Case Report Open Access
A Blue Spotted Baby: A Case Report
Célia Silva1, Carlos Mendes2, Luísa Sousa3and Humberto S Machado4*
1USF Families, Santa Maria da Feira, Portugal
2USF John Week, Ovar, Portugal
3Gynecology and Obstetrics, Hospital Entre Douro e Vouga, Portugal
4Anaesthesiology Department, Hospital of Porto, Portugal
- *Corresponding Author:
- Humberto S Machado
Anaesthesiology Department Hospital of Porto
Largo professor Abel Salazar, Portugal
Tel: +351935848475
E-mail: hjs.machado@gmail.com
Received date: August 24, 2016; Accepted date: August 26, 2016; Published date: August 31, 2016
Citation: Silva C, Mendes C, Sousa L, Machado HS (2016) A Blue Spotted Baby: A Case Report. J Preg Child Health 3:273. doi:10.4172/2376-127X.1000273
Copyright: ©2016 Silva C, et al. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.
Visit for more related articles at Journal of Pregnancy and Child Health
Abstract
Background: The Mongolian spot (MS) is a congenital macula of blue-gray colour usually located on the sacrococcygeal region, but may have atypical locations such as the back and more rarely the limbs. Case report: The authors describe a case of an infant male, born from a monitored pregnancy without complications, whose skin objective examination showed a Mongolian spot occupying the entire lower back region and lower limbs with many similar spots of different sizes and locations as well as on the back of the right hand. Further physical examination appeared to be normal. Discussion: The knowledge of normal variants is crucial in clinical practice of the family doctor, particularly in child health consultation. This atypical skin colouration arises with relative frequency in our population and although it does not seem strange in the usual location, the appearance in atypical locations can be a sign of other associated pathologies, and if they had not been observed at birth, they can be an alert for eventual child abuse. Conclusion: The early diagnosis of the MS and the follow-up and monitoring of the child’s development is crucial to assess the evolution of pigmentation, which usually involutes in early childhood but can persist into adulthood, especially if there were multiple spots and locations.
Keywords
Mongolian spot; Birthmark; Transient skin lesions
Introduction
The Mongolian spot (MS), also known as congenital dermal melanocytosis, is a congenital macula of blue-gray colour, with variable shape and size, resulting in an abnormal migration of melanocytes, which are added in the dermis. It is usually located in the sacrococcygeal or lumbar region, but it may have atypical locations such as back and more rarely limbs. It is present in 10% of Caucasian new-borns but may reach about 80% of Black and Asian babies and it seems that both sexes are affected, with a slightly higher prevalence in boys [1].
The exact origin of the MS is unknown, although the most consistent theory admits that the MS represents a rudimentary formation of the simian tail [2].
The colouring of MS, attributed to the reflection of dermal pigmentation in the skin surface, is more intense at one year of age and it gradually disappears.
Visually, this spots are macular, without a texture and round, oval or irregularly shaped. The colour varies from blue to greenish, gray, black or the combination of any of the above colours [3].
The number of spots varies and there may be only one or several in the same person. Similarly, the size varies from small spots with less than 1cm in diameter to more than 20 cm [4].
The MS usually disappears during early childhood, due to inclusion of dermal melanocytes by a protective extracellular fibrous sheath.
Most commonly these spots regress by early childhood (before 6 years of age), however the extensive type regresses very slowly and the persistent type may be seen into adulthood. The persistent type is related to abundance of melanocyte stimulating growth factors, defective regulation of melanocyte proliferation in epidermal and genetic factors.
As MS are histologically characterized by spindle-shaped melanocytes within the dermis, they are thought to be the result of the failure of melanocytes to correctly migrate from the neural crest to the developing epidermis.
Differential diagnosis mainly includes physical abuse, a condition excluded in our patient.
Extensive differential diagnosis should be done with other potentially serious dermal melanocytosis like nevus of Ota, nevus of Ito, Hori nevus (Grupta) and blue nevus [5]. These pathologies may be confused with aberrant MS. There are also serious congenital disorders such as Gangliosidosis that can course with blue-greyish spots or macules.
Main characteristics to diagnose MS are: onset at birth, disappearance with age and absence of mucosal involvement/ progression to malignancy.
Case Report
We observed an infant male, born from a monitored pregnancy, in which no complications or abnormalities were noticed. The mother, aged 28, G1P0 and the father, aged 28, are both healthy and with no history of consanguinity. During pregnancy, mother was supplemented with folic acid in the first part of pregnancy and iron in the third trimester by mild anaemia. There was no history of drug ingestion or contact with potentially harmful substances during or before pregnancy. The delivery was by caesarean section for orthopaedic indication of the mother, at 37 weeks of gestation, after spontaneous rupture of membranes. The Apgar score was 9 and 10, respectively to the first and fifth minute. Birth weight was 2850 g and 46 cm tall, and the neonatal period was totally uneventfully.
