Research Article Open Access
A Case Control Study to Identify the Risk Factors of Periodontitis in Pregnant Women in District Faisalabad
Saher Yousaf*, Mansur-ud-Din Ahmed, Muhammad Asif, Shumila Yousaf and Shazia Munir
Department of epidemiology and public health, University of veterinary and animal sciences, Lahore, Pakistan
- Corresponding Author:
- Yousaf S
Department of epidemiology and public health
University of veterinary and animal sciences, Lahore, Pakistan
Tel: +92-42-99211374
E-mail: yousafsaher@gmail.com
Received Date: May 19, 2016; Accepted Date: September 30, 2016; Published Date: October 07, 2016
Citation: Yousaf S, Ahmed MD, Asif M, Yousaf S, Munir S (2016) A Case Control Study to Identify the Risk Factors of Periodontitis in Pregnant Women in District Faisalabad. Occup Med Health Aff 4:247. doi:10.4172/2329-6879.1000247
Copyright: © 2016 Yousaf S, et al. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.
Visit for more related articles at Occupational Medicine & Health Affairs
Abstract
Good oral health is the indicator of good general health of an individual. Poor oral hygiene is the most important factor to cause dental diseases. Advanced stage of gum disease is called periodontitis. Periodontal disease affects the gum and jaw bone. Gingival health is compromised during pregnancy due to hormonal changes. This is called pregnancy gingivitis which is initial stage of periodontitis. Method: A matched case control study was conducted to identify the risk factors of periodontitis during pregnancy. Study duration was three months and it was conducted in tertiary care hospitals of Faisalabad (Madina teaching hospital, D.H.Q, Allied hospital). Cases were matched on the bases of month of pregnancy and number of pregnancy with control. Study sample was 282 (141 cases and 141 controls). Data were collected through questionnaire which comprises of two sections one is demographic data and one is questions related risk factors. Findings: Data were entered on SPSS software value was less than 0.05 and confidence interval was 95%. Multi logistic regression test was apply to identify the potential risk factors of periodontitis. Results have shown the different risk factors which can cause periodontitis. The most significant risk factors e.g. family history, systemic illness in which diabetes and hypertension were most common, poor eating habits due to lack of knowledge about oral health were common. Results will share with the health authorities of concerned hospitals.
Keywords
Periodontitis; Periodontal disease; Gingival
Introduction
Good oral health is the indicator of good general health of an individual. Poor oral hygiene is the most important factor to cause dental diseases. Dental plaque is a sticky colorless film which continually accumulates on teeth. Plaque may leads to many infections such as gingivitis. Gingivitis is the initial stage of gum disease which can be easily controlled or treatable if left untreated it become worse [1].
The worsen condition of gingivitis is called periodontitis [2]. Periodontal disease affects the gum and jaw bone. If periodontitis is not treated in the early stages it become worse due to increased production of clavicular fluid, which contains inflammatory mediators and bacterial flora that can damages the periodontium [3].
Periodontitis most commonly associated with a gram-negative anaerobic infection of these periodontium structures. The common normal flora of teeth is streptococci, which proliferate and in turn become colonized by other bacteria in saliva, such as Actinomyces species [4].
The mechanisms of this infectious process involve both direct tissue damage and indirect damage with the help of bacterial induction and host inflammatory immune responses [4].
Periodontal diseases are classified in two groups i.e., gingivitis and periodontitis. Gingivitis is inflammation of gingiva which periodontitis involve the soft tissues leading to the loss of bone [5].
As the disease progress the multiplication of microorganism primarily the gram negative bacteria causes disintegration of periodontal ligaments. It has been observed that the patients of periodontitis are on high risk of developing some systemic diseases like atherosclerosis, ischemic stroke and cardiovascular diseases [6].
Recent research shows that periodontitis can be associated for the development of cardiac disease. One theory suggests that bacteria of periodontal disease and inflammatory proteins enter in to blood stream and cause pathological effects on cardiovascular system. Recent study shows that bacteria present in periodontitis can lead to thickening of blood vessels as seen in heart diseases [7].
Gingival health is compromised during pregnancy due to hormonal changes. This is called pregnancy gingivitis which is initial stage of periodontitis. During pregnancy women need extra care to maintain good oral hygiene because hormonal fluctuations can triggers the nausea, vomiting. These hormonal fluctuations make existing gum disease worse [8].
