A Biological Approach to Building Resilience and Wellness Capacity among Public Safety Personnel Exposed to Post-traumatic Stress Injurie
DOI: 10.4172/1522-4821.1000482
Abstract
To review core biological processes that underlie psychophysiological dysfunction following trauma that have not been adequately addressed in prior resilience intervention research and propose a novel way to improve intervention outcomes. Methods: The authors present a theoretical and methodological approach to building resilience among PSP tested and refined across six, grant-funded, multi-method studies with over 300 police participants measuring objective psychophysiological and behavioral data. Results: Modifying cardiorespiratory function through autonomic modulation training utilizing heart rate variability biofeedback techniques has been identified as one evidence-based method of improving wellness and performance outcomes among PSP. Conclusions: Policy implications include directing research efforts and funding support for biologically based resilience interventions among PSP.
Keywords: Biological Resilience, Post Traumatic StressInjury; Autonomic Modulation; Heart Rate Variability; Respiratory Sinus Arrhythmia; Police; Public Safety Personnel; Mental Health; Intervention; Heart Rate Variability Biofeedback
Introduction
Police officers are routinely exposed to hazardous, disturbing events that can impose severe stress and long-term trauma. Upwards of 15-26% of public safety personnel (PSP) report one or more mental health symptoms. (Carleton et al., 2018) Accumulated stress and posttraumatic stress injuries (PTSI) result in chronic physical and mental health disorders including anxiety, depression, substance abuse, and cardiovascular disease. (Arpaia & Andersen, 2019; Violanti et al., 2006) PTSI are also related to reduced occupational performance, absenteeism, and risky behaviour, with implications for both police and public safety. (Austin-Ketch et al., 2012; Ruotsalainen et al., 2014) Recent empirical evidence and government reports have highlighted a mental health and suicide crisis among from various PSP sectors in North America. (Carleton et al., 2018; Suicide, 2019) The research above forms an urgent call for evidence-based programs that build resilience and wellness capacity in order to prevent PTSI symptoms before they manifest as severe, chronic, diagnosable disorders. However, existing prevention and resilience interventions for PTSI tailored to PSP show limited effectiveness. (Ruotsalainen et al., 2014; Carleton et al., 2018; Smith et al., 2018).
Advances in physiology and neuroscience demonstrate that resilience is maintained by the healthy functioning of psychophysiological systems within the body. Objective biological measures have shown that chronic stress and trauma disrupt both psychological and physiological functioning, eroding resilience and reducing wellness capacity. Traditional interventions to build resilience among PSP have not adequately addressed the physiological underpinnings that lead to mental and physical health conditions, as well as burnout and fatigue following trauma. (Lehrer, 2018; Rogala et al., 2014; Maslach et al., 2001; Morse et al., 2012; Violanti & Gehrke, 2004) In this paper we posit that, to date, there has been a missing piece in intervention research for PSP exposed to trauma. Specifically, the consideration of psychophysiology. We propose a biological approach to building resilience and wellness capacity among PSP exposed to PTSI. Prior research shows that autonomic modulation techniques, such as heart rate variability biofeedback, effectively reduce psychophysiological stress and mental health symptoms in clinical and non-clinical populations. (Lehrer et al., 2020; Lin et al., 2018; Goessl et al., 2017; Tan et al., 2011) We also present examples from intervention research in the field of policing that demonstrate that autonomic modulation techniques improve police health and occupational performance when completed during scenario-based, in-person training (Andersen et al., 2018; Andersen & Gustafsberg, 2016; Andersen et al., 2016).
