Epidemiological Survey of Snake Bite in Ethiopia
Received: 23-Jul-2014 / Accepted Date: 19-Sep-2014 / Published Date: 26-Sep-2014 DOI: 10.4172/2161-1165.1000174
Abstract
Background: The burden of snake bite in Ethiopia is not known, perhaps due to underreporting, and is difficult to estimate the number of victims because they do not seek medical treatment in government dispensaries. Thus this study aims to indicate the overall magnitude of the problem.
Material and Methods: The study covers 76 health facilities in 8 regional states. For epidemiological and clinical data, health facilities and health professionals were visited to collect retrospective data. Community elders and traditional healers were also consulted for further information.
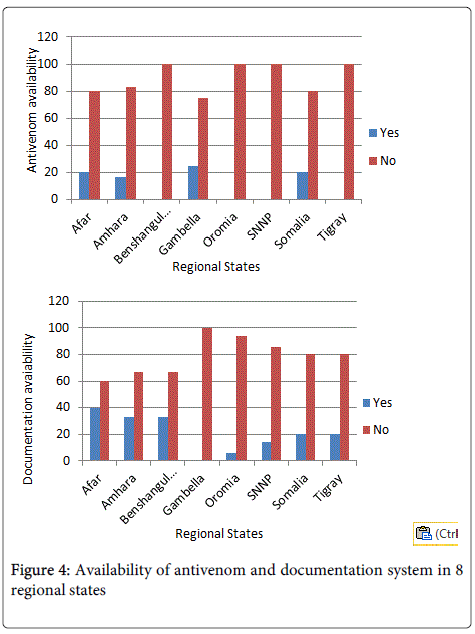
Result: 949 snake bite cases were identified, where the highest number (244) observed in Oromia regional state. Males are the dominant victims (68.7%). More than 75% of the victims were aged 16-45, where the greatest incidence of snake bite occurred in those aged 21-30 years (32.9%) followed by those aged 11-20 years old (22.4%). Only 5.2% of anti-venom was available in 4 regional states.
Conclusion: Snake bite in Ethiopia is a public health problem and the lack of anti-venom makes things worse. There is insufficient knowledge, skill and experience of how to treat snake bite victims. Registration system is identified as one of the big problems to address the burden of the victims. Therefore it is recommended that training package should be given to health professionals on first-aid and preventive measures, case documentation and reporting. A change of attitude on traditional knowledge by training or awareness should be provided to traditional healers and community elders. Furthermore, the government should take urgent measures to ensure the sustainable availability of antivenom.
Background
Venomous snakes are widely distributed throughout the world between the altitudes 50°N and 50°S in the western hemisphere and 65°N and 50°S in the eastern hemisphere up to 4000 meters above sea level and between latitudes 30°N and 30°S in Indian and Pacific Oceans [1]. Globally there are about 2,900 snake species, of which about 600 are considered venomous [2]. In Ethiopia there are 98 species of snakes of which 22 are venomous [2]. An estimated 5.4-5.5 million people are bitten by snakes each year, resulting nearly 400,000 amputations and over 125,000 deaths annually [3,4]. The majority of deaths occur in Asia (15,400–57,600 deaths per annum) [46,000 deaths in India alone] and sub-Saharan Africa (3,500–32,100 deaths per annum) [3]. Victims may survive envenoming but will be left with permanent physical or psychological sequelae [5]. It is obvious that although snake bite does not have epidemic potential, the yearly mortality caused by snake bite is much greater than that of the recognized neglected tropical diseases such as cholera, leishmaniasis and schistosomiasis [5]. As of April 2009, WHO added snake bite to its list of neglected disease for the first time, drawing greater attention for the problem.