Pregnancy Gingivitis increased in the first trimester of pregnancy and more worse in third trimester. Research shows that 15% childbearing women have high proportion of devolving periodontal disease [9].
Pregnancy is a physiological state that brings various changes in oral cavity along with many of other physiological changes taking place in the female body. The role of increased levels circulating estrogen is associated with prevalence of gingivitis [10].
Different studies show poor maternal oral health and unfortunately self-maintenance of oral hygiene in pregnant women faces different other barriers to achieving maximum oral health. These barriers to finding dental services include lack of knowledge, negative oral health experiences, and negative attitudes of dental staff toward pregnant woman [11].
Swollen gum, Tenderness, and redness, are some symptoms of periodontitis. Some common symptoms of periodontitis are bleeding from gums that bleed during bad breath and mobile tooth. During pregnancy these signs may become worse so professional dentist should be consulted [12].
Different research studies suggested that women with periodontitis have increased risk to deliver premature. According to the Center for Disease Control and Prevention (CDC), babies with less than 5.5 pounds birth weight have a risk of different health problems like motor skills, social development and learning disorders. Other problems are vision and hearing loss, feeding and digestive problems and respiratory problems [13].
Epidemiology of periodontitis
Periodontitis is one of the most common dental diseases in the world, related to poor general and oral health. It is reported that prevalence of periodontitis is high in both developed and developing countries. Severe periodontitis is sixth most prevalent disease affecting 743 million people worldwide [14].
It was reported that 80% of all adults in United States are suffering from periodontitis with clinical attachment loss (CAL) >2 mm. Prevalence of CAL >6 mm is reported less than 20% [15].
Various estimations shows from that 7% of the U.K population between age 35 and 64 had moderate to severe periodontitis. Incidence of moderate to severe periodontal disease in dental practices is much higher than previously survey [16].
The last 10 years research suggests relationship between periodontitis and risk of systemic disorders e.g. atherosclerosis, myocardial infarction, diabetes mellitus, and adverse pregnancy outcomes [6].
There is scanty research of National oral health in Pakistan. Moderate to advanced periodontitis has been reported 31%-40% in pregnant ladies have advanced periodontitis [17].
Pregnancy and periodontitis
Pregnancy is a delicate condition leading to different physiological changes in body structure, because of an increased production of different hormones such as oestrogens, progesterone, gonadotropins, and relaxine. The prevalence of various dental diseases increase during pregnancy such as caries and erosions [12].
The status of periodontal disease in Pakistan is very high in all age groups predominantly in childbearing women (18-34 years). Research suggests the range from 22% suffering from bleeding gums and 34% having calculus deposition [18].
In normal pregnancy tiny blood vessels of gum tissues dilated in the results of increased production pregnancy hormones such as progesterone and estrogen. This condition is more vulnerable to formation of plaque and toxins. Pregnancy periodontitis can be observed as early in 2nd month of pregnancy and may become worse in 8th month of pregnancy [19].
Economics of periodontitis
Clinically diagnosed periodontitis is costly to treat. Dental treatment is fourth highest costly treatment of all diseases [12].
Risk factors
Studies have been shown that 15% population of childbearing age affect with periodontitis [20].
Studies shown the strong association, OR=7.9, between periodontitis and adverse pregnancy outcome, either premature delivery or low birth weight in pregnant women of North Carolina [21].
Several researches support an association between periodontitis and premature birth. Periodontal pockets are reservoir of bacteria (usually Gram-negative bacteria, such as Porphyromonas gingivalis, Prevotella intermedia) and their virulent products, which reached the fetal placental unit through the hematogenic pathway and can lead to premature labor [13].
Tobacco smoking: Smoking is clearly defined risk factor to cause periodontitis [22]. National health survey shows an association between periodontitis and smoking. It has been observed that 90% of persons with periodontitis were smokers [23]. Smokers are on high risk to develop periodontitis than nonsmokers [24].
Diabetes mellitus: Most important oral sign of Diabetes is periodontitis and gingivitis. Patients with poorly controlled diabetes are on high risk to develop periodontitis [25].
The pathological and physiologically association between diabetes and periodontitis develop through the ability to produce an inflammatory responses either through bacterial adherence or by leading the production of inflammatory mediators [26].