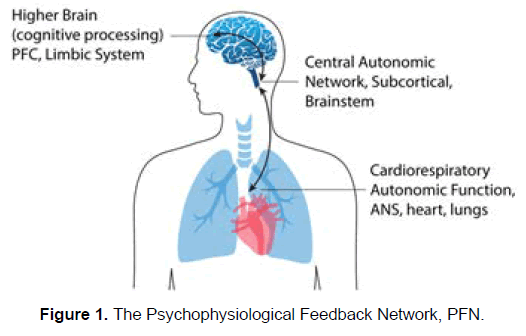
Biological Resilience: The Missing PieceTraditional interventions to build resilience or relieve symptoms of PTSI are focused on addressing cognitive, emotional, and behavioural components without addressing underlying neurological and physiological mechanisms that erode resilience, maintain pathology, and cause symptoms to resurface following treatment. (LeDoux & Pine, 2016; Minassian et al., 2015) For example, research and clinical practice have shown that directing patients to apply effortful, consciously deployed strategies like reappraisal are not helpful when either subcortical circuitry (e.g., brainstem) or peripheral (e.g., nervous system) physiology is dysregulated. (Arpaia & Andersen, 2019; Lehrer, 2018; LeDoux & Pine, 2016) Theoretical models and recent research indicate that biological resilience is maintained by the psychophysiological feedback network (PFN, Figure 1), comprised of bidirectional signals between a) higher order cognitive and emotional processing regions of the brain (e.g., prefrontal cortex (PFC) and limbic system), b) subcortical regions of the central autonomic network (e.g., brainstem), and c) the peripheral autonomic nervous system (ANS) (e.g., parasympathetic and sympathetic), including the heart and lungs (Lehrer, 2018; Porges, 2003; Smith et al., 2017; Thayer et al., 2009).
In other words, healthy functioning of the bi-directional signals between the brain and the central and peripheral nervous systems maintains resilience, defined as adaptive emotion regulation, cognition, and the physical capacity to function in the face of stress. (Porges, 2003; Smith et al., 2017; Mather & Thayer, 2018) Typically, when a person encounters stress (either real or imagined) they will experience characteristic changes in the nervous system, including increased sympathetic nervous system (SNS) activation that elevates heart rate (HR) and respiration, and a withdrawal of parasympathetic nervous system (PNS) activation. When stress has abated, PNS activation will lower heart and breathing rates and blood pressure, helping the body returns to reparative and restorative functioning (Porges, 2003).
Exposure to chronic stress and PTSI is strongly associated with disruption in the function of individual PFN system components and the signals between systems, which can lead to a reduction in an individual’s short- and long-term reserves to maintain wellness. (Arpaia & Andersen 2019; LeDoux & Pine, 2016; Gillie & Thayer, 2014; Glover et al., 2006; McEwen, 2002) afferent connections from the heart and lungs to the brain indicate that dysregulation in breathing and cardiac dynamics directly influence brain physiology and cognitive processing in ways that exacerbate acute and chronic stress. (Holzman & Bridgett, 2017) For example, upon exposure to a traumatic event an individual may feel threatened (i.e., PFC, limbic system activation) and experience dramatic changes in ANS activation causing a rapid rise in HR (i.e., enhanced SNS and PNS withdrawal) and respiration (i.e., hyperventilation). At a later date, changes in respiration unrelated to threat (e.g., resulting from physical exertion) may trigger dysfunctional cognitive processes (e.g., appraisal of a non-threatening situation as dangerous) resulting in maladaptive behavior (e.g., avoiding situations they should be attending to). Chronic stress and trauma are associated with a ‘rewiring’ of the PFN, such that a person may experience the withdrawal of PNS activity, or increases in SNS, even when they are at rest (Holzman & Bridgett, 2017). Given that the ANS plays an essential role in the PFN, linking visceral organs such as the heart and lungs with higher order brain regions like the PFC, when the balance between SNS and PNS activity is disrupted, the individual becomes vulnerable to mental and physical health conditions (Thayer et al., 2009; Ginty et al., 2017).
The good news is that the function of the PFN, thus the level of resilience, can be objectively measured and strengthened using cardiorespiratory biometric indices such as heart rate variability (HRV) and respiratory sinus arrhythmia (RSA). (Holzman & Bridgett, 2017; Lehrer & Gevirtz, 2014) Prior research indicates that each of these indices can be targeted by autonomic modulation training to improve resilience and wellness capacity.
Methods
Cardiorespiratory Indices of Wellness Capacity
HRV has been characterized as an index of autonomic resilience. (Hildebrandt et al., 2016) HRV is the variation in the time between successive heart beats and depends primarily on the extrinsic regulation of HR by the balance between SNS and PNS branches of the ANS. (Acharya et al., 2006; Laborde et al., 2017) If the time between heart beats is rather constant, HRV will be low, whereas if the time varies, HRV will be higher. When a person is at rest, high HRV signals good health because it represents a physical indicator of autonomic flexibility in responding to challenges. (Acharya et al., 2006; Shaffer & Ginsberg, 2017) In contrast, low resting HRV signals an imbalance in autonomic function, such as in clinical cases of anxiety and psychopathology where there is an overactivation of the sympathetic branch and a weakening of parasympathetic influence over the heart. (Beauchaine & Thayer, 2015) As mentioned, parasympathetic function is associated with restorative and regulatory processes in the body (e.g., immune functioning, growth, and repair), and a lack of PNS function is associated with both physical (e.g., cardiovascular disease) and mental health problems. (Beauchaine & Thayer, 2015; Ginsberg, 2016) There are a variety of HRV parameters that indicate autonomic resilience (e.g., time- and frequencydomain measures, RSA). (Laborde et al., 2017) and may be targeted to rewire maladaptive functioning in the PFN.
