Review Article Open Access
3D Ultrasound Assessment of the Uterus: Why an Accuracy Study for Mullerian Congenital Anomalies is not Feasible, while Screening Already is, and should be done
Tudorache S1, Florea M1, Dragusin R1, Patru LC1, Dragoescu A2, Iliescu DG1* and Cara ML3
1Department of Obstetrics and Gynecology, Prenatal Diagnostic, University of Emergency Hospital, University of Medicine and Pharmacy, Craiova, Dolj, Romania
2Department of Intensive Care and Pharmacy of Craiova, University of Emergency Hospital, University of Medicine and Pharmacy of Craiova, Craiova, Dolj, Romania
3Department of Public Health, University of Medicine and Pharmacy of Craiova, Craiova, Dolj, Romania
- *Corresponding Author:
- Iliescu Dominic Gabriel
Department of Obstetrics and Gynecology
University Emergency Hospital
University of Medicine and Pharmacy of Craiova, Craiova, Dolj, Romania
Tel: +4 0723 888773
Fax: +4 0251 502179
E-mail: dominic.iliescu@yahoo.com
Received Date: December 27, 2016; Accepted Date: January 28, 2017; Published Date: February 02, 2017
Citation: Tudorache S, Florea M, Dragusin R, Patru LC, Dragoescu A, et al. (2017) 3D Ultrasound Assessment of the Uterus: Why an Accuracy Study for Mullerian Congenital Anomalies is not Feasible, while Screening Already is, and should be done. J Clin Diagn Res 5:134. doi: 10.4172/2376-0311.1000134
Copyright: © 2017 Tudorache S, et al. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.
Visit for more related articles at JBR Journal of Clinical Diagnosis and Research
Abstract
The review covers the recently published research regarding the assessment of congenital mullerian anomalies by means of 3-dimensional transvaginal ultrasound. It is a plea toward standardization, defining diagnostic criteria, specifying the diagnostic methods and screening on daily basis with 3D ultrasound for congenital uterine anomalies. Many debates surrounded the most appropriate approach of mullerian anomalies diagnosis. In congenital uterine anomalies 3D ultrasound is critical in reaching the correct diagnosis. Before the routine use of 3D scanning for uterine anomalies is recommended, research should be dedicated to reproducibility of the diagnosis of uterine abnormalities. “Volumetric criteria” for the diagnosis of female genital anomalies should probably be elaborated, because we still face the lack of agreement in regards to diagnostic standards. There is very limited information on the reproductive risk associated with an incidental diagnosis of congenital uterine anomaly and the true prevalence in general population in not known. In order to achieve this objective, a relatively large amount of data needs to be collected. Uterine anomalies being rare, this can only be achieved by establishing a wide international collaboration involving a large number of research centers. 3D ultrasound is the only diagnostic method available to facilitate such collaboration. By submitting the archived 3D volumes, the operator dependence, the subjective bias in the assessment of uterine morphology and the selection bias would be almost completely eliminated. 3D ultrasound represents the most major development in gynaecological ultrasound imaging, providing a unique, very different way of displaying ultrasound data.
Keywords
Screening; Songenital uterine anomalies; Mullerian anomalies; 3-Dimensional ultrasound; Routine care
Introduction
Congenital malformations of the female genital tract are common miscellaneous deviations from normal anatomy. Pioneers in the field published comparative studies between 2D, 3D and HSG with regards to the assessment of uterine anomalies since the 90s (speaking of “planar reformatted sections”) [1]. Since long before that, uterine congenital anomalies have been associated with infertility, recurrent pregnancy loss, prematurity and other obstetric complications which increase perinatal morbidity and mortality rates [2,3,4], malpresentations, cervical incompetence [5], abruptio, whereas in others, these uterine malformations are asymptomatic [6,7]. Still, recognition of this group of congenital anomalies is far from clear.
Methods of Investigation of Mullerian Anomalies
Hysterosalpingography
The oldest investigation used to assess the shape of the uterus is Hysterosalpingography (HSG). For decades, it was considered the gold standard, being the pillar of sterile patients’ management plan. As years went by, many disadvantages of HSG became apparent, and this method is nowadays considered almost entirely outdated:
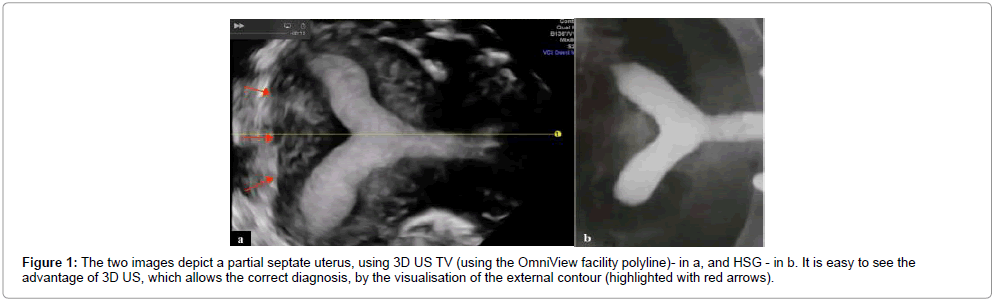
It has a low accuracy, assessing the endoluminal contour only, and not the external contour. Thus, has no potential to discriminate between the septate and bicornuate uter, two entities with radically different prognosis and treatment. It was reported with a 44.4% sensitivity [8] and 55% accuracy (Figure 1) [9,10].
It has the ability to characterize patent canals only. Expose patients to ionizing radiation, ovaries receiving a small dose of radiation. Although Karande indicate [11] that the level of radiation exposure is well within established margins of safety, the risk to the unfertilized ova is unknown. This is important, because these are typically young women and with reproductive difficulties.
A procedure-related pain occurs in up to 72% of patients undergoing HSG for the investigation of infertility [12]. The procedure may be complicated by pelvic inflammatory disease, especially if there is evidence of tubal disease when the test is performed. This is present in many cases, and especially if there is immunologic evidence of Chlamydia trachomatis [13]. It is highly operator-dependent. Depending on the setting, in many cases is not performed by a gynaecologist, the ideal observer for interpretation of the images.
Carries a high risk for allergies (induced by the contrast agents used) [14].
Due to tubal spasm, it does not always accurately assess the tubes (intravenous administration of scopolamine or rotation of the investigation bed is sometimes necessary) [15]. The main advantage of HSG is allowing concomitant assessment of tubal patency.