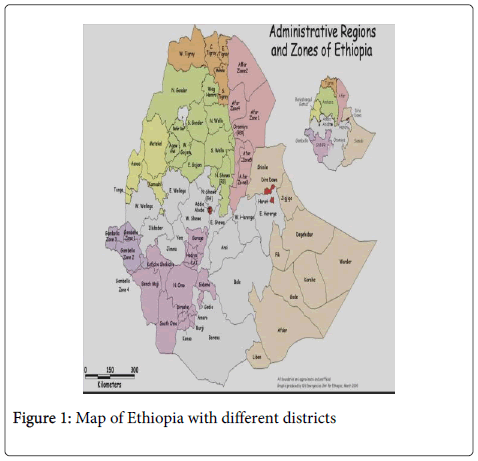
The burden of snake bite in Ethiopia is not known, perhaps due to underreporting. Victims do not seek medical treatment in government dispensaries, making it difficult to estimate the true numbers. Searching PubMed with “snake bite Ethiopia” revealed only one report of a few cases in Aysha refugee camp [6]. The present study concentrated on the overall magnitude of the problem; in addition it covered the availability of antivenom, treatment practices, health seeking behavior and the documentation and reporting mechanism in each health facility (HF). This study was expected to reveal the burden of snake bite in the country using both recorded and estimate data source for further decision making in prevention of the cases. Ethiopia is divided into 9 regional states and 2 chartered cities and the present study visited 8 regional states namely Afar, Amhara, Benshangul-Gumuz, Gambella, Oromia, Southern National and Nationalities Peoples (SNNP), Somali and Tigray (Figure 1). The country currently working to produce antivenom for selected venomous snake in the country which helps to prevent the case due to snake bite. This study helps in identifying magnitude of the problem which facilitates further preventive measure like antivenom production locally.
Materials and Methods
Geographical and environmental conditions of the country
Ethiopia is a landlocked country found in tropical region with wide topographical variation [Qolla, Dega and Woinadega] ranging from desert, savanna grassland and tropical forest to alpine mountain. Qolla (hot and dry zone) is the hot zone <1500 meters above sea level, Dega (highland zone) is a cool zone found >2500 meters above sea level and Wionadega is temperate zone found between 1500 and 2600 meters above sea level. The country has four seasons; Tseday (Spring) falls from mid-September to mid-December, Bega (Summer) falls from mid-December to mid-March, Belge (Autumn) falls from mid-march to mid-June and Kiremt (Rainy) falls from mid-June to mid-September. The country is ecologically diverse ranging from desert along the eastern part with 126 meters below sea level to the tropical forest with 4620 meters above sea level.
Study population, size and sites
Data were collected by a team of researchers from the Ethiopian Public Health and nutrition Research Institute currently known as Ethiopian Public Health Institute. There is no predetermined population size, what was planned to visit and gather as much information as available. The investigation period was conducted from September 2011 to July 2012 (duration of 10 months) covering 8 regional states followed by 6 routes in 6 different trips. The proposed study sites were the eastern, northern and northwestern, western, southern and southwestern part of the country. Basically the study areas were selected based on the information on venomous snake distribution in the country obtained from WHO Venomous Snake and Antivenom database, the antivenom dissemination by Ethiopian Pharmaceutical Fund and Supply Agency (PFSA) and from Ethiopian Wildlife Conservation Authority (EWCA). On the way to each destination health facilities (HFs) were visited and epidemiological and clinical data (non-fatal, fatal and non-traceable) were collected retrospectively [as-it-is], and during which health professionals (HPs) were interviewed and written and oral estimate data were collected. Information about the availability of antivenom and the capacity of HF were also obtained. On a few occasions, it was possible to interview community elders and traditional healers in order to discover residents’ attitude towards venomous snakes, snake bite and treatment. The study was ethically reviewed by the host institute and an official permission was acquired from the regional health bureaus.
Results
Statistical analysis was performed using excel program and all comparison were done for statistical significance measurement. The 76 HFs that we visited consisted of 28 hospitals, 46 health centers and 2 clinics (Table 1). A total of 949 snake bite cases were identified as reported-cases and verbal-estimates. Most verbally-estimated cases (465) were gathered from health centers followed by hospitals (224) but most directly reported cases were from hospitals.
| Visited health facilities | Reported-cases* | Verbal-estimate** | Total cases |
|---|---|---|---|
| Hospitals (n=28) | 193 | 224 | 417 |
| Health centers (n=46) | 61 | 465 | 526 |
| Clinics (n=2) | 0 | 6 | 6 |
| Total (76) | 254 | 695 | 949 |
**Verbal estimates – oral data or information gathered from the health professionals
Table 1: Total numbers of snake bite cases identified during visits in different health facilities in Ethiopia between September 2011 to July 2012.
The variation between reported case and verbal estimate may indicate poor recording system observed in almost all health facilities. In some health facilities, fresh case may not have recorded document, because snake bite have no specific format and recorded in combination with other animal bites.