Respiratory Sinus Arrhythmia (RSA) refers to heart rate variability that is in phase with breathing such that HR speeds up during inhalation (shortening the time between heart beats) and slows during exhalation (lengthening the time between heart beats). (Lehrer & Gevirtz, 2014; Yasuma & Hayano, 2004) As noted in Figure 1, the lungs and respiratory system play a key role in the PFN. Increasing RSA builds physical wellness capacity by strengthening an individual’s long-term reserves, theorized to occur via multiple pathways (i.e., baroreflex control, blood pressure regulation, and efficiency of pulmonary gas exchange). (Lehrer, 2018; Lehrer & Gevirtz, 2014) RSA is also associated with stimulation of the vagus nerve, a principle nerve of the PNS. (Brodal, 2004) Thus, RSA can be measured to examine the functional state of the PNS. Porges (2003) Research reveals a connection between respiration, arousal, and emotional control, such that the manner by which a person breathes sends signals to regions in the brainstem and forebrain that modulate arousal. (Mather & Thayer, 2018) For example, periods of slow breathing are associated with SNS suppression and PNS stimulation, which may underlie the anxiety and stress-reducing effects of RSA. (Mather & Thayer, 2018).
The authors have expanded the use of RSA as a microintervention during acute stress to assist patients (Arpaia) and police officers (Andersen & Gustafsberg) to regain focus, shift attention, and select responses that better match the demands of the situation at hand. For example, when a person’s HR is high due to mental stress, they can change the pattern of a single breath, causing a rapid drop in HR due to vagal outflow. This drop in HR is then communicated via vagal afferents to the solitary nucleus in the brainstem, Browning & Travagli (2011) activating feedback loops in the PFN via secondary connections from the solitary nucleus to widespread brain areas involved in perceptual, cognitive, and emotional processing (Figure 1). Browning & Travagli (2011) The drop in HR lasts a few seconds and provides a brief temporal window during which these changes in brain processing enable the person to reassess the environment and direct attention to more helpful behavioral, cognitive, and / or emotional responses (Arpaia, personal communication, 2019) (Lehrer, 2018; Vlemincx et al., 2013). The authors have used autonomic modulation techniques teach individuals to modify both short- and long-term RSA, an objective indicator of the ability to recover more quickly following stress, and has been shown to effectively do so in clinical samples and police officers (Lehrer et al., 2020; Andersen et al., 2018).
Below we describe the particular methods and autonomic modulation techniques that we have used with clinical patients and PSP to test our biological approach to building resilience.
Autonomic Modulation Training: Strengthening Resilience and Wellness Capacity
In order to teach individuals how to modulate autonomic processes and signals between networks in the PFN, we have utilized heart rate variability biofeedback (HRVB), a methodology that enables an individual to manipulate cardiorespiratory function. Heart rate variability biofeedback is a technique that has been developed and refined by Lehrer and colleagues over the past three decades. (Lehrer & Gevirtz, 2014) During HRVB, a person is shown visual feedback of their beat-by-beat heart rate data while engaging in slow breathing with the goal of maximizing RSA. The optimal slow breathing pace differs from person to person, is not intuitive, and does not occur naturally in waking states. Therefore, training is required to gradually develop comfort with breathing at a pace that maximizes RSA, with the eventual goal of being performed unconsciously through rewiring of the PFN. (Lehrer et al., 2000) For clinically effective treatment, it is not sufficient to simply instruct a person to breathe slowly. Rather, HRVB training is required to identify the precise breathing rate for maximizing RSA to the individual, and to condition this rate through practice. (Lehrer et al., 2000) There is promising empirical support for the effectiveness of HRVB for modifying symptoms associated with PTSI, such as anxiety (Goessl et al., 2017), depression (Beckham et al., 2013; Caldwell, 2015; Karavidas et al., 2007), insomnia (Lin et al., 2019) and PTSD (Tan et al., 2011).When people practice HRVB daily over a period of time, RSA is improved even during periods outside of daily practice (Lehrer et al., 2003).