Cardiovascular disease: 29% deaths occur worldwide due to cardiovascular diseases. Estimation of 2004 shown that 70 million Americans suffering from one of the types of CVD which includes hypertension, coronary artery disease and myocardial infarction are important cause of heart diseases [27].
Atherosclerosis is responsible for 50% of mortality in the United States, Europe and Japan Beside these causes one of the other risk factor is severe periodontitis that is associated with 25% to 80% increases the risk for heart diseases [28].
Estimation had shown that 91% of patients with cardiovascular diseases are suffering from mild to advance periodontitis and 66% of cardiologically healthy persons have periodontitis. The same estimated study showed a statistically correlation between myocardial infarction and periodontitis [29].
Periodontal pathogens can cause the atherogenicity in two way, firstly they invade the arterial wall directly and secondly they release some kind of inflammatory mediators after the response of infection [28].
These micro-organisms especially P. gingivalis, have confirmed the ability to interact the endothelial surface and to provoke smooth-cell proliferation, it also causes damage to the endothelial cells functioning. C-reactive protein also plays an important role in endothelial dysfunction, and increased levels of C-Reactive Proteins provide insight linking of periodontal disease and CVD [30].
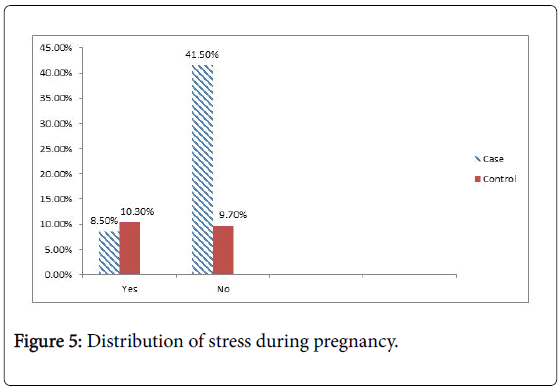
Stress: Patients with inadequate behavior and stress are at greater risk to develop periodontitis. Stress increased glucocorticoid secretions which can depress immune function and increased the risk of periodontitis. Patients who angry on daily basis have 43% higher risk developing periodontitis [31].
Female hormonal changes: Hormonal changes during puberty, menopause and pregnancy can alter the status of periodontal health. Most pronounced changes occur during pregnancy. Pregnant women are on high risk to develop periodontitis as compared to non-pregnant women [21].
Age: Several studies show that risk of developing periodontitis increase with the age. Periodontal destruction and bone loss seen under the age of 40 [19].
Treatment for periodontitis
Periodontitis can be intervening by surgically and non-surgically and may include systemic antibiotics. Tetracycline is a drug of choice to treat periodontitis because they suppress glaciations the proteins and minimize the activity of inflammatory mediators such as prostaglandins [32].
Periodontal treatment involves the debridement of surfaces, mineralized calculus and removal of dental plaque. Scaling and root planning are debridement methods which are done by surgically. Oral hygiene teaching, antiseptic and mouth wash such as chlorhexidine, dentifrices, tooth extraction, sub gingival curettage, and gingivectomy are the other interventions to treat the periodontitis [33].
Materials and Methods
A matched case control study was conducted from January-March 2016 to identify risk factors of periodontitis among pregnant women in district Faisalabad. The cases and controls were matched on month and number of pregnancy.
The sample size of case control study was calculated by WinPeppi software keeping confidence interval 95%. Total sample size was 282 pregnant ladies (cases 141 control 141).
