. He’s in hospital again and blood leukocyte was 10.22 × 109/L (neutral 84.2%), CSF showed pressure 240 mmH2O, 2 leukocytes/ul (82% lymphocytes), protein 523 mg/L, glucose 3.8 mmol/L. CSF oligoclonal showed that IgG was synthesized in the scabbard, the oligoclonal band (OB)number of CSF was greater than serum and monoclonal antibody was found in CSF. The immunological parameters of CSF were significantly increased and several IgG bands different from serum were visible in it. NMDA receptor antibody was strongly positive in CSF and weak positive in serum. Head MRI showed bilateral temporal lobe hyperintense and left temporal lobe atrophy without new lesions on T2MI/FLAIR (Figure 1B). EEG showed extreme delta brush EDB (Figure 2). He had a great sweat and heart rate during the process of hospitalization which was considered autonomic nervous dysfunction. Three courses of immunoglobulins (0.4 g/kg.d) and methylprednisolone started at 500 mg/d were given, followed by a gradual reduction of methylprednisolone. He was also treated with the left ethylalanine, valproate and phenobarbital for movement disorders. After 3 months, although still left memory decline sequelae, he could walk, and the movement disorder of the right hand and mouth disappeared.
Discussion
There have been reported cases of anti-NMDA receptor encephalitis and HSE was considered a precursor to it since the first report in 2012 [1-3]. Now the more acceptable mechanism is a viral infection of the central nervous system, especially the herpes simplex virus (HSV) infection, leads to severe inflammation of the peripheral lobe and tissue necrosis which causes NMDA receptor antigenic determinant exposure and activate autoimmune response. The anti-NMDA receptor antibody produced in the central nervous system can also enter peripheral blood through the damaged blood-brain barrier and causes the antibody to be positive in the blood.
The main symptoms of anti-NMDA receptor encephalitis include mental symptoms, seizures, cognitive dysfunction, movement disorders, abnormal behavior, autonomic nerve dysfunction, low ventilation, etc. Some of these symptoms are similar to viral encephalitis and another are specific, such as movement disorders, autonomic nerve dysfunction and low ventilation. A report analyzed the distinct differences in the clinical manifestations of autoimmune relapse after HSE between adults and children, which found the latter were more likely to develop choreoathetosis and decreased conscious level [4]. And case reports of adult developing movement disorders were rare [4]. Autonomic nervous dysfunction, such as cardiac arrhythmia, abnormal sweating, changes in respiratory frequency, and retention of urine are also specific manifestations of anti-NMDA receptor encephalitis and the mechanism may be disorders of the hypothalamus.
EDB have been recently described as a unique EEG phenomenon in anti NMDA receptor encephalitis [5]. Schmidt et al. reported seven of 23 patients with anti-NMDA receptor encephalitis had a EEG pattern characterized by rhythmic delta activity at 1-3 Hz with superimposed bursts of rhythmic 20-30 HZ beta frequency activity “riding “on each delta wave [6].
There are two kinds of typical symptoms (movement disorders, autonomic nervous dysfunction) in our patient and whose EEG shows EDB, which is a rare case report about anti-NMDA receptor encephalitis relapse after HSE. Compared with HSE, CSF routine examination and head MRI generally have no special performance.
Conclusion
This case indicates clinicians when symptoms of encephalitis appear again in patients recover from HSE, especially movement disorders, autonomic nerve dysfunction, EDB of EEG, NMDA receptor antibody should be tested in time.
References
- Pruss H, Finke C, Holtje M, Hofmann J, Klingbeil C, et al. (2012) N-methyl-D-aspartate receptorantibodies in herpes simplex encephalitis.Ann Neurol72:902-911.
- Morris NA, Kaplan TB,Linnoila J, Cho T (2016) HSV encephalitis-induced anti-NMDAR encephalitis in a 67-year-old woman: Report of a case and review of the literature.J Neurovirol22:33-37.
- Schein F,Gagneux-Brunon A,Antoine JC, Lavernhe S, Pillet S, et al. (2017) Anti-N-methyl-daspartate receptor encephalitis after Herpessimplex virus-associated encephalitis: an emerging diseasewith diagnosis and therapeutic challenges. Infection45:545-549.
- Armangue T, Moris G, CantarÃn-Extremera V, Conde CE, Rostasy K, et al. (2015) Autoimmune post-herpes simplex encephalitis of adults and teenagers.Neurology85:1736-1743.
- Veciana M, Becerra JL, Fossas P, Muriana D, Sansa G, et al. (2015) EEGextreme delta brush: An ictal pattern in patients with anti-NMDA receptorencephalitis. Epilepsy Behav49:280–285.
- Schmitt SE, Pargeon K, Frechette ES, Hirsch LJ, Dalmau J, et al. (2012) Extreme delta brush: A unique EEG pattern in adults with anti-NMDA receptor encephalitis. Neurology79: 1094-1100.
Citation: Jin X, Ye X (2017) A Case of Anti-N-Methyl-D-Aspartate Receptor Encephalitis Triggered by Herpes Simplex Virus Encephalitis. J Neuroinfect Dis 8: 270. DOI: 10.4172/2314-7326.1000270
Copyright: 2017 Jin X, et al. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution and reproduction in any medium, provided the original author and source are credited.
Share This Article
Recommended Journals
Open Access Journals
Article Tools
Article Usage
- Total views: 6405
- [From(publication date): 0-2017 - Nov 21, 2024]
- Breakdown by view type
- HTML page views: 5706
- PDF downloads: 699