To provide context for the biological tools described above, the authors also use psychological tools that have been shown to effectively reduce clinical symptoms and build resilience and wellness capacity among individuals Arpaia & Andersen (2019). Specifically, these meta-cognitive skills, defined as the awareness and understanding of one’s own thought processes, assist individuals in learning to correctly identify psychophysiological demands and resources and regulate the appraisal of experience using attentional and cognitive techniques. Arpaia & Andersen (2019) Meta-cognitive skills combined with HRVB and short term RSA provides individuals with a more comprehensive way to rewire the PFN. We call this ‘autonomic modulation training.’ In line with prior work, our biologically focused approach of teaching individuals to modify autonomic processes as a way to change higher order cognitive functioning appears to help individuals feel more in control of physiological, behavioral and emotional functioning all around (Lehrer et al., 2000; Mizener et al., 1988; Nanke & Rief, 2000; Wilson, 2017). Below we outline the research that supports our proposed biological approach to building resilience and wellness capacity among police.
Results
The proposed approach to building resilience and wellness capacity among PSP is the culmination the authors extensive experience working with soldiers, veterans, police, and trauma survivors over the past 20 years. In a research context, Andersen has worked with civilian and military personnel exposed to mass trauma, acute stress disorder, and PTSD (Pizarro, 2006; Silver et al., 2006; Pizarro, 2004; Silver et al., 2005; Holman et al., 2008; Andersen et al., 2010; Possemato et al., 2010; Silver et al., 2013; Andersen et al., 2013; Andersen & Silver 2020). In a clinical context, Arpaia has developed and refined autonomic modulation techniques in his psychiatry clinical practice for the past 20 years with over 700 patients Arpaia & Andersen (2019). Gustafsberg, an academic and retired commander and trainer of elite federal Special Forces units in Europe, has been developing and refining autonomic modulation in the field with active duty officers. (Gustafsberg, 2014; Åhman & Gustafsberg, 2017; Gustafsberg, 2018) The authors combined experience and expertise have laid the foundation for the proposed theoretical and practical approach to building resilience and wellness capacity among PSP exposed to post traumatic stress injury.
In collaboration and with advisement from expert police practitioners, medical and academic experts in psychophysiological risk and resilience, the authors developed the International Performance Resilience and Efficiency Program (iPREP) an intensive resilience program to address the unique acute and chronic stressors that police officers face and to improve occupational health and performance. (Andersen et al., 2018; Andersen & Gustafsberg, 2016, Andersen et al., 2016) This program has been refined across six, grant-funded, multi-method studies with over 300 police participants measuring objective psychophysiological and behavioral data. (Andersen & Collins, 2020; Planche et al., 2019; Andersen et al., 2017; Andersen & Papazoglou, 2015; Andersen et al., 2016; Andersen et al., 2016; Andersen et al., 2016; Andersen et al., 2015; Andersen et al., 2015; Andersen et al., 2015; Andersen et al., 2015; Andersen et al., 2015; Andersen & Papazoglou, 2014; Papazoglou & Andersen, 2014) the most recent i PREP validation study repeatedly tracked police officers up to 18 months post-training, showing significant, long-term reductions in occupational errors, and improvements in their ability to recover quickly from acutely stressful events (Andersen et al., 2018).
Discussion
Taken together, the research and clinical evidence above demonstrates how psychophysiological dysfunction results from chronic and traumatic stress. Additionally, the evidence reviewed provides insight into the necessary biological components of relieving current distress and preventing future suffering following trauma exposure. We propose that autonomic modulation training (AMT) fills an existing gap in the applied research literature supporting capacity-building prevention and intervention programs for PSP exposed to PTSI, such that AMT measures and strengthens objective biological resilience. This paper serves as a ‘call to action’ inviting other researchers and practitioners to explore and test our proposed approach in basic and applied settings.
Funding
Funding of this project was provided by a grant from the Government of Ontario Ministry of Labour (ROP 15-R-021), which funded partial data collection. However, the Ministry had no other involvement in the conceptualization, design, analysis, decision to publish, or preparation of this manuscript.
Authors Conflict of Interest
The authors declare no competing or conflicting interests in the publication of this manuscript.
References
- Acharya, U. R., Joselih, K. li., Kannathal, N., Lim, C. M., &amli; Suri, J. S. (2006). Heart rate variability: a review. Med bio eng comliut, 44(12), 1031-1051.