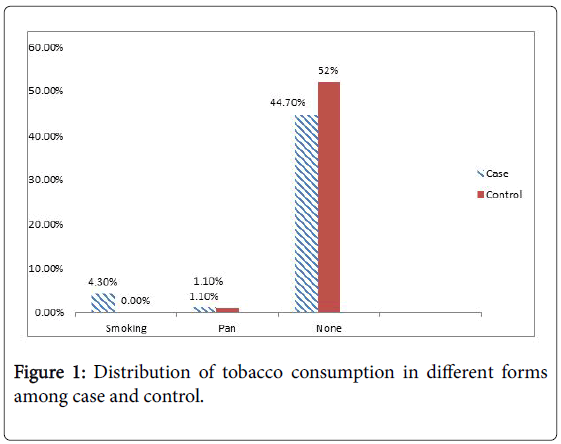
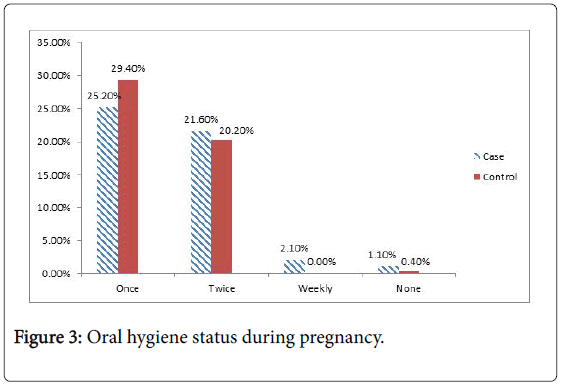
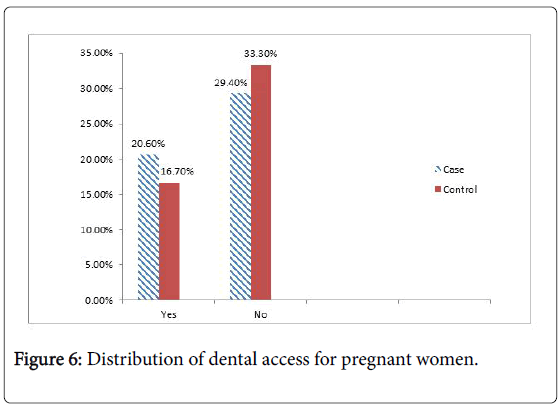
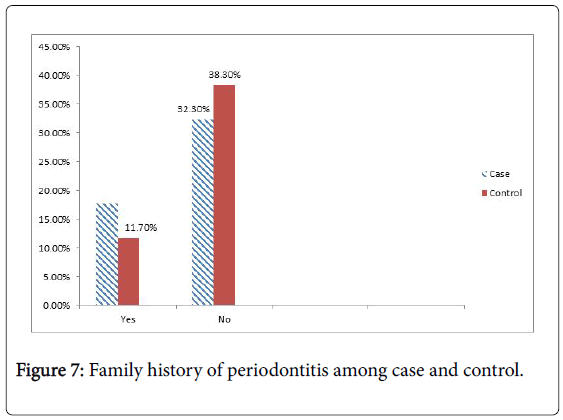
Data about risk factors of periodontitis in pregnant women was collected on a predesigned questionnaire in a face to face interview with cases (n=141) and controls (n=141). Questionnaire comprised of demographic information, clinical signs and risk factors. Written informed consent was signed by each participant (case and control) and briefly informed about purpose of study (Figures 1-7, Tables 1-3).
| Tobacco consumption | Parameters | Case(n=141) | Control(n=141) | Total(n=282) | P-value |
|---|---|---|---|---|---|
| Smoking | Numbers | 12 | 0 | 12 | 0.000* |
| % within the group | 100% | 0.00% | 100% | ||
| % of total | 4.30% | 0.00% | 4.30% | ||
| Pan | Numbers | 3 | 3 | 6 | |
| % within the group | 50% | 50% | 100% | ||
| % of total | 1.10% | 1.10% | 2.10% | ||
| No formof tobacco | Numbers | 126 | 138 | 264 | |
| % within the group | 47.70% | 52.30% | 100% | ||
| % of total | 45% | 48.90% | 93.60% | ||
| Total | Numbers | 141 | 141 | 282 | |
| % | 50% | 50% | 100% |
Table 1: Tobacco consumption among cases and controls.
