10 Years Follow-Up after Bariatric Surgery: Body Composition, Weight and Diabetes
Received: 28-Oct-2020 / Accepted Date: 10-Nov-2020 / Published Date: 17-Nov-2020 DOI: 10.4172/2165-7904.1000416
Abstract
Introduction: Obese patients have better glycemic control and/or Type 2 diabetes mellitus (T2DM) remission after bariatric surgery.
Objectives: To evaluate body composition in obese patients after Roux-en-Y Gastric Bypass surgery (RYGB).
Methods: Anthropometric measurements, subcutaneous adipose tissue (SAT) and muscle thickness of both thighs were determined, 30, 60, 90 and 180 days after surgery (N:19) and ten years after RYGB (N:7). During these periods, patients were evaluated by ultrasound in transverse plane to determine the thickness of SAT and muscle of the lower limbs.
Results: They were 6 female and 1 male with 51(±6.0years) of age. Six of them had initially T2DM, with remission after surgery. The baseline Body Mass Index was 43(±8.0kg/m2), and after 10 years of RYGB was 31(±5.5kg/m2). The right and left muscle thickness in baseline were, respectively, 3.0(±0.6 cm) and 3.0(±0.6 cm), after 10 years were 2.1(±0.6 cm) and 2.0(±0,6 cm).The right and left SAT thickness were, respectively, 2.0(±0.5 cm) and 1.6(±0.6 cm), at baseline and after 10 years 0.9(±0.5cm) and 0,5(±0.2 cm).The reduction of muscle and SAT thickness and weight 10 years after RYGB was significant compared to the baseline.
Conclusion: After 10 years of RYGB, we found maintenance of weight loss, reduction of muscle and fat thickness and remission of T2DM.
Keywords: Fat mass, Muscle, Ultrasound, Obesity, Body composition
Introduction
Bariatric surgery for grade III obesity is considered the most effective method of achieving significant weight loss and maintaining a reduced weight over time [1,2]. In general, at 12 months, changes in weight are greater in the gastric bypass than in the clinical treatment [3]. In addition, grade I-II obese patients after bariatric surgery usually show better glycemic control or even Type 2 diabetes mellitus (T2DM) remission [4-6].
Moreover, in addition to loss of fat mass after bariatric surgery, there is a degree of skeletal muscle loss that also occurs, approximately 31%, raising the possibility of a negative effect on muscle strength, quality of life and physical performance. Fatigue and functional impairment also occur [2,7-11]. Besides that, muscle is involved in post-prandial glucose disposal and is a major determinant of insulin sensitivity [11]. For this reason, after bariatric surgery, it is important to evaluate, besides the amount of weight loss, changes in body composition. This can be estimated through ultrasound (US) measurements of muscle and fat thickness in the thighs. It is a practical, high cost-benefit, safe, reproducible, accurate and validate method for fat and muscle evaluation in obese and bariatric surgery patients [2,12].
Thus, the primary aim of the present study was to describe muscle and fat mass thickness of right and left thigh changes after 30 days, 90 days, 180 days and 10 years after Roux-en-Y gastric bypass surgery.
Methods
Patients
In 2008, we evaluated 19 patients (10 diabetic and 9 nondiabetic) undergone RYGB, Obesity and Bariatric Surgery Division, Universidade Federal de Sao Paulo (UNIFESP), São Paulo, Brazil. In 2018, only 7 could be recruited for revaluation. The Ethic Committee at the UNIFESP approved this study, and all participants signed an informed consent agreement.
Anthropometric measurements, Glucoses serum levels (GSL) and Glycated hemoglobin (A1C)
In order to determine the height (m), a stadiometer (with total height of 2.0 m and precision of 1.0 mm) was used, duly posted on the wall, with the patient standing, barefoot, with their heels together, with the back straight and arms outstretched at the sides of the body. The measurement of weight (kg) was performed by a properly calibrated scale, with the patient standing in the center of the scale base, barefoot and wearing light clothing.
Body mass index (BMI) calculated as weight (kg) divided by the squared height (m) [13,14]. BMI was used to classify nutritional status of the adult patients as [13]: < 16 kg/m2: malnutrition grade III; 16 – 16,9 kg/m2: malnutrition grade II; 17 – 18,4 kg/m2: malnutrition grade I; 18,5 – 24,9 kg/m2: normal; 25 – 29,9 kg/m2: overweight;30 – 34,9 kg/m2: obesity grade I; 35 – 39,9 kg/m2: obesity grade II; ≥ 40 kg/m2: obesity grade III.