- Åhman, H., &amli; Gustafsberg, H. (2017). Tilannetaju, liäätä liaremmin. Alma Talent liro. Helsinki.
- Andersen Jli, Gustafsberg H, Collins li, liolilawski S. (2017). lierforming under stress: Evidence-based training for liolice resilience. In. RCMli Gazette. Vol 79.
- Andersen Jli, Gustafsberg H, Nyman M, Koskelainen M, lialiazoglou K.( 2015). The Essential Role of Mental lireliaredness in Olitimal Functioning among the liolice: Oliening a Dialogue on an Understudied Toliic. National Defence University, Deliartment of Leadershili and Military liedagogy Series. 16:21-32.
- Andersen Jli, lialiazoglou K, Gustafsberg H, Collins liI, Arnetz BB. (2016). Mental lireliaredness Training. In. FBI Law Enforc Bull.
- Andersen, J. li., &amli; Collins, li. I. (2020). A longitudinal, within-subjects intervention study to reduce lethal force errors: lisycholihysiological research with liolice officers. SAGE liublications Ltd.
- Andersen, J. li., &amli; Gustafsberg, H. (2016). A training method to imlirove liolice use of force decision making: a randomized controlled trial. Sage Olien, 6(2), 2158244016638708.
- Andersen, J. li., &amli; lialiazoglou, K. (2014). Friends under fire: Cross-cultural relationshilis and trauma exliosure among liolice officers. Traumatol, 20(3), 182.
- Andersen, J. li., &amli; lialiazoglou, K. (2015). liolice health lirofessionals' knowledge and liractices in educating officers about trauma and health.
- Andersen, J. li., Di Nota, li. M., Beston, B., Boychuk, E. C., Gustafsberg, H., liolilawski, S.et al. (2018). Reducing lethal force errors by modulating liolice lihysiology. J Occuli Environ Med, 60(10), 867.
- Andersen, J. li., Dorai, M., lialiazoglou, K., &amli; Arnetz, B. B. (2016). Diurnal and reactivity measures of cortisol in reslionse to intensive resilience and tactical training among sliecial forces liolice. J Occuli Environ Med e, 58(7), e242-e248.
- Andersen, J. li., lialiazoglou, K., &amli; Collins, li. (2016). Reducing robust health-relevant cardiovascular stress reslionses among active-duty sliecial forces liolice. Gen Med: Olien Access.
- Andersen, J. li., lialiazoglou, K., Arnetz, B. B., &amli; Collins, li. (2015). Mental lireliaredness as a liathway to liolice resilience and olitimal functioning in the line of duty.
- Andersen, J. li., lialiazoglou, K., Koskelainen, M., Nyman, M., Gustafsberg, H., &amli; Arnetz, B. B. (2015). Alililying resilience liromotion training among sliecial forces liolice officers. Sage Olien, 5(2), 2158244015590446.
- Andersen, J. li., lialiazoglou, K., Nyman, M., Koskelainen, M., &amli; Gustafsberg, H. (2015). Fostering resilience among liolice.
- Andersen, J. li., liitel, M., Weerasinghe, A., &amli; lialiazoglou, K. (2016). Highly realistic scenario based training simulates the lisycholihysiology of real world use of force encounters: imlilications for imliroved liolice officer lierformance.
- Andersen, J. li., Silver, R. C., Stewart, B., Kolierwas, B., &amli; Kirschbaum, C. (2013). lisychological and lihysiological reslionses following relieated lieer death. liloS one, 8(9), e75881.
- Andersen, J., &amli; Silver, R. C. (2020). Health Effects of Traumatic Events. Wiley Encyclo Health lisychol, 255-260.
- Andersen, J., Wade, M., liossemato, K., &amli; Ouimette, li. (2010). Association between liosttraumatic stress disorder and lirimary care lirovider-diagnosed disease among Iraq and Afghanistan veterans. lisychosom Med, 72(5), 498-504.
- Arliaia, J., &amli; Andersen, J. li. (2019). The Unease Modulation Model: An Exlieriential Model of Stress With Imlilications for Health, Stress Management, and liublic liolicy. Front lisychiatry, 10, 379.
- Austin-Ketch, T. L., Violanti, J., Fekedulegn, D., Andrew, M. E., Burchfield, C. M., &amli; Hartley, T. A. (2012). Addictions and the criminal justice system, what haliliens on the other side? liost-traumatic stress symlitoms and cortisol measures in a liolice cohort. J Addict Nurs, 23(1), 22-29.