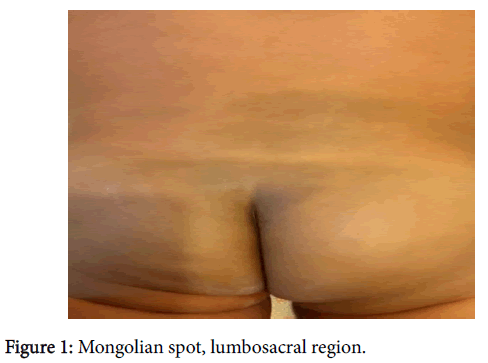
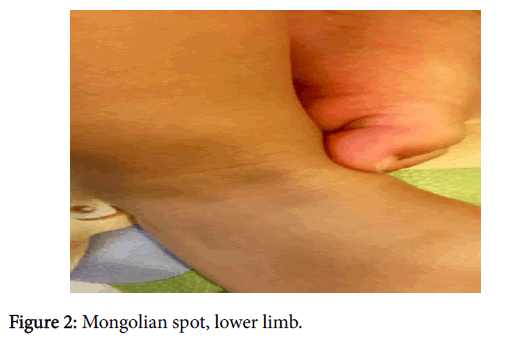
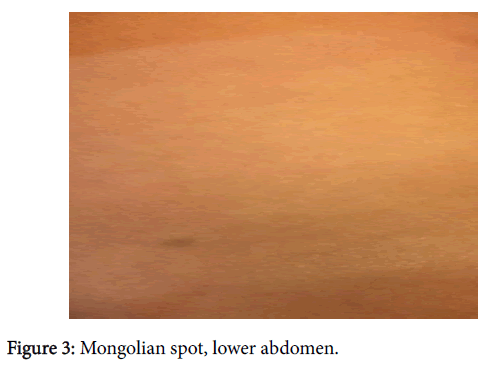
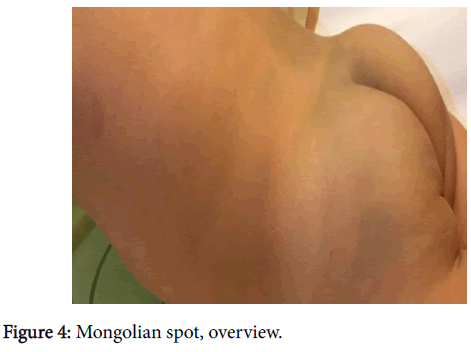
The objective examination of the skin showed a blue-gray spot occupying the entire lower back region (about 6 cm) and in the lower limbs many similar spots of different sizes (between 1-3 cm) and locations as well as on the back of the right hand (about 1 cm) (Figures 1-4).
The colouring of the spots was similar, presenting macular spot without any aberrant skin texture or hairiness. Further physical examination was normal, particularly in ophthalmological, neurological and further dermatological examination.
In subsequent routine visits, there was a good stature evolution, as well as weight and psychomotor development of the baby, with the consonant growth of the spots.
At the age of 18 months, it was observed that the spots of the right hand and ankle could hardly be seen. Nevertheless, the biggest spot at the lumbosacral region remained big and with a blue-gray colour.
Discussion
The observation of a new-born includes the assessment of the anthropometric measures, complete physical examination and it becomes particularly relevant for the demand for normal variants.
The cutaneous variants are most common, and they appear in almost all of the new-borns, in which we include the MS. MS are benign, congenital, bluish macules affecting healthy new-borns and generally disappear during childhood.
A typical localization and shape and presence of many MS require a differential diagnosis from dermatologic diseases as well as from child abuse and bleeding diathesis.
In this case, the absence of other abnormalities in the physical and neurological examination, the proper development of the baby and the consistency of size and staining of the spots firmly points to the presence of MS.
Thus, MS may worry families because of the difficulty in differential diagnosis in cases where clinical presentation is atypical. Therefore, the knowledge of normal variants is crucial in clinical practice of the Family doctor, particularly in child health consultation. In addition, the follow-up and monitoring of the evolution of the child is fundamental to assess the evolution of pigmentation, which usually involutes in early childhood but can persist into adulthood, especially if multiple or with a large extension.
Conclusion
It is essential to be aware of the various shapes and localizations of MS as well as the frequency in population to facilitate the diagnosis, inform parents, and eliminate parental distress, to strengthen the family-doctor relationship.
It is fundamental the observation of the similarity between the MS and the spots found in other potentially serious conditions. In this case, elevated level of suspicion proved to be essential by the number, size, location and atypical staining intensity.
On the other hand, the physical examination of the new-born is of paramount importance in order to avoid additional studies in otherwise healthy children.
References
- Egemen A (2006) Frequency and characteristics of Mongolian spots among Turkish children in Aegean region. The Turkish Journal of Pediatrics 48: 232-236.
- Musumeci ML, Lacarrubba F, Santagati C (2016) Multiple and superimposed Mongolian spots. BMJ Case Rep.
- I-Hsin Shih (2007) Neonatal birthmark survey. Birthmark Survey in 500 new-borns: Clinical observation in two northern Taiwan medical center nurseries. Chang Gung Med J 30: 220-225.
- Hackbart B (2013) Mongolian spots are not always a benign sign. J Pediatr 162:1070.
- Monteagudo B (2011) Prevalencia de marcas de nacimiento y lesionescutâneastransitorias en 1.000 reciénnacidosespañoles. ActasDermosifiliogr 102: 264-269.
Relevant Topics
Recommended Journals
Article Tools
Article Usage
- Total views: 12626
- [From(publication date):
August-2016 - Apr 03, 2025] - Breakdown by view type
- HTML page views : 11734
- PDF downloads : 892