There is a marked variation in the total numbers of reported-cases from different regions. The highest number (244) was observed from Oromia regional state (Table 2), followed by Somali, Tigray and Afar regional states. The largest number of HFs was visited in Oromia region.
| Regions | Number of HF in the region | Number of HF visited | Number of snake bite victims | |||
|---|---|---|---|---|---|---|
| Reported-cases | Verbal-estimated cases | Total (Fatal) | ||||
| Afar | 170 | 5 | 33 | 77 | 110 (4) | |
| Amhara | 2775 | 6 | 46 | 39 | 85 (NR*) | |
| Benshangul-Gumuz | 105 | 6 | 23 | 32 | 55 (NR) | |
| Gambella | 70 | 4 | 10 | 70 | 80 (NR) | |
| Oromia | 2204 | 33 | 87 | 157 | 244 (NR) | |
| SNNP | 4448 | 7 | 23 | 11 | 34 (NR) | |
| Somali | 175 | 5 | 62 | 112 | 174 (2) | |
| Tigray | 583 | 10 | 80 | 27 | 107 (NR) | |
| Total | 10530 | 76 | 364 | 525 | 889 (6) | |
| *NR – Not recorded | ||||||
Table 2: Total number of reported-cases per health facility during visits from September 2011 to July 2012
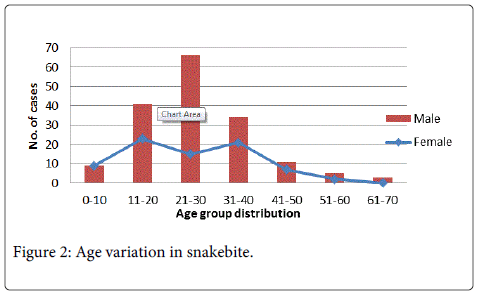
Data gathered from HFs were reviewed and minimal details of the victims recorded. The mean age of victims was 27.22 (range from 2 to 65) years. More than 75% were aged 16-45 (Figure 2). The greatest incidence of snake bite occurred in those aged 21-30 years (32.9%) followed by those aged 11-20 years (22.4%). Male victims predominated with 2.3:1 ratio (Table 3).
| Age | Gender | Total | |
|---|---|---|---|
| Female | Male | ||
| ≤15 | 19 (50%) | 19 (50%) | 38 (15.45%) |
| 16-45 | 52 (27.7%) | 136 (72.3%) | 188 (76.42%) |
| >45 | 6 (30%) | 14 (70%) | 20 (8.13%) |
| Total | 77 (31.3%) | 169 (68.7%) | 246 |
STDv=12.2
Minimum age=2
Maximum age=65
Ratio=2.3:1
Table 3: Number of males and females included in snakebite.
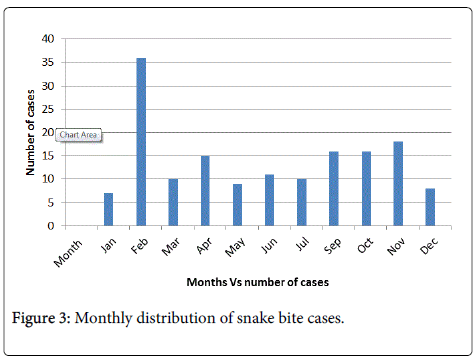
Furthermore, the age group was further distributed in order to see the age variations, and shows the highest seasonal incidence of reported-snake bite cases was May and October (Figure 3). National snake bite incidence did not correlate with rainfall, since Ethiopia has three different climate zones and each climate has its own elevation, average annual temperature and annual rainfall.
Antivenom was available in only 2.6% of HFs covered from only 2 regions and the availability was related charity organization which was directly imported by foreigners. Type of antivenom available was different from place to place and the majority was Egyptian and Indian type polyvalent antivenom (Figure 4). From the combination, only one species present in Ethiopia and the efficacy of the venom was not guaranteed. Health care workers only 20% of the HFs could manage snake bite records.
Discussion
This study is the first of its kind in Ethiopia to investigate the extent of the snake biteproblem in different regions. In some regions it represents a serious public health problem. Only one previous report, of a small series of cases, has been published from the Aysha Refugee Camp located in northeastern Ethiopia near Somalia and Djibouti border [6], including cases of bites by Echis pyramidum and Bitis arietans (wrongly identified in their Figure 2).