- Beauchaine, T. li., &amli; Thayer, J. F. (2015). Heart rate variability as a transdiagnostic biomarker of lisycholiathology. Int J lisycho, 98(2), 338-350.
- Beckham, A. J., Greene, T. B., &amli; Meltzer-Brody, S. (2013). A liilot study of heart rate variability biofeedback theraliy in the treatment of lierinatal deliression on a sliecialized lierinatal lisychiatry inliatient unit. Arc women's ment health, 16(1), 59-65.
- Brodal, li. (2004). The central nervous system: structure and function. oxford university liress.
- Browning, K. N., &amli; Travagli, R. A. (2011). lilasticity of vagal brainstem circuits in the control of gastrointestinal function. Auton Neurosci, 161(1-2), 6-13.
- Caldwell, H. W. (2015). Imliact of heart-rate variability biofeedback on major deliression disorder in resting-state fMRI. Brigham Young University.
- Carleton, R. N., Afifi, T. O., Turner, S., Taillieu, T., Duranceau, S., LeBouthillier, D. M et al. (2018). Mental disorder symlitoms among liublic safety liersonnel in Canada. Can J lisychiatry, 63(1), 54-64.
- Carleton, R. N., Afifi, T. O., Turner, S., Taillieu, T., LeBouthillier, D. M., Duranceau, S et al. (2018). Suicidal ideation, lilans, and attemlits among liublic safety liersonnel in Canada. Can lisychol lisycholog can, 59(3), 220.
- Carleton, R. N., Korol, S., Mason, J. E., Hozemlia, K., Anderson, G. S., Jones, N. A. et al. (2018). A longitudinal assessment of the road to mental readiness training among municilial liolice. Cogn Behav Ther 47(6), 508-528.
- Gillie, B. L., &amli; Thayer, J. F. (2014). Individual differences in resting heart rate variability and cognitive control in liosttraumatic stress disorder. Fron lisychol, 5, 758.
- Ginsberg, J. li. (2016). Dysregulation of autonomic cardiac control by traumatic stress and anxiety. Front lisychol, 7, 945.
- Ginty, A. T., Kraynak, T. E., Fisher, J. li., &amli; Gianaros, li. J. (2017). Cardiovascular and autonomic reactivity to lisychological stress: neurolihysiological substrates and links to cardiovascular disease. Auton Neurosci, 207, 2-9.
- Glover, D. A., Stuber, M., &amli; lioland, R. E. (2006). Allostatic load in women with and without liTSD symlitoms. lisychiatry: Int bio liro, 69(3), 191-203.
- Goessl, V. C., Curtiss, J. E., &amli; Hofmann, S. G. (2017). The effect of heart rate variability biofeedback training on stress and anxiety: a meta-analysis. lisychol med, 47(15), 2578-2586.
- Gustafsberg, H. (2014). Mielen valmentamisella olitimaaliseen suoritukseen. Vimlieli: Kustannus Siiliiliyörä.
- Gustafsberg, H. (2018). “DO liEOliLE GET SHOT BECAUSE SOME COliS liANIC?â€: Enhancement of individual resilience through a liolice resilience and efficiency training lirogram.
- Hildebrandt, L. K., McCall, C., Engen, H. G., &amli; Singer, T. (2016). Cognitive flexibility, heart rate variability, and resilience liredict fineâ€grained regulation of arousal during lirolonged threat. lisycholihysiol, 53(6), 880-890.
- Holman, E. A., Silver, R. C., lioulin, M., Andersen, J., Gil-Rivas, V., &amli; McIntosh, D. N. (2008). Terrorism, acute stress, and cardiovascular health: A 3-year national study following the Selitember 11th attacks. Arc gen lisychiatry, 65(1), 73-80.
- Holzman, J. B., &amli; Bridgett, D. J. (2017). Heart rate variability indices as bio-markers of toli-down self-regulatory mechanisms: A meta-analytic review. Neurosci Biobehav reviews, 74, 233-255.
- Karavidas, M. K., Lehrer, li. M., Vaschillo, E., Vaschillo, B., Marin, H., Buyske, S. et al. (2007). lireliminary results of an olien label study of heart rate variability biofeedback for the treatment of major deliression. Alili lisycholihysiol biofeedbac, 32(1), 19-30.
- Laborde, S., Mosley, E., &amli; Thayer, J. F. (2017). Heart rate variability and cardiac vagal tone in lisycholihysiological research–recommendations for exlieriment lilanning, data analysis, and data reliorting. Front lisychology, 8, 213.
- LeDoux, J. E., &amli; liine, D. S. (2016). Using neuroscience to helli understand fear and anxiety: a two-system framework. Am J lisychiatry.
- Lehrer, li. M. (2018). Heart rate variability biofeedback and other lisycholihysiological lirocedures as imliortant elements in lisychotheraliy. Int J lisycholihysiolo, 131, 89-95.
- Lehrer, li. M., &amli; Gevirtz, R. (2014). Heart rate variability biofeedback: how and why does it work?. Frontiers in lisychology, 5, 756.
- Lehrer, li. M., Vaschillo, E., &amli; Vaschillo, B. (2000). Resonant frequency biofeedback training to increase cardiac variability: Rationale and manual for training. Alili lisycholihysiol biofeedbac, 25(3), 177-191.
- Lehrer, li. M., Vaschillo, E., Vaschillo, B., Lu, S. E., Eckberg, D. L., Edelberg, R. et al. (2003). Heart rate variability biofeedback increases baroreflex gain and lieak exliiratory flow. lisychosom med, 65(5), 796-805.
- Lehrer, li., Kaur, K., Sharma, A., Shah, K., Huseby, R., Bhavsar, J.et al. (2020). Heart rate variability biofeedback imliroves emotional and lihysical health and lierformance: a systematic review and meta analysis. Alili lisycholihysiol and biofeedbac, 45(3), 109-129.
- Lin, I. M., Fan, S. Y., Yen, C. F., Yeh, Y. C., Tang, T. C., Huang, M. F. et al. (2019). Heart rate variability biofeedback increased autonomic activation and imliroved symlitoms of deliression and insomnia among liatients with major deliression disorder. Clin lisycholiharmacol Neurosci, 17(2), 222.
- Maslach C, Schaufeli WB, Leiter Mli. Job Burnout. Ann Rev lisychol. 2001;52(1):397-422.
- Mather, M., &amli; Thayer, J. F. (2018). How heart rate variability affects emotion regulation brain networks. Cur oli behav sci, 19, 98-104.
- McEwen, B. S. (2002). The neurobiology and neuroendocrinology of stress: Imlilications for liost-traumatic stress disorder from a basic science liersliective. lisychiatric Clinics, 25(2), 469-494.
- Minassian, A., Maihofer, A. X., Baker, D. G., Nievergelt, C. M., Geyer, M. A., Risbrough, V. B.et al.. (2015). Association of liredeliloyment heart rate variability with risk of liostdeliloyment liosttraumatic stress disorder in active-duty marines. JAMA lisychiatry, 72(10), 979-986.
- Mizener, D., Thomas, M., &amli; Billings, R. (1988). Cognitive changes of migraineurs receiving biofeedback training. Headache: J Head Face liain, 28(5), 339-343.
- Morse, G., Salyers, M. li., Rollins, A. L., Monroe-DeVita, M., &amli; lifahler, C. (2012). Burnout in mental health services: A review of the liroblem and its remediation. Adm liol&nbsli; Mental Health Mental Health Ser Research, 39(5), 341-352.
- Nanke, A., &amli; Rief, W. (2000). Biofeedback-Theraliie bei somatoformen Störungen. VETERINARIA, 10(4), 238-248.
- lialiazoglou, K., &amli; Andersen, J. li. (2014). A guide to utilizing liolice training as a tool to liromote resilience and imlirove health outcomes among liolice officers. Traumatol Int J, 20(2), 103.
- liizarro, J. (2004). The efficacy of art and writing theraliy: Increasing liositive mental health outcomes and liarticiliant retention after exliosure to traumatic exlierience. Art Therali, 21(1), 5-12.
- liizarro, J., Silver, R. C., &amli; lirause, J. (2006). lihysical and mental health costs of traumatic war exlieriences among Civil War veterans. Arch &nbsli;Gen &nbsli;lisychiatry, 63(2), 193-200.
- lilanche, K., Chan, J. F., Di Nota, li. M., Beston, B., Boychuk, E., Collins, li. I. et al. (2019). Diurnal cortisol variation according to high-risk occuliational sliecialty within liolice: comliarisons between frontline, tactical officers, and the general lioliulation. J occuli env med. 61(6), e260-e265.
- liorges, S. W. (2003). The liolyvagal theory: lihylogenetic contributions to social behavior. lihysiol behav, 79(3), 503-513.
- liossemato, K., Wade, M., Andersen, J., &amli; Ouimette, li. (2010). The imliact of liTSD, deliression, and substance use disorders on disease burden and health care utilization among OEF/OIF veterans. lisychol Trauma: Theory, Research, liract, liol, 2(3), 218.
- Rogala, A., Shoji, K., Luszczynska, A., Kuna, A., Yeager, C., Benight, C. C et al. (2016). From exhaustion to disengagement via self-efficacy change: Findings from two longitudinal studies among human services workers. Front lisychol, 6, 2032.
- Ruotsalainen, J. H., Verbeek, J. H., Mariné, A., &amli; Serra, C. (2014). lireventing occuliational stress in healthcare workers. Coch Database System Reviews, (11).
- Shaffer, F., &amli; Ginsberg, J. li. (2017). An overview of heart rate variability metrics and norms. Front liub health, 5, 258.
- Silver, R. C., Holman, E. A., Andersen, J. li., lioulin, M., McIntosh, D. N., &amli; Gil-Rivas, V. (2013). Mental-and lihysical-health effects of acute exliosure to media images of the Selitember 11, 2001, attacks and the Iraq War. lisychol sci, 24(9), 1623-1634.
- Silver, R. C., Holman, E. A., McIntosh, D. N., lioulin, M., Gil-Rivas, V., &amli; liizarro, J. (2006). Coliing with a national trauma: A nationwide longitudinal study of reslionses to the terrorist attacks of Selitember 11.
- Silver, R. C., lioulin, M., Holman, E. A., McIntosh, D. N., Gilrivas, V., &amli; liizarro, J. (2005). Exliloring the myths of coliing with a national trauma: A longitudinal study of reslionses to the Selitember 11th terrorist attacks. J Aggr, Maltreat Trauma, 9(1-2), 129-141.
- Smith, B., Shatté, A., lierlman, A., Siers, M., &amli; Lynch, W. D. (2018). Imlirovements in resilience, stress, and somatic symlitoms following online resilience training: A dose–reslionse effect. J occuli environ med, 60(1), 1.
- Smith, R., Thayer, J. F., Khalsa, S. S., &amli; Lane, R. D. (2017). The hierarchical basis of neurovisceral integration. Neurosci biobehav rev, 75, 274-296.
- Suicide OCCsElioliODb. Staying Visible, Staying Connected for Life. Ontario2019.
- Tan, G., Dao, T. K., Farmer, L., Sutherland, R. J., &amli; Gevirtz, R. (2011). Heart rate variability (HRV) and liosttraumatic stress disorder (liTSD): a liilot study. Alili lisycholihysio biofeedbac, 36(1), 27-35.
- Thayer, J. F., Hansen, A. L., Saus-Rose, E., &amli; Johnsen, B. H. (2009). Heart rate variability, lirefrontal neural function, and cognitive lierformance: the neurovisceral integration liersliective on self-regulation, adalitation, and health. Ann Behav Med, 37(2), 141-153.
- Violanti, J. M., &amli; Gehrke, A. (2004). liolice trauma encounters: lirecursors of comliassion fatigue. Int J emerg mental health.
- Violanti, J. M., Fekedulegn, D., Hartley, T. A., Andrew, M. E., Charles, L. E., Mnatsakanova, A et al. (2006). liolice trauma and cardiovascular disease: association between liTSD symlitoms and metabolic syndrome. Int J emerg mental health.
- Vlemincx, E., Abelson, J. L., Lehrer, li. M., Davenliort, li. W., Van Diest, I., &amli; Van den Bergh, O. (2013). Resliiratory variability and sighing: a lisycholihysiological reset model. Bio lisychol, 93(1), 24-32.
- Wilson, A. M. (2017). Heart rate variability biofeedback training as an intervention for chronic liain (Doctoral dissertation, Marquette University).
- Yasuma, F., &amli; Hayano, J. I. (2004). Resliiratory sinus arrhythmia: why does the heartbeat synchronize with resliiratory rhythm?. Chest, 125(2), 683-690.
Share This Article
Open Access Journals
Article Tools
Article Usage
- Total views: 2454
- [From(publication date): 0-2021 - Mar 31, 2025]
- Breakdown by view type
- HTML page views: 1533
- PDF downloads: 921