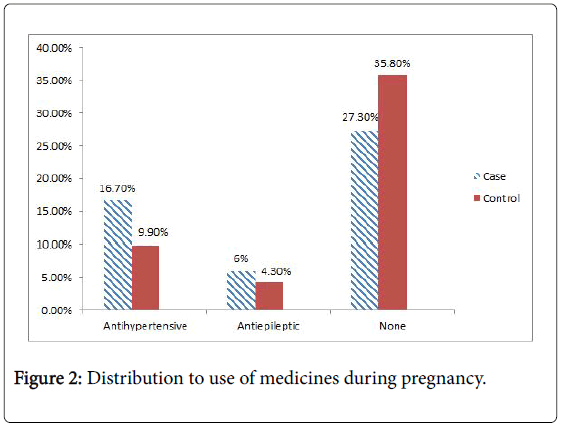
| Medication Status | Parameters | Case (n=141) | Control (n=141) | Total(n=282) | P-value |
|---|---|---|---|---|---|
| Antihypertensive | Numbers | 47 | 28 | 75 | 0.011â?° |
| % within the group | 62.70% | 37.30% | 100% | ||
| % of total | 16.70% | 9.90% | 26.60% | ||
| Antiepileptic | Numbers | 17 | 12 | 29 | |
| % within the group | 58.60% | 41.40% | 100% | ||
| % of total | 6% | 4.30% | 10.30% | ||
| No Medicine use | Numbers | 77 | 101 | 178 | |
| % within the group | 43.30% | 56.70% | 100% | ||
| % of total | 27.30% | 35.80% | 63.10% | ||
| Total | Numbers | 14100% | 141 | 282 | |
| % | 50% | 50% | 100% |
Table 2: Use of medicines during pregnancy.
| Variable | Cases (141) | Controls (141) | OR | 95% CI | P value |
|---|---|---|---|---|---|
| Systemic illness | 48 | 35 | 1.563 | 0.932-2.621 | 0.117 |
| Dental clinicnearby home | 58 | 47 | 1.398 | 0.861-2.270 | 0.218 |
| Husband allow to visit dentist | 50 | 54 | 0.885 | 0.546-1.436 | 0.711 |
| Food impaction | 45 | 28 | 1.892 | 1.097-3.261 | 0.029 |
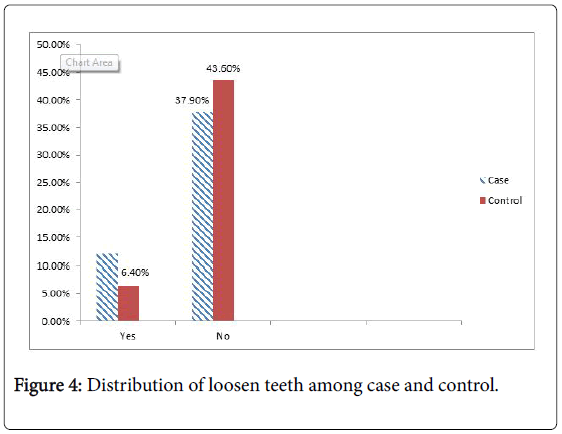
| Loosen teeth | 34 | 18 | 2.171 | 1.160-4.066 | 0.021 |
| Pregnancy history | 42 | 33 | 0.720 | 0.423-1.225 | 0.281 |
| Prefer female dentist | 39 | 50 | 0.696 | 0.420-1.153 | 0.2 |
| Balanced diet | 98 | 94 | 1.140 | 0.690-1.881 | 0.702 |
| Family history | 50 | 33 | 1.789 | 1.068-3.026 | 0.06 |
Table 3: Multi logistic regression results to identify the risk factors to cause periodontitis.
Discussion
The maternal oral health can be improved by identifying the risk factors and modifying lifestyle. Various risk factors have been identified that are involved in the progress of periodontitis. In present study the risk factors identified for periodontitis were low socioeconomic status, smoking, diabetes mellitus, and family history and previous history of periodontitis. Smoking is clearly defined risk factor to cause periodontitis, and these findings matched with the findings of Bergstrom and Preber [22],who had described that smokers are on high risk to develop advanced stage of periodontitis [22]. The association of periodontitis and adverse pregnancy outcome, either premature delivery or low birth weight in pregnant women of North Carolina was OR=7.9 [21]. The status of periodontal disease in Pakistan is very high in all age groups predominantly in childbearing women (18-34 years). 22% suffering from bleeding gums and 34% having calculus deposition [18].
Pregnant women of low socioeconomic status don’t have enough resources to manage balance diet and to seek medical advice. Thus such woman cannot afford to consult a professional dentist due to lack of resources and lack of knowledge and usually the do not have enough money to pay dental fee.
In present study data were collected from tertiary care hospitals of Faisalabad. These hospital are highly over burded to patients and mostly patients come from lower and middle class. They do not have good knowledge and awareness about the diseases and consequently they do not enough weightage about medical treatment. Even if they consult to a doctor they will not be serious in follow up of treatment.