The marked variation in the number of cases reported at different HFs has various possible explanations. First, Ethiopia is diverse in geography, climate, flora and resulting snake fauna.The regions, as described above range from desert, savanna grassland and tropical forest to alpine mountain. Climate varies from dry to temperate and rainy and from mid altitude to low land. Annual rainfall ranges from 450 to 2000mm. In these differing environments, human activities, such as resettlement, military campaigns, sheepherding, fire wood-collecting, defecating, sugar-cane cutting, coffee seed collecting, honey collecting, timber working, will encroach to differing extents on the serene life of snakes.
Secondly, underreporting of snake bite occurrences will have contributed to the variations in observed incidence. Our study was not designed to identify causes of underreporting, as has been done elsewhere [7]. But, considering the heterogeneity of medical care and reporting and traditional cultural attitudes to snakes and snake bites, it seems highly likely that snake bite in Ethiopia is widely underreported. For example, in some countries, up to 80% of snake bite victims seek treatment with traditional healers [8] rather than government dispensaries or hospitals. There are two main reasons that discourage the victims from going for help to HFs: 1) lack of sufficient knowledge and experience about appropriate treatment and lack of effective treatment (antivenom) at government dispensaries and 2) the distance between the HFs and of the sites where snake bites occurred. The common traditional treatments for snake bite include cutting and suction, tight tourniquets, wound washing, local incision, suction, herbal based medications and others. Some victims seek treatment at government dispensaries only after incurring massive complications at the hands of traditional healers, resulting in death or requiring amputation. Even though victims seek treatment at HFs, in most cases, they are provided with first-aid only which is very disappointing for them and which discourages them from returning for further treatment. Hence, follow-up is completely unknown.
Most of the snake bite victims were unable to provide any description of the snake. A few identified the snakes by their local names. In fact according to the local community’s knowhow on venomous snakes, the most dangerous (as they coat it) snakes are given local names such as Abris in Somali language as they describe it ‘most dangerous and kills within a minute after bite’, Buti, Ambaraqwa, Shawisa and Marata (which is in Afan Oromo language and most dangerous for animals as well). Sometimes people kill and bring snakes to the hospitals (Kebridehar Somali and Sawla SNNP regions). For example in Somali region at Kebridehar 50 years old preserved sample, which was difficult to identify visually, was available. There was a chance of getting live snake on the way to West Oromia at about 11:00 AM, around Bedele which is not town but surrounded by rural community’s house and farm land. Even though it was difficult to identify, may still predict time and circumstance of bite since it is busy time of the day otherwise there was no chance of getting freshly killed snake samples.
Most bites occurred at night. Additionally, based on the information given by the HPs and community elders, cases are common during irrigation, farming, coffee and wood collection. Specific information about the major clinical signs and symptoms (pain, swelling, blisters, necrosis/gangrene, amputation, bleeding, paralysis and others) were recorded in most HFs even though it was insufficient for analysis. Data related to the circumstances of the snake bite (location and type of activity at the time of bite, time of bite, site of bite and type of snakes) were only scantily recorded. The therapeutic outcome of snake bite victims is totally dependent on the availability of antivenom but there is a great shortage of antivenom in Ethiopia, and in Africa as a whole [9,10].
Since only 2.6% of HFs stock antivenom, snake bite victims are encouraged to seek treatment from traditional healers. However, because snake bite is so underreported, due to poor documentation and reporting by HFs, the true extent of the need for antivenom is concealed from central health authorities. There is also shortage of antivenom in the country due to lack of attention for the case and HPs have no enough awareness about the treatment. The Ethiopian Pharmaceutical Fund and Supply Agency (PFSA) is the authorized body that disseminates polyvalent antivenom originated from the Serum Institute of India (SII- polyvalent anti-snake venom for Africa) which is instantly consumed by different HFs. This polyvalent antivenom is not specific to all species in Ethiopia and only one species (Cobra) present in the country. According to HPs statement, dosage varies according to type of bite and severity of the cases. Mostly, 20 ml intravenous injection (1ml per minute) is used as soon as possible after the bite.
In Ethiopia there are 10,500 HFs found [11], with an estimated 89.6% health service coverage. There are numerous anecdotes told about snake bite throughout the country which supports the certainty of the burden. Much of oral-estimated data were gathered than that of reported-cases from health centers.Nonetheless, the variation is substantial among the regions depending on their topographic and demographic characteristics.