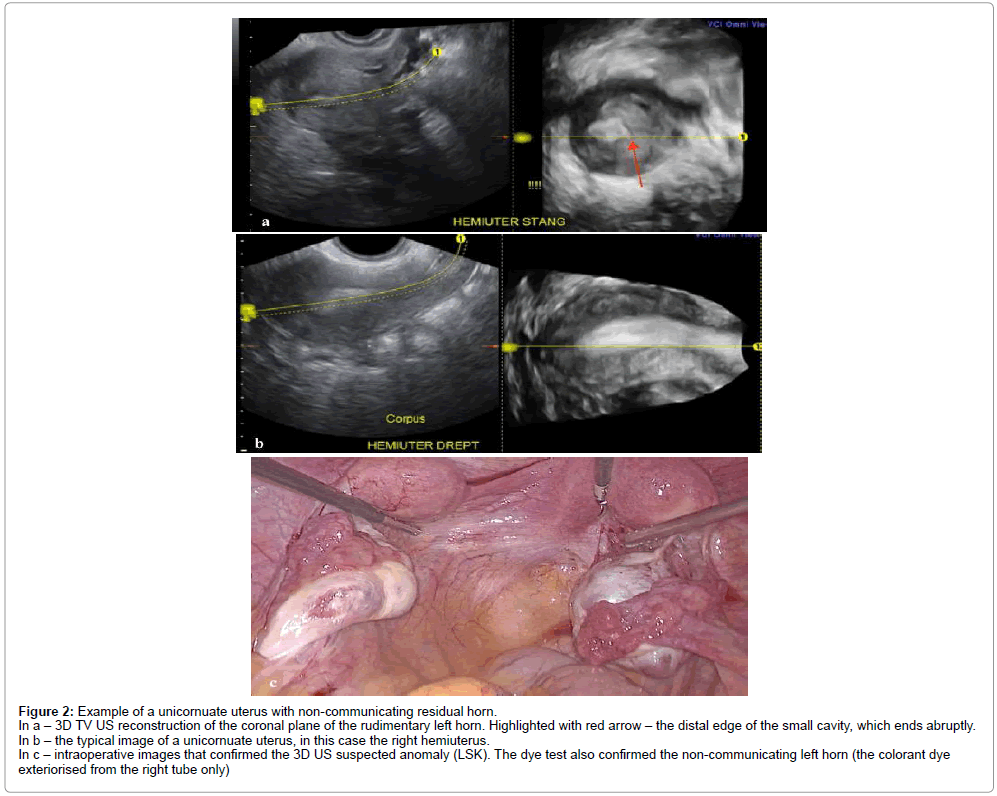
Combined laparoscopy and Hysterosalpingography
Until 2000, the combined use of laparoscopy (LSK) and hysteroscopy (HSK) was considered the gold standard for diagnosis of mullerian duct anomalies, due to the capabilities to assess the external and internal contour, respectively (Figure 2) [16-20]. Still, in many cases the two investigations are separately performed by different operators, and thus, the diagnosis accuracy may be influenced.
Figure 2: Example of a unicornuate uterus with non-communicating residual horn.
In a – 3D TV US reconstruction of the coronal plane of the rudimentary left horn. Highlighted with red arrow – the distal edge of the small cavity, which ends abruptly.
In b – the typical image of a unicornuate uterus, in this case the right hemiuterus.
In c – intraoperative images that confirmed the 3D US suspected anomaly (LSK). The dye test also confirmed the non-communicating left horn (the colorant dye
exteriorised from the right tube only)
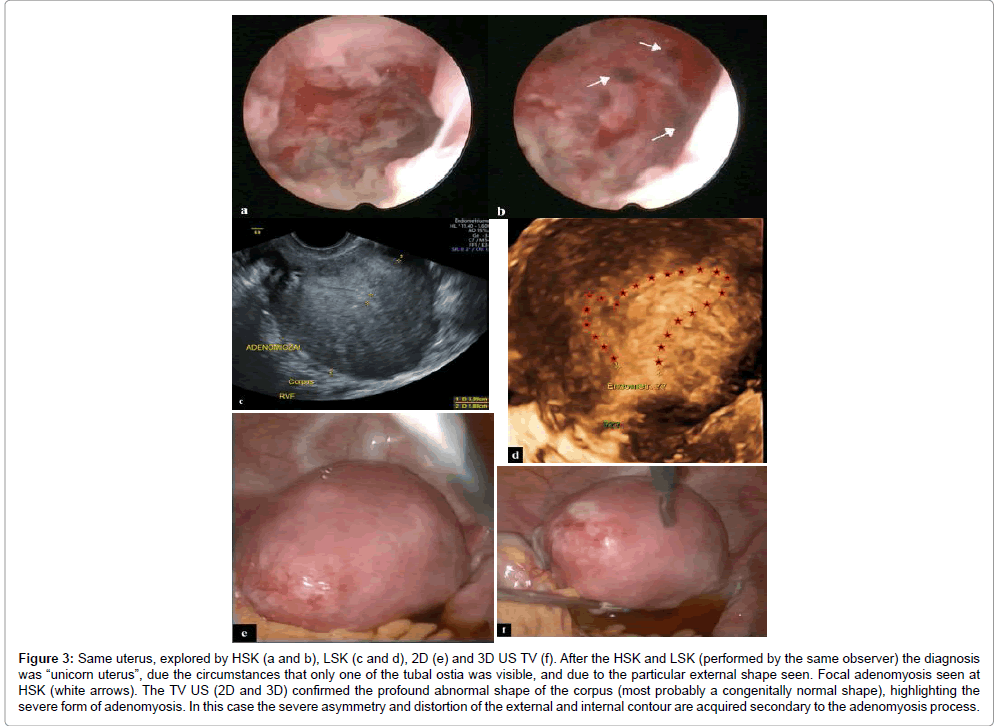
Histeroscopy alone
Lately, the accuracy of HSK alone has been severely questioned. Although used by some researchers as a gold standard for the examination of the cervical canal and internal aspects of the uterine cavity, HSK does not provide any information on the myometrial layer, nor on the width/length of a uterine septum in septate uteri. Moreover, at times, it is difficult to assess the shape of the uterus, especially in the absence of a device that offers panoramic views, and especially in uterus that associate evolving diseases (Figure 3).
Figure 3: Same uterus, explored by HSK (a and b), LSK (c and d), 2D (e) and 3D US TV (f). After the HSK and LSK (performed by the same observer) the diagnosis was “unicorn uterus”, due the circumstances that only one of the tubal ostia was visible, and due to the particular external shape seen. Focal adenomyosis seen at HSK (white arrows). The TV US (2D and 3D) confirmed the profound abnormal shape of the corpus (most probably a congenitally normal shape), highlighting the severe form of adenomyosis. In this case the severe asymmetry and distortion of the external and internal contour are acquired secondary to the adenomyosis process.
Limitations of traditional methods of investigation
Both HSG and HSK are limited in the assessment of the uterine cavity and are unable to differentiate reliably between the septate, subseptate, arcuate, and bicornuate uterus. Even when these methods are combined with LSK, the diagnosis relies on the subjective impression of the clinician rather than strict diagnostic criteria. This aspect is important in cases with just a small indentation of the external contour, which is critical in the bicornuate uterus.
With that approach (LSK and HSK), subtle differences in uterine morphology may be very difficult to assess, and the only way to describe uterine anomalies is by using 3DUS.
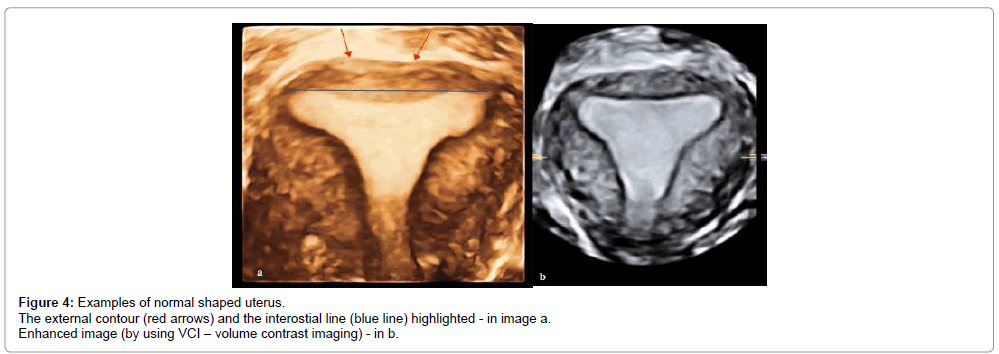
3D ultrasound
The first publications in regards to the potential of 3D of confirming the internal structure of the uterus, as seen by means of histerosalpingography (HSG), date back to 1995. In one of the early pioneering studies, Campbell et al. Found agreement between 3DUS and HSG in all cases, and moreover, considered that 3DUS further aided the differential diagnosis between the subseptated and bicornuate uteri, because of the ability to assess the external contour [1]. With the 3D TV technique, it is always possible to obtain the coronal view of the uterus, which is usually lying perpendicular to the ultrasound beam [21,22]. The analysis of uterine morphology should be performed in this standardized plane using, the interstitial portions of the Fallopian tubes as reference points. An even more comprehensive evaluation of uterine morphology has become feasible by transvaginal ultrasound (TV US).
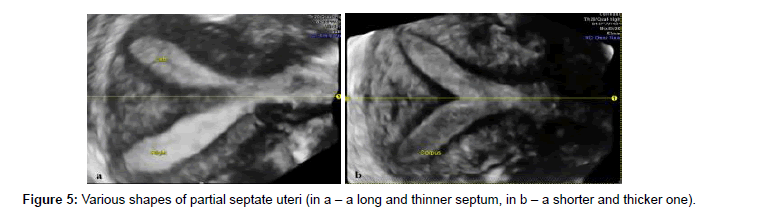
With 3D TV US, both the external contours and internal morphology of the uterus may be displayed on the coronal plane, and the presence and type of uterine anomaly may be accurately detected (Figures 3-5).
3DUS overcomes all limitations, by providing the coronal view of the uterus, which can rarely be seen so clearly, even when using MRI (due to the relatively small size of the normal uterus). The coronal view enables the clinician to examine both the endometrial cavity and uterine fundus, thus providing all information necessary for a complete assessment of uterine morphology [23-27]. Measurements of uterine septum and other features of uterine anomalies allow the possibility of comparisons between the degree of uterine distortion and reproductive outcomes [26,27].
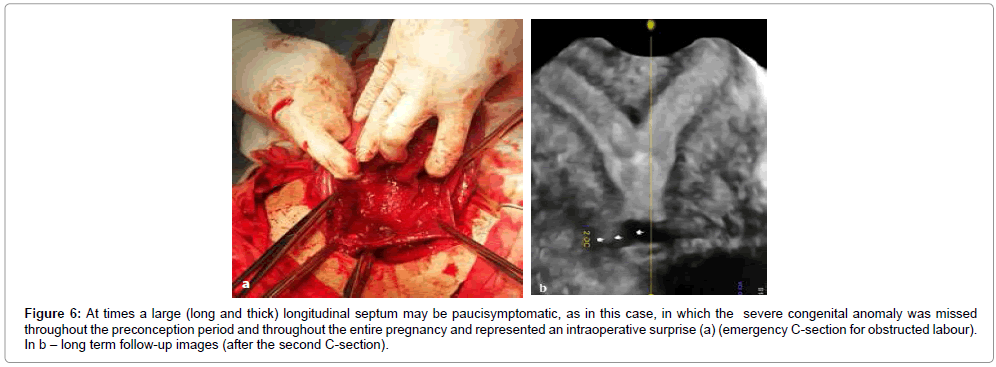
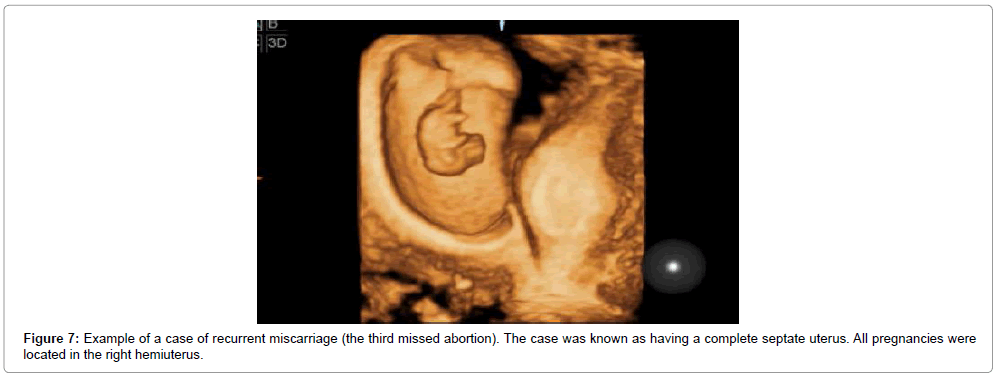
Raga et al, made one of the first attempts to correlate the mullerian anomalies with their reproductive impact, in a retrospective research [28]. In a study on almost 3200 patients that had been investigated with HSG and laparoscopic (LSK)/open surgery, mullerian anomalies had a 4% overall incidence: 3.8% in fertile woman, 6.3% in infertile ones and 2.4% in sterility cases. He also found that the most frequent type of the various anomalies is the septate and arcuate uterus. Based on the chances of having a living child (in unicornuate and didelphys uterus 37-40%, in bicornuate and septate 62.5%, arcuate-82.7%), he concluded that the arcuate uteri is a mild form of mulllerian anomaly and has no or very little impact on the reproductive outcome. Later studies confirmed a 3-4% incidence, with less than half of cases having clinical symptoms (Figure 6) [7]. Many subsequent studies on the classification of uterine morphology also reported high levels of agreement between 3D US, HSG and LSK (Figure 7) [1,8,9,16-20].
Figure 6: At times a large (long and thick) longitudinal septum may be paucisymptomatic, as in this case, in which the severe congenital anomaly was missed throughout the preconception period and throughout the entire pregnancy and represented an intraoperative surprise (a) (emergency C-section for obstructed labour). In b – long term follow-up images (after the second C-section).
In our view, screening with 3DUD TV for uterine anomalies should be part of routine clinical investigations of women presenting for gynecology visits, regardless the history of all mentioned above.
Conventional methods (HSG, HSK, LSK) should be restrained as second line investigations, due to the circumstance that all these methods are invasive and inaccurate, involving the subjective impression of the operator performing the test.
3D TV US has become nowadays the method of choice in assessing the uterus, due to many reasons and having distinct advantages over all other techniques:
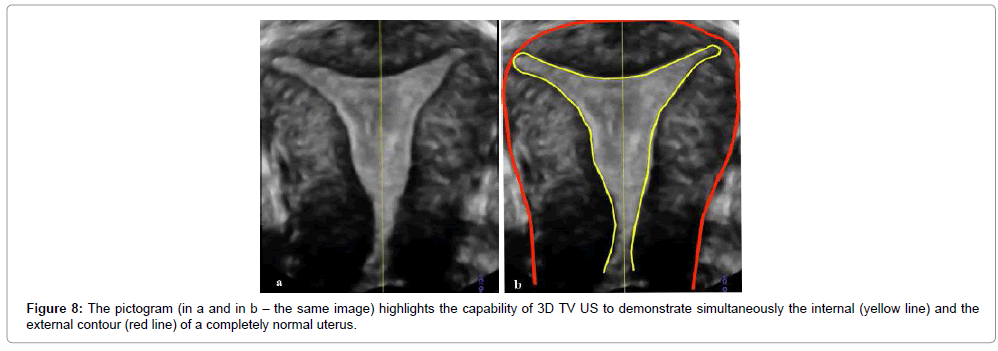
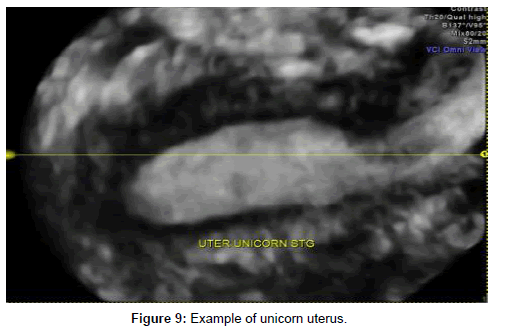
Allows the visualization of the coronal plane of the uterus, critically important for the congenital uterine anomalies diagnosis, and impossible to achieve in 2D US (Figures 8 and 9).
Is accurate and reliable, providing exceptionally clear high resolution frontal view of the uterus and its anatomical details, including details on the uterine walls, the assessment the relationship between endometrium and myometrium of the uterine fundus and depicts cornual angles, offers the accurate simultaneous assessment of both internal and external contour of the uterus. Is non-invasive (thus extremely well tolerated), Have no side-effects, so it is repeatable, is cost-effective, is simple, and the learning curve is abrupt and short, due to higher resolution and convenience of the systems used in daily practice. Offers fast results (as the matter of fact instant results), is objective (offers measurable and reproducible measurement of different features) Carries no anaesthetic or surgical risks, Implies no ionizing radiation, it is an outpatient (office) procedure, Images are not affected by bowel peristalsis. Has a continuously wider availability worldwide.
Allows storage of volume data (useful in retrospective analysis, network consultation and exchange of the data, interactive review at any time without presence of the patient, reduction of the imaging time);
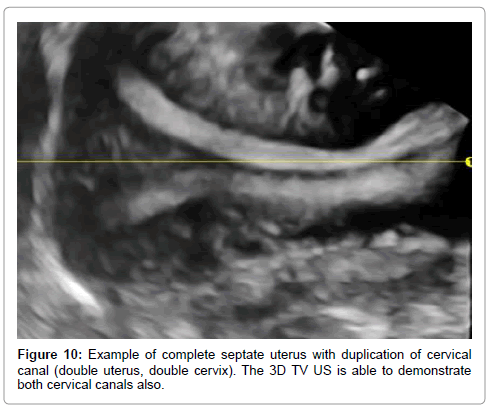
Has the characteristic of multiplanar capability, rotation and magnification, enabling an unlimited number of scan planes for detailed exploration of the uterine cavity; Delineates the entire cervical canal (Figure 10).
The reasons mentioned above upgrade the 3D TV US to the ideal diagnostic modality, the basic imaging method, to asses in detail the complete uterine morphology.
3D TV US has very few disadvantages: the operator-dependency (common in every imagistic technique) and the rare situation of complete transversal vaginal septa, in which it is impossible to be performed.
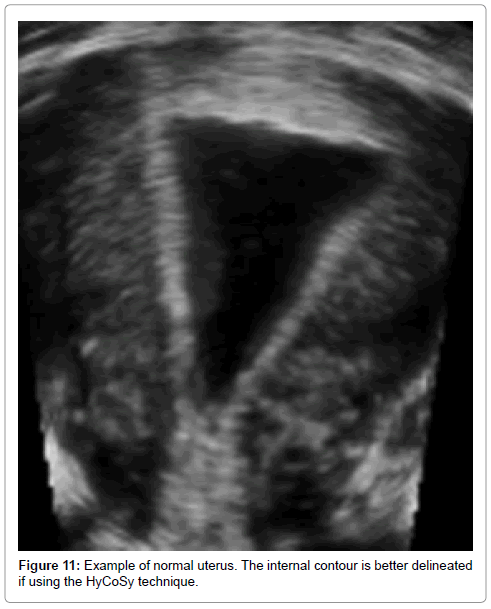
Enhancing the amount of information with sonohisterography (SHG) and ambulatory mini-HSK is reasonable, since they can provide additional information, especially in cases with associated endometrial focal lesions (Figure 11). Hysterosalpingo-contrast-sonography (shortened to HyCoSy) is a safe and reliable alternative to the conventional HSG, using no radiation or iodinated contrast material, but an agitated saline/air mixture [12]. If a non-iodinated contrast foam agent (called ExEm Foam) is used, the test is referred to as a HyFoSy procedure. These techniques offer information on the tubal patency also.
Magnetic resonance imaging alone
Magnetic resonance imaging (MRI) has been considered by some groups the ideal method to assess congenital mullerian anomalies, having the additional benefit to asses associated anomalies in other systems [29]. Still, from the point of view of a gynaecologist, it carries a number of drawbacks also:
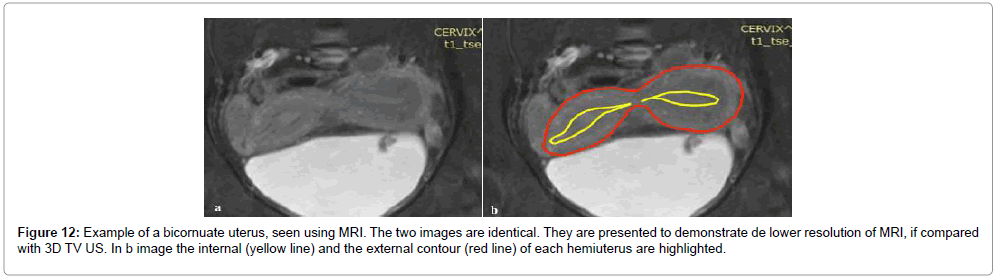
Contrary to the visualization in ultrasound, in MRI, the myometrium is not seen as a homogeneous smooth muscle mass, but is divided into two different structural and functional entities: the internal myometrium or junctional zone (JZ), ontogenetically related to the endometrium and functionally important for reproduction, and the outer myometrium, which is seen as a larger hypodense zone. This difference may influence critically the way that MRI allows classification. It is an expensive method. Has a low availability. Implies an important discomfort for the patient. Has not an adequately proven accuracy (Class III method by Saravelos) [23].
Has a much lower resolution (mainly due to the size of normal uterus and bowels movements) if compared to 3D US (Figure 12). There are different safety regulations in each country. Images are affected by bowel peristalsis. For all these reasons, MRI should be probably kept for research, especially for cases of complex anomalies.
The Diagnostic Methods Classification
Based on their diagnostic accuracy, the diagnostic methods have been categorized, in an exceptionally important paper [23], into four categories:
Class Ia-Those that are capable of identifying mullerian duct anomalies (MDA) and classifying them into appropriate sub-types with an accuracy of >90%: 3DUS; HSK+LSK; SHG.
Class Ib-Those that are capable of identifying MDA with an accuracy of >90% without being able to classify them into appropriate sub-types: HSK alone.
Class II-Those that are capable of identifying MDA with an accuracy of <90%: HSG; 2DUS.
Class III-This includes the investigations whose diagnostic accuracy in identifying MDA still not exactly known: MRI.
Nevertheless, this classification of the methods used will probably suffer changing in the foreseeable future, each method being in the midst of rapid evolution.
Screening (in low risk population) for mullerian anomalies in general should imply an MRI exam, due to associations. This cannot be used as a screening tool. Just the opposite, screening with 3D for uterine corpus anomalies, is easy, cheap, and feasible. This approach should be preferred, because mullerian anomalies that avoid the corpus are extremely rarely seen, and because an impact in obstetrical outcome is expected to be found in this particular subgroup, with corporeal changes in shape and amount of surface available for carrying a full term pergnancy. To highlight the type of corpus distortion that may be encountered in everyday practice, we review below the main congenital uterine anomalies classification systems used nowadays.
Congenital Uterine Anomalies Classification Systems
In recent years, the field of congenital mullerian anomalies has become a “field of battle”, researchers involved in this area being equally passionate and defending many proposed classification systems.
The most heated debates concerned two classification systems: the classic AFS/ASRM (AFS=American Fertility Society, later named ASRM=American Society for Reproductive Medicine) classification system and the much newer proposal from ESHRE/ESGE (ESHRE=European Society of Human Reproduction and Embryology, ESGE=European Society of Gynaecological Endoscopy).
Classification systems are extremely useful and necessary for organizing any kind of knowledge, especially medical knowledge. In medicine, categorization enables a better understanding of disease processes, as well as more effective diagnosis and treatment. The acceptance of a system indicates its ability to effectively correspond to the needs of the clinicians in understanding, diagnosing, and treating patients.
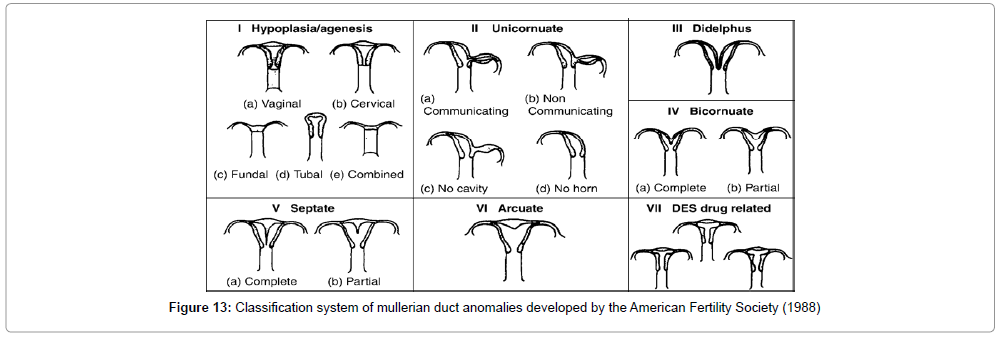
The AFS (American Fertility Society) (1998), based on the previous work of Buttram and Gibbons (1979), classified the anomalies of the female reproductive tract into groups according to the degree of failure of normal development with similar clinical manifestations, treatment, and possible prognoses for their reproductive performance [30]. The various Mu╠?llerian anomalies are the consequence of four major disturbances in the development of the female genital system during fetal life:
1. Failure of one or more Mu╠?llerian ducts to develop (agenesis, unicornuate uterus without rudimentary horn);
2. Failure of the ducts to canalize (unicornuate uterus with rudimentary horn without proper cavities);
3. Failure to fuse or abnormal fusion of the ducts (uterus didelphys, bicornuate uterus);
4. Failure of resorption of the midline uterine septum (septate uterus, arcuate uterus).
Hereby we present the well-known AFS classification system, used worldwide since its publication (Figure 13).
The main drawback of the AFS classification system is that it does not specify either morphological features or diagnostic methods to describe the uterine morphology. All reports using it are based on the subjective assessment of the operators.
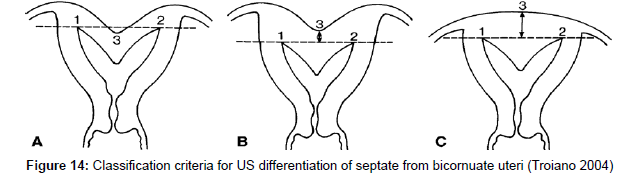
Due to the numerous debates on the differentiation of septate from bicornuate uteri, in 2004, Troiano and his team published a new 3D US based method, with the purpose to help this delineation [31]. It is not yet widely used, and has not yet been clinically validated (Figure 14).
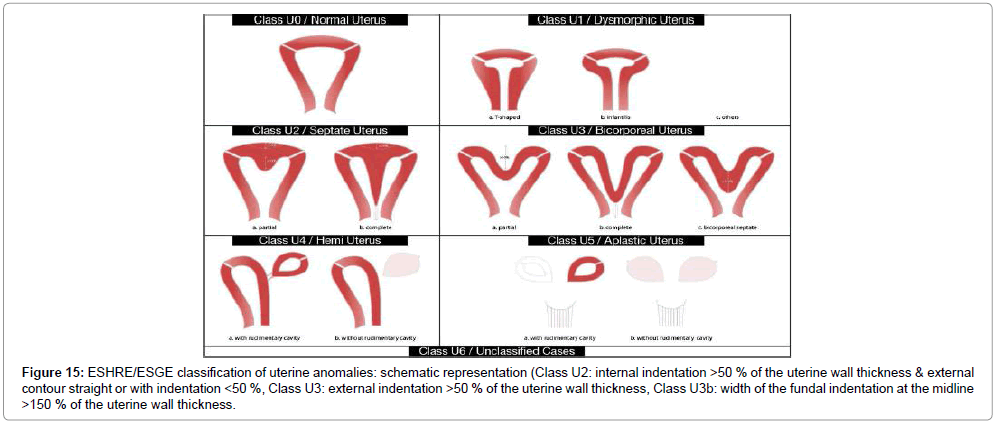
Below we present the new ESHRE/ESGE classification system, published in 2013 (Figure 15) [32].
Figure 15: ESHRE/ESGE classification of uterine anomalies: schematic representation (Class U2: internal indentation >50 % of the uterine wall thickness & external contour straight or with indentation <50 %, Class U3: external indentation >50 % of the uterine wall thickness, Class U3b: width of the fundal indentation at the midline >150 % of the uterine wall thickness.
The ESHRE/ESGE classification system claims many advantages over the old AFS one [32-35]:
It is based on a high number of experts and their opinion. It is based on anatomy. It has mainly clinical orientation. May be the starting point for the development of guidelines for diagnosis and treatment.
Cervical and vaginal anomalies are classified independently into sub-classes.
Anomalies are sorted in the classes and subclasses according to increasing severity [32-37].
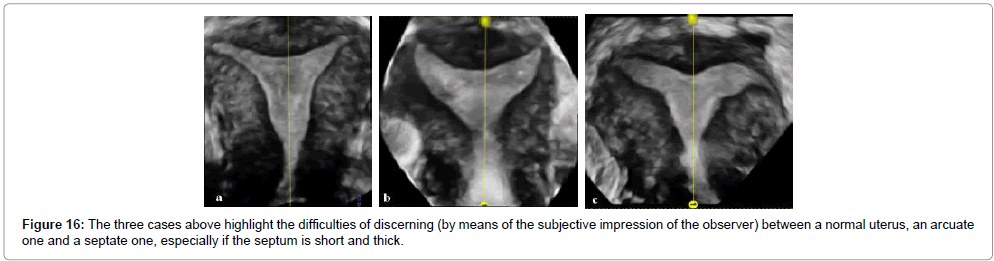
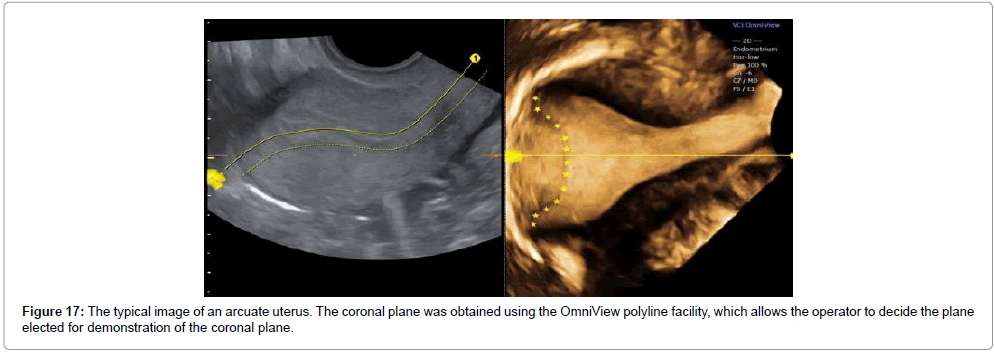
Still, its clinical value is questioned [33-44], it needs to be proved in everyday practice, and it has not yet gained validation and generalization. The absence of arcuate uterus from the new classification system has been repeatedly commented; some groups supported the notion that even very small deformities of the uterine cavity (arcuate uterus) could be associated with poor pregnancy outcome. However, it was pointed out by the ESHRE/ESGE group that until now the term arcuate was quite confusing, and it included patients with different degrees of uterine deformity, even partial septa, since its definition is not clear at all (Figures 16 and 17). The group highlights the necessity to have clear definitions, based on the experience gained from the application of the AFS system.
Differentiation between arcuate and septate uteri was traditionally carried out in the coronal plane. While both types of uterus have a normal contour, in arcuate uterus the fundal indentation appears as an obtuse angle at the central point, with a depth of up to 1.5 cm, whereas septate uterus is characterized by a fundal indentation with an acute angle at the central point, with a depth of 1.5 cm or more [35].
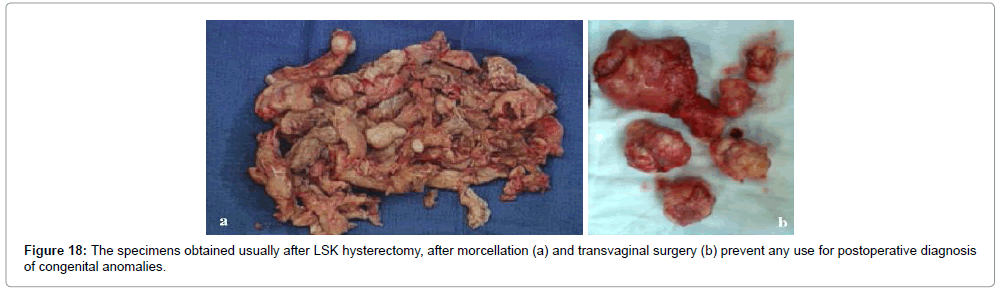
Why a Conventional Accuracy Study is Impossible
The most important problem of accuracy studies is that there is no true “gold standard test”. Because such a test would be assessing the uterus itself, all others (including the MRI) have many limitations. Having the specimen itself is impossible, and, when possible, the uterus is usually severely distorted, by intrinsic diseases and/or the surgery intervention itself (especially nowadays, with the advances of minimal surgery techniques) (Figure 18).
Thus, trying to screen is particularly challenging.
Why should Use 3D TV US in Screening for Congenital Uterine Anomalies in Unselected Population
Although using 3D in assessing the uterus has been advocated since many years now, many asymptomatic congenital uterine anomalies remain undiagnosed. Investigations such as HSG, HSK and LSK would not be warranted in women without a particular indication. Nor in women either undergoing sterilization or being investigated for non-obstetric reasons such as pelvic pain, ovarian cancer screening, abnormal bleeding and suspected fibroids/polyps. Until recently, 3D US have been used in selected cases, mainly in fertility centers and in case series with obstetrical unfavourable outcome (sterile, infertile and subfertile women). Many research groups have reported 3D accuracy compared to the established, well-known methods. Yet, in our view, we should do the other way around: to consider 3DUS the gold standard method, ideal for routine screening and diagnosis, and to report accuracy rates for all traditional invasive methods (HSK, HSG, LSK) against it, and using it as a gold standard.
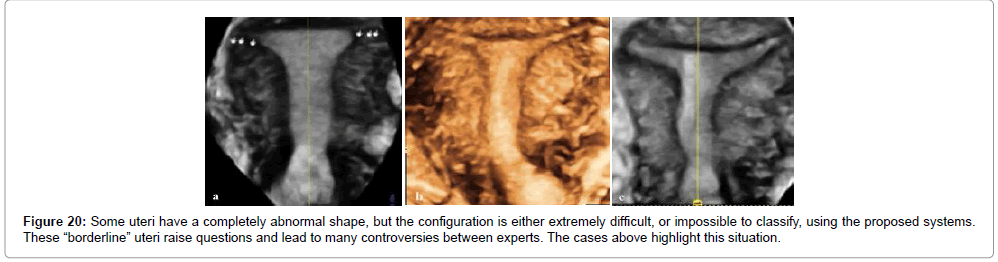
A screening policy with 3DUD TV, the ideal method in many aspects, for congenital uterine anomalies would be a difficult prospective research. In the authors’ view it will eventually be part of routine clinical investigations of women presenting for routine gynecology visits in the foreseeable future. Still, a huge amount of research must be done, to homogenize the technique for performing the scan and the measurements, in order to clarify the true incidence of uterine anomalies (in low and high risk, symptomatic and asymptomatic women) and thus, to be able to clarify the clinical significance (especially in “borderline” uterus). The current definitions for uterine morphology are still controversial, which is an important barrier for studies evaluating the true clinical significance and also the effectiveness of interventions for women with such conditions.
Quantitative description of uterine morphology, by far best achieved in 3D TV US, may show that not only the type of uterine anomaly, but also its severity, may be important in assessing the risk of adverse pregnancy outcomes. This could help to refine the classification in major/minor anomalies, the selection criteria for surgery, resulting the true impact of congenital uterine anomalies on reproductive outcomes (which is unknown), and hopefully, in improved long-term outcomes in women with uterine anomalies.
In order to achieve this objective, a relatively large amount of data needs to be collected. Bearing in mind the rarity of uterine anomalies, this can only be achieved by establishing a wide international collaboration involving a large number of research centers. 3D ultrasound is the only diagnostic method available to facilitate such collaboration. By submitting the archived 3D volumes, both operator dependence and subjective bias in the assessment of uterine morphology would be almost completely eliminated. Until such a study has been conducted, we have to face uncertainty about the clinical significance and optimal management of congenital uterine anomalies [4,45].
The potential significance of uterine anomalies in the context of recurrent pregnancy loss cannot be established without comparisons with the low risk population, because all published reports have studied different populations, different or non-standardized classification systems, having many differences in diagnostic data acquisition and being characterized by an extremely difficult to avoid, almost mandatory, selection bias.
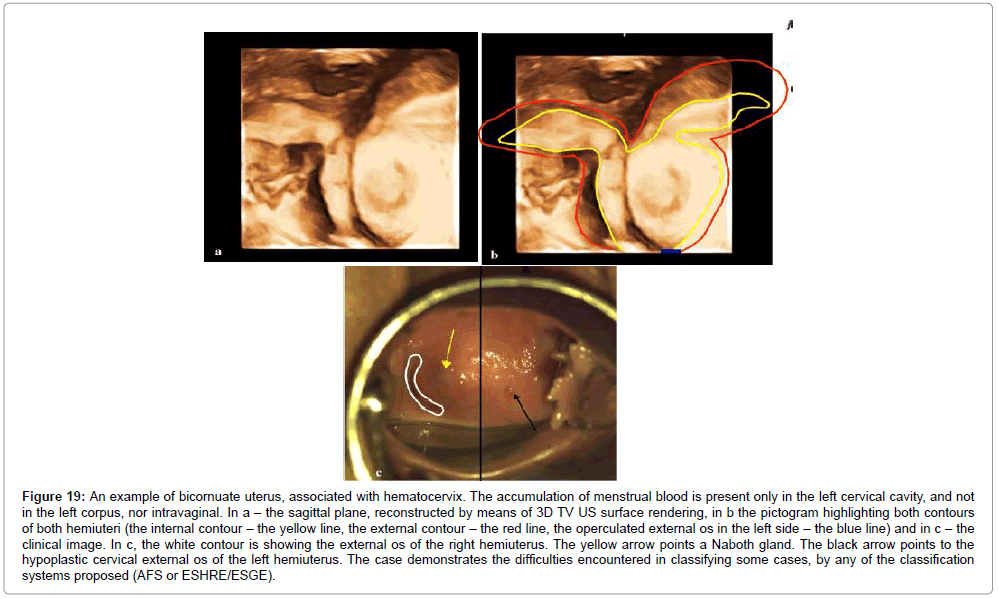
Very few studies published so far have included a formal assessment of diagnostic reproducibility [45]. There is no agreement on the criteria to diagnose different types of anomalies in 3D. The need to address this issue is clearly illustrated by the large variation in the prevalence of uterine anomalies between different studies using three-dimensional ultrasound [4,16-18,27,30,45]. These differences cannot be explained by the variations in study populations and it is almost certain that the researchers used different criteria to diagnose a uterine septum (Figure 19). Standardization leads to a less operator-dependency of the technique, and this is the reason why we all should aim for standardization of uterus examination also. In a screening policy there won’t be any sampling bias, since 3D-US would be performed in all consecutive cases, not only on those patients whose 2D-US findings suggested the presence of a uterine malformation or on those patients with associated morbidity (Figure 20). The association of clinical exam, 3D TV US, SHG and office HSK may became the gold-standard investigation of the female genitalia. This approach would obviate for sure the need for diagnostic laparoscopy to assess the fundal indentation, making invasive procedures (such as HSK and LSK) beneficial, but in conjunction with therapeutic procedures only. Even in developing countries like Romania 3D TV US seems to be already a technically feasible and commercially available diagnostic procedure. Judging by published literature, 3 TV US has achieved a recognized diagnostic role that goes much beyond the conventional 2D US and thus deserves to be included in routine practice. Health care providers should be informed about the established, increasing role being played by 3D US in gynecology practice and should be confident about administering 3D US examination to their patients. Health authorities are being required to make significant investments in advanced technology and to appropriately equip and digitalize modern obstetrics ultrasound laboratories.
Figure 19: An example of bicornuate uterus, associated with hematocervix. The accumulation of menstrual blood is present only in the left cervical cavity, and not in the left corpus, nor intravaginal. In a – the sagittal plane, reconstructed by means of 3D TV US surface rendering, in b the pictogram highlighting both contours of both hemiuteri (the internal contour – the yellow line, the external contour – the red line, the operculated external os in the left side – the blue line) and in c – the clinical image. In c, the white contour is showing the external os of the right hemiuterus. The yellow arrow points a Naboth gland. The black arrow points to the hypoplastic cervical external os of the left hemiuterus. The case demonstrates the difficulties encountered in classifying some cases, by any of the classification systems proposed (AFS or ESHRE/ESGE).
Conclusion and Future Direction Research
In obstetrics 3D US did not fundamentally change the way in which ultrasound examination is performed; neither did cause a revolution in ultrasound diagnosis.
In congenital mullerian anomalies 3D is critical in reaching the correct diagnosis. This is the area where the greatest diagnostic improvements did occur.
We should elaborate standard “volumetric criteria” for the diagnosis of female genital anomalies, thus using the 3DUS only. Clearly defined diagnostic criteria is required in order to examine the reproducibility of US diagnosis, because we still face the lack of agreement in regards to diagnostic standards. Otherwise there is a high risk of significant interobserver variability in the diagnosis of uterine anomalies [24,26,45].
There is very limited information on the reproductive risks associated with an incidental diagnosis of congenital uterine anomaly, and many asymptomatic cases, and these are the main reasons for screening.
There is also no evidence that surgical correction of an incidentally diagnosed uterine anomaly is helpful [46,47]. This direction merits all efforts. 3 DUS represents, in our view, the most major development in ultrasound imaging, providing a unique, very different way of displaying ultrasound data in gynecology. Thus, the option of 3D TV imaging should be integrated in all US machines, and large prospective multinational studies should be carried out.
Acknowledgement
The authors would like to thank the University Hospital researchers for their contribution in collecting the data, and the patients involved for their permission to publish their images.
References
- Jurkovic D, Geipel A, Gruboeck K, Jauniaux E, Natucci M, et al. (1995) Three-dimensional ultrasound for the assessment of uterine anatomy and detection of congenital anomalies: a comparison with hysterosalpingography and two-dimensional sonography. Ultrasound Obstet Gynecol 5: 233-237.
- Green LK, Harris RE (1976) Uterine anomalies. Frequency of diagnosis and associated obstetric complications. Obstet Gynecol 47:427-429.
- Heinonen PK, Saarikoski S, Pystynen P (1982) Reproductive performance of women with uterine anomalies. An evaluation of 182 cases. Acta Obstet Gynecol Scand 61:157-162.
- Golan A, Langer R, Bukovsky I, Caspi E (1989) Congenital anomalies of the müllerian system. Fertil Steril 51:747-755.
- Golan A, Barnan R, Wexler S, Langer R, Bukovsky I, et al. (1989) Incompetence of the uterine cervix. Obstet Gynecol Surv 44:96-107.
- Simón C, Martinez L, Pardo F, Tortajada M, Pellicer A (1991) Müllerian defects in women with normal reproductive outcome. Fertil Steril 56:1192-1193.
- Kupesic S (2001) Clinical implications of sonographic detection of uterine anomalies for reproductive outcome. Ultrasound Obstet Gynecol 18: 387-400.
- Soares SR, Reis MMBD, Camargos AF (2000) Diagnostic accuracy of sonohysterography, transvaginal sonography, and hysterosalpingography in patients with uterine cavity diseases. Fertil Steril 73:406-411.
- Reuter KL, Daly DC, Cohen SM (1989) Septate versus bicornuate uteri: errors in imaging diagnosis. Radiology 172: 749-752.
- Golan A, Ron-El R, Herman A, Soffer Y, Bukovsky I, et al. (1992) Diagnostic hysteroscopy: its value in an in vitro fertilisation/embryo transfer unit. Hum Reprod 7: 1433-1434.
- Karande VC, Pratt DE, Balin MS, Levrant SG, Morris RS, et al. (1997) What is the radiation exposure to patients during a gynecoradiologic procedure? Fertil Steril 67:401-403.
- Ayida G, Kennedy S, Barlow D, Chamberlain P (1996) A comparison of patient tolerance of hysterosalpingo-contrast sonography (HyCoSy) with Echovist-200 and X-ray hysterosalpingography for outpatient investigation of infertile women.Ultrasound Obstet Gynecol 7:201-204.
- Forsey JP, Caul EO, Paul ID, Hull MG (1990) Chlamydia trachomatis, tubal disease and the incidence of symptomatic and asymptomatic infection following hysterosalpingography. Hum Reprod 5: 444-447.
- Belt MM, Rodenko G, Taylor K, Maguire C, Bello S (2008) Use of gadolinium for hysterosalpingography in iodine allergic women: a case-control study. Fertil Steril 90:835-838.
- Maheux-Lacroix S, Boutin A, Moore L, Bergeron ME, Bujold E, et al. (2014) Hysterosalpingosonography for diagnosing tubal occlusion in subfertile women: a systematic review with meta-analysis. Hum Reprod29:953-963.
- Chan YY, Jayaprakasan K, Tan A, Thornton JG, Coomarasamy A, et al. (2011) Reproductive outcomes in women with congenital uterine anomalies: a systematic review. Ultra Obste Gynecol38: 371-382
- Nick Raine-Fenning, Arthur C Fleischer (2005) Clarifying the role of three-dimensional transvaginal sonography in reproductive medicine: an evidenced-based appraisal. J Exper Clin Assisted Reprod 2: 10.
- YY Chan, K Jayaprakasan, J Zamora, JG Thornton, N Raine-Fenning, et al. (2011) The prevalence of congenital uterine anomalies in unselected and high-risk populations: a systematic review. Human Reproduction Update 17: 761-771.
- K Jayaprakasan, YY Chan, S Sur, S Deb, JS Clewes, N Raine-Fenning(2011) Prevalence of uterine anomalies and their impact on early pregnancy in women conceiving after assisted reproduction treatment.Ultras Obste Gynecol37: 727-732.
- Birmingham, Alabama (2012) Evaluation and treatment of recurrent pregnancy loss: a committee opinion. Fertility and Sterility 98: 1103-1111.
- Eberhard Merz (1999) Three-dimensional transvaginal ultrasound in gynecological diagnosis, Ultr Obste Gynec 14: 81-86.
- Abuhamad AZ, Singleton S, Zhao Y, Bocca S (2005) The Z Technique: An Easy Approach to the Display of the Midcoronal Plane of the Uterus in Volume Sonography. J Ultras Med25: 607-612.
- Saravelos SH, Cocksedge AK, Li TC(2008) Prevalence and diagnosis of congenital uterine anomalies in women with reproductive failure: a critical appraisal. Human Reproduction Update14: 415-429.
- Ghi T, Casadio P, Kuleva M, Perrone AM, Savelli L, et al. (2009) Accuracy of three-dimensional ultrasound in diagnosis and classification of congenital uterine anomalies. Fertility and Sterility92: 808-813.
- Homer HA, Li TC, CookeID (2000) The septate uterus: a review of management and reproductive outcome. Fertility and Sterility73: 1-14.
- Salim R, Woelfer B, Backos M, Regan L, Jurkovic D (2003) Reproducibility of three-dimensional ultrasound diagnosis of congenital uterine anomalies. Ultras Obste Gyneco21: 578-582.
- Woelfer B, Salim R, Banerjee S, Elson J, Regan L, et al. (2001) Reproductive Outcomes in Women With Congenital Uterine Anomalies Detected by Three-Dimensional Ultrasound Screening.Obsteand Gyne98: 1099-1103.
- Raga F, Bauset C, Remohi J, Bonilla-Musoles F, Simón C, et al. (1997) Reproductive impact of congenital Müllerian anomalies. Hum Reprod12:2277-2281.
- Bermejo C, Martínez TP, Cantarero R, Diaz D, Pérez Pedregosa J, et al. (2010) Three-dimensional ultrasound in the diagnosis of Müllerian duct anomalies and concordance with magnetic resonance imaging. Ultrasound Obstet Gynecol 35:593-601.
- Birmingham, Alabama (1988) The American Fertility Society classifications of adnexal adhesions, distal tubal occlusion, tubal occlusion secondary to tubal ligation, tubal pregnancies, mullerian anomalies and intrauterine adhesions. Fertil Steril 49: 944-955.
- Troiano RN, McCarthy SM (2004) Mullerian duct anomalies: imaging and clinical issues. Radiology233: 19-34.
- Grimbizis GF, Gordts S, Sardo ADS, Brucker S, De Angelis C, et al. (2013) The ESHRE/ESGE consensus on the classification of female genital tract congenital anomalies. Human Reproduction28: 2032-2044.
- Grimbizis GF, Sardo ADS, Saravelos SH, Gordts S, Exacoustos C, et al. (2016) The Thessaloniki ESHRE/ESGE consensus on diagnosis of female genital anomalies. J Gyneco Sur31: 1-16.
- Grimbizis GF, Gordts S, Sardo ADS, Brucker SY, Angelis CD, et al. (2014) Reply: Are the ESHRE/ESGE criteria of female genital anomalies for diagnosis of septate uterus appropriate? Human Reproduction pp: 1-2.
- Grimbizis GF, Campo R, (2010) Congenital malformations of the female genital tract: the need for a new classification system. Fertility and Sterility 94: 401-407.
- Sardo ADS, Campo R, Gordts S, Spinelli M, Cosimato C(2015) The comprehensiveness of the ESHRE/ESGE classification of female genital tract congenital anomalies: a systematic review of cases not classified by the AFS system. Human Reproduction 30: 1046-1058.
- Graupera B, Pascual MA, Rodríguez I (2015) Reply, Ultrasound in Obstetrics and Gynecology46: 633-637.
- Ludwin A, Ludwin I, Pityn K, Banas T, Jach R (2014) Role of morphologic characteristics of the uterine septum in the prediction and prevention of abnormal healing outcomes after hysteroscopic metroplasty. Human Reproduction29:1420-1431
- Ludwin A, Ludwin I, Kudla M, Pitynski K, Banas T, et al. (2014) Diagnostic accuracy of three-dimensional sonohysterography compared with office hysteroscopy and its interrater/intrarater agreement in uterine cavity assessment after hysteroscopic metroplasty. Fertility and Sterility101: 1392-1399.
- Ludwin A, Ludwin I (2015) Correspondence - Diagnostic rate and accuracy of the ESHRE–ESGE classification for septate uterus and other common uterine malformations: why do we not see that the Emperor is naked? Ultrasound in Obstetrics and Gynecology 46: 634-636.
- Ludwin A, Ludwin I (2015) Comparison of the ESHRE–ESGE and ASRM classifications of Müllerian duct anomalies in everyday practice”. Human Reproduction 30: 569-580.
- Ludwin A, Ludwin I, Pity┼?ski K, Jach R, Banas T (2014) Are the ESHRE/ESGE criteria of female genital anomalies for diagnosis of septate uterus appropriate? Human Reproduction 29: 867-869.
- Grimbizis GF, Camus M, Tarlatzis BC, Bontis JN, Devroey P (2001) Clinical implications of uterine malformations and hysteroscopic treatment results. Human Reproduction Update 7: 161-174.
- Graupera B, Pascual MA, Hereter L, Browne JL, Ubeda B (2015) Accuracy of three-dimensional ultrasound compared with magnetic resonance imaging in diagnosis of Müllerian duct anomalies using ESHRE–ESGE consensus on the classification of congenital anomalies of the female genital tract. Ultras Obstetr Gyneco 46: 616-622.
- Neto MAC, Roncato P, Nastri CO, Martins WP (2015) True Reproducibility of UltraSound Techniques (TRUST): systematic review of reliability studies in obstetrics and gynecology. Ultras Obstet Gynec46: 14-20.
- Prior M, Raine-Fenning N (2014) Response to: Hysteroscopic metroplasty: reproductive outcome in relation to septum sizem by Paradisi et al. Archives of Gyneco Obste 290: 2.
- Paradisi R, Barzanti R, Natali F, Guerrini M, Battaglia C, et al. (2014) Hysteroscopic metroplasty: reproductive outcome in relation to septum size. Archives of Gynecology and Obstetrics 289: 671-676.
Relevant Topics
- Back Pain Diagnosis
- Cardiovascular Diagnosis
- Clinical Diagnosis
- Clinical Echocardiography
- COPD Diagnosis
- Diabetes Diagnosis
- Diagnosis Methods
- Diagnosis of cancer
- Diagnosis of CNS
- Diagnosis of Diabetes
- Diagnostic Products
- Diagnostics Market Analysis
- Heart diagnosis
- Immuno Diagnosis
- Infertility Diagnosis
- Medical Diagnostic Tools
- Preimplementation Genetic Diagnosis
- Prenatal Diagnostics
- Ultrasonography
Recommended Journals
Article Tools
Article Usage
- Total views: 15381
- [From(publication date):
June-2017 - Dec 03, 2024] - Breakdown by view type
- HTML page views : 14297
- PDF downloads : 1084