In present study, the association (OR=1.563) found between development of periodontitis and systemic illness like diabetes mellitus and hypertension. Systemic illness is important risk factor to cause periodontitis. 91% of patients with cardiovascular diseases are suffering from mild to advance periodontitis and 66% of cardio logically healthy persons have periodontitis. The same estimated study showed a statistically correlation between myocardial infarction and periodontitis [29]. Most important oral sign of Diabetes is periodontitis and gingivitis. Patients with poorly controlled diabetes are on high risk to develop periodontitis [25].
In present study the significant association found p value=0.000 and C.I 95%. Family history is another risk factor of periodontitis. Association between Family history and periodontitis (OR=1.789).
Diet is compromised during pregnancy and women needs balanced diet. Mostly women develop bad eating habits during pregnancy. Association between balance diet and periodontitis (OR=1.140). Health education about personal and oral hygiene is very important for pregnant ladies to maintain their healthy pregnancy. Government should be increased the standard of government hospitals, their level of care, so that maximum patients avail their health care facilities.
Results were discussed with health authorities of certain hospitals and discussed risk factors. It was also discussed that dental care is very expensive and people cannot afford it. They ensure that dental care facility will be maximum provide to the pregnant ladies in case of any oral or dental disease.
The limitation of these study shows that sample size was less and it cannot be generalized the whole population.
Recommendations
• Education campaigns for mothers should be in every antenatal clinic about oral health.
• healthy glucose monitoring in case of diabetes mellitus.
• Early recognition of these risk factors will improve the health of pregnant women.
Every pregnant woman should screen earlier if she had;
• Family history of Periodontitis.
• Previous pregnancy history of Periodontitis.
References
- Dzink JL, Socransky SS, Haffajee AD (1988) The predominant cultivable microbiota of active and inactive lesions of destructive periodontal diseases. J ClinPeriodontol 15: 316-323.
- Lohsoonthorn V1, Kungsadalpipob K, Chanchareonsook P, Limpongsanurak S, Vanichjakvong O, et al. (2009) Is maternal periodontal disease a risk factor for preterm delivery? Am J Epidemiol 169: 731-739.
- Foreman S, Kilsdonk J, Boggs K, Mouradian WE, Boulter S, et al. (2012) Broader Considerations of Medical and Dental Data Integration. In. Integration of Medical and Dental Care and Patient Data(3rd edn.) Springer pp: 167-298.
- Genco RJ (1992) Host responses in periodontal diseases: current concepts. J Periodontol 63: 338-355.
- Mannucci PM (1998) Hemostatic drugs. N Engl J Med 339: 245-253.
- Genco RJ (2009) Periodontal disease and association with diabetes mellitus and diabetes: clinical implications. J Dent Hyg 83: 186-187.
- FA Carranza (1990) Glickman’s clinical periodontology. Philadelphia: WB Saunders Co. (7th edn.) pp: 335-351.
- Boggess KA, Edelstein BL (2006) Oral health in women during preconception and pregnancy: implications for birth outcomes and infant oral health. Matern Child Health J 10: 169-174.
- Pepys MB, Hirschfield GM, Tennent GA, Gallimore JR, Kahan MC, et al. (2006) Targeting C-reactive protein for the treatment of cardiovascular disease. Nature 440: 1217-1221.
- Xiong X, Buekens P, Fraser W, Beck J, Offenbacher S(2006) Periodontal disease and adverse pregnancy outcomes: a systematic review. BJOG113: 135-143.
- Gaffield ML, Gilbert BJ, Malvitz DM, Romaguera R (2001) Oral health during pregnancy: an analysis of information collected by the pregnancy risk assessment monitoring system. J Am Dent Assoc 132: 1009-1016.
- Silness J, Loe H (1964) Periodontal Disease in Pregnancy. Ii. Correlation Between Oral Hygiene and Periodontal Condtion. ActaOdontolScand 22: 121-135.
- Mishra P, Gita B, Chandrasekaran SC(2014) Assessment of Periodontal Status in Association with Gestational Diabetes Mellitus: A Case-Control Study. J Diabetes Metab 5.
- Kumar TS, Dagli RJ, Mathur A, Jain M, Balasubramanyam G, et al.(2009) Oral health status and practices of dentate Bhil adult tribes of southern Rajasthan, India. Int Dent J 59: 133-140.
- Smith ML, Mott A, Marques C, Maor Y, de Andrade M,et al. (2005) Position paper: epidemiology of periodontal diseases. J Periodontol 76: 1406-1419.
- Agarwal V, Khatri M, Singh G, Gupta G, Marya C, et al. (2010) Prevalence of periodontal diseases in India. Health Care 44.
- Wali ZH (2002) Effects of cigarette smoking on periodontal health status among the fifth year dental students In Iraq. Journal of the College of Dentistry 60.
- Mealey BL, Rose LF (2008) Diabetes mellitus and inflammatory periodontal diseases. CurrOpinEndocrinol Diabetes Obes 15: 135-141.
- Hugoson A, Laurell L, Lundgren D(1992) Frequency distribution of individuals aged 20–70 years according to severity of periodontal disease experience in 1973 and 1983. J ClinPeriodontol 19: 227-232.
- Moore S, Randhawa M, Ide M(2005) A case–control study to investigate an association between adverse pregnancy outcome and periodontal disease. J ClinPeriodontol 32: 1-5.
- Offenbacher S, Katz V, Fertik G, Collins J, Boyd D, et al. (1996) Periodontal infection as a possible risk factor for preterm low birth weight. J Periodontol 67: 1103-1113.
- Bergström J, Preber H (1994) Tobacco use as a risk factor. J Periodontol 65: 545-550.
- Johnson GK, Slach NA (2001) Impact of tobacco use on periodontal status. J Dent Educ 65: 313-321.
- Müller HP, Stadermann S, Heinecke A(2002) Longitudinal association between plaque and gingival bleeding in smokers and non-smokers. J ClinPeriodontol 29: 287-294.
- AlJehani YA (2014) Risk factors of periodontal disease: review of the literature. Int J Dent 2014: 182513.
- Miller LS, Manwell MA, Newbold D, Reding ME, Rasheed A, et al.(1992) The relationship between reduction in periodontal inflammation and diabetes control: a report of 9 cases. J Periodontol 63: 843-848.
- Pihlstrom BL, Michalowicz BS, Johnson NW (2005) Periodontal diseases. Lancet 366: 1809-1820.
- Geerts SO, Legrand V, Charpentier J, Albert A, Rompen EH (2004) Further evidence of the association between periodontal conditions and coronary artery disease. J Periodontol 75: 1274-1280.
- Albandar JM, Rams TE (2002) Global epidemiology of periodontal diseases: an overview. Periodontol 2000 29: 7-10.
- Amar S, Gokce N, Morgan S, Loukideli M, Van Dyke TE, et al. (2003) Periodontal disease is associated with brachial artery endothelial dysfunction and systemic inflammation. ArteriosclerThrombVascBiol23: 1245-1249.
- Merchant AT, Pitiphat W, Ahmed B, Kawachi I, Joshipura K (2003) A prospective study of social support, anger expression and risk of periodontitis in men. J Am Dent Assoc 134: 1591-1596.
- Simpson TC, Needleman I, Wild SH, Moles DR, Mills EJ(2010) Treatment of periodontal disease for glycaemic control in people with diabetes. Cochrane Database Syst Rev CD004714.
- Madden TE, Herriges B, Boyd LD, Laughlin G, Chiodo G, et al. (2008) Alterations in HbA1c following minimal or enhanced non-surgical, non-antibiotic treatment of gingivitis or mild periodontitis in type 2 diabetic patients: a pilot trial. J Contemp Dent Pract 9: 9-16.
Relevant Topics
- Child Health Education
- Construction Safety
- Dental Health Education
- Holistic Health Education
- Industrial Hygiene
- Nursing Health Education
- Occupational and Environmental Medicine
- Occupational Dermatitis
- Occupational Disorders
- Occupational Exposures
- Occupational Medicine
- Occupational Physical Therapy
- Occupational Rehabilitation
- Occupational Standards
- Occupational Therapist Practice
- Occupational Therapy
- Occupational Therapy Devices & Market Analysis
- Occupational Toxicology
- Oral Health Education
- Paediatric Occupational Therapy
- Perinatal Mental Health
- Pleural Mesothelioma
- Recreation Therapy
- Sensory Integration Therapy
- Workplace Safety & Stress
- Workplace Safety Culture
Recommended Journals
Article Tools
Article Usage
- Total views: 11353
- [From(publication date):
October-2016 - Dec 04, 2024] - Breakdown by view type
- HTML page views : 10589
- PDF downloads : 764