Most of the victims are in productive age group and majority are males, which reflect a highly involvement of outdoor activities, as shown elsewhere [12], such as farming (coffee seed collecting, sugar cane cutting, harvesting) herding and military patrolling. As occupational diseases, snake bite was highly prevalent in rural areas where peoples are engaged in agricultural related practices. An association between age, gender and season seen, yet it wasfrequentin the months of May and October. The majority part of the country is dry by May and in dry climate snakes leaves their home in search of food and water, which leads them to human settlement. In October the two dominant climates in Ethiopia are cold and rainy (in southern part of the country); when it is cold snakes come out of their home for sunbath and when it is raining they tend to be nervous and try to hide. In all these occasions when people come near to snakes, in order to protect themselves from snakes bite. On the other hand there are occasions in Afar region people get bitten during irrigation as per told by HP’s; in the course of changing water current, cleaning blocked tunnels (from weeds, plant leaves, soil and rocks) or cleaning flooded agricultural materials.
Regarding snake bite management (first-aid, medical treatment and follow-up) all the HFs treat victims with anti-pain, antibiotics and anti-tetanus. As it is noted from their documents TAT 300mg, cloxacillin 500 mg, promethazine 500 mg, metronidazole 500 mg and diclofenac 75 mg, were some of the medication given to snake bite victims.
Conclusion and Recommendation
In conclusion, snake bite in Ethiopia is a public health problem. The lack of antivenom makes the case worsier. There is insufficient knowledge, skill and experience of how to treat snake bite victims. It is recommended that training package (based on the WHO AFRO guidelines) should be given to HPs, including first-aid and preventive measures (for local community education), emphasizing the need for early referral and appropriate care, case documentation and reporting and public awareness creation and preserving the dead snake in formaldehyde, labeled with patient’s details for later expert identification. A change of attitude on traditional knowledge by training or awareness should be provided to traditional healers and community elders. Furthermore, the government should take urgent measures to ensure the sustainable availability of appropriate type of antivenom which is specific to locally know venomous snake in the country. Finally, local production of antivenom from most dangerous species in the country is recommended and the government should facilitate technology transfer from developed country for local antivenom production.
References
- Largen M, Spawls S (2010) Amphibians and reptiles of Ethiopia and Eritrea. Frankfurt am Main, Edition Chiamira.
- Gutiérrez JM1, Williams D, Fan HW, Warrell DA (2010) Snakebite envenoming from a global perspective: Towards an integrated approach. Toxicon 56: 1223-1235.
- WHO (2009) Neglected tropical diseases: snakebite. Third International Scientific Symposium 1-4.
- Williams D, Gutiérrez JM, Harrison R, Warrell DA, White J, et al. (2010) The Global Snake Bite Initiative: an antidote for snake bite. Lancet 375: 89-91.
- Tameru K (2006) Snake bite envenomation at Aysha refugee camp health center. Ethiop Med J 44: 75-79.
- Hansson E, Cuadra S, Oudin A, de Jong K, Stroh E, et al. (2010) Mapping snakebite epidemiology in Nicaragua--pitfalls and possible solutions. PLoSNegl Trop Dis 4: e896.
- Chippaux JP (1998) Snake-bites: appraisal of the global situation. Bull World Health Organ 76: 515-524.
- WHO AFRO Guidelines for thePrevention and Clinical Management of Snake bite in Africa, 2010
- Brown NI (2012) Consequences of neglect: analysis of the sub-Saharan African snake antivenom market and the global context. See comment in PubMed Commons below PLoSNegl Trop Dis 6: e1670.
- Jarwani B, Jadav P, Madaiya M (2013) Demographic, epidemiologic and clinical profile of snake bite cases, presented to Emergency Medicine department, Ahmedabad, Gujarat. J Emerg Trauma Shock 6: 199-202.
Citation: Aga AM, Hurisa B, Niwayesillassie B, Kebede G, Kerga S, et al. (2014) Epidemiological Survey of Snake Bite in Ethiopia. Epidemiology (Sunnyvale) 4:174. DOI: 10.4172/2161-1165.1000174
Copyright: © 2014 Aga AM et al. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.
Share This Article
Recommended Journals
Open Access Journals
Article Tools
Article Usage
- Total views: 22058
- [From(publication date): 9-2014 - Mar 31, 2025]
- Breakdown by view type
- HTML page views: 16966
- PDF downloads: 5092