All patients had GSL and A1C measured before and after surgery. GSL was determined by the glucose oxidase method and A1C was determined by high-performance liquid chromatography (HPLC) [15]. All diabetes medications were discontinued after surgery.
Quadriceps muscle and subcutaneous adipose tissue thickness
All participants were examined by ultrasound Philips® Envisor CHD ultrasound machine, using the 5.0-MHz linear transducer. The right and left quadriceps femoris, subcutaneous adipose tissue (SAT) and muscle thickness were the sites chosen for re-evaluation. The site was evaluated by a single experienced physician examiner, the same at 10 years before, who obtained the mean of three ultrasound measurements performed in the same place in both the transverse planes [2].
The subject rested in supine position prone and relaxed, with arms and legs fully extended during the measurements. To standardize the measurements, the probe was held perpendicular to the corresponding bone. Water-soluble transmission gel provided acoustic contact without depression of the skin surface while the probe was placed perpendicular to the tissue interface under the marked sites [2].
For ultrasound measurements, the probe was placed at the position of maximum circumference.The thickness of subcutaneous adipose tissue was measured by the distance between the skin and muscle fascia (cm). And the thickness of muscles was measured by the distance between the muscle fascia and underlying bones (femur) (cm). These measurements were performed 15 cm from the superior pole of the patella on the quadriceps muscle in the ventral, mid-line of the thigh [2].
Data analysis
Statistical analysis was performed using Statistical Package for Social Sciences (SPSS) version 22.0 (SPSS Inc., Chicago, IL, USA). Friedman’s statistical test was used to evaluate all comparisons of preoperative and postoperative ultrasound and anthropometric measurements. Pearson’s statistical test was used to correlate ultrasound measurements and age.
Data are expressed as the mean ± standard deviation (SD), and p <0.01 and p <0.05 were considered statistically significant.
Results
We evaluated 6 female and 1 male patient that corresponded 42% of previous sample in 2008. They were 51 (±6.0 years) in 2018 and 6 who were diabetics in 2008 showed complete remission after 10 years of surgery.GSL was evaluated before surgery and after 10 years, respectively, 119(±40 mg/dL) and 79(±9.4 mg/dL) and A1C respectively, 7.0(±2.0%) and 5.3(±0.5%).GSL (p=0.000) and A1C (p=0.046) were significantly different after 10 years related to baseline.
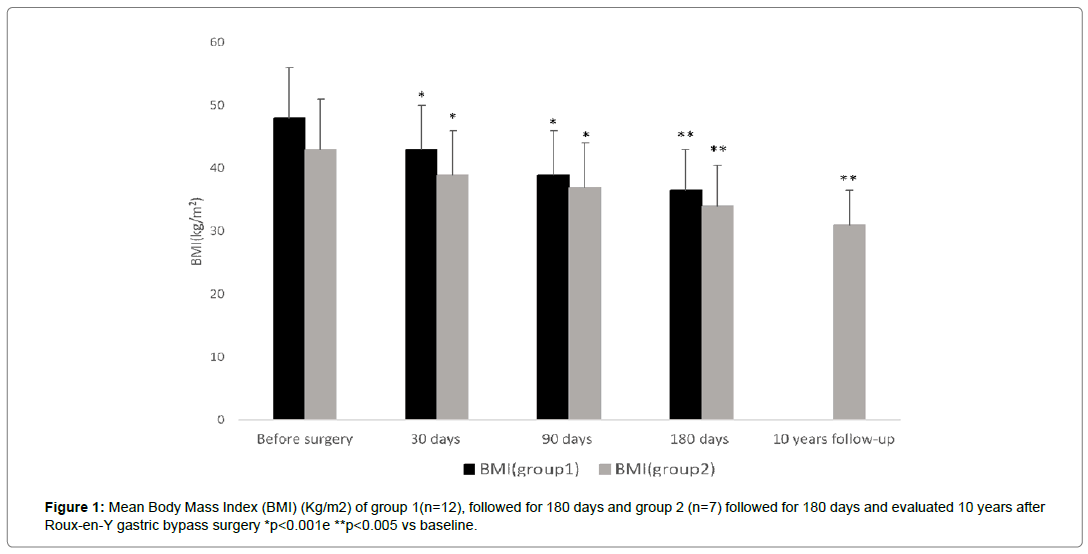
Considering 10 years follow up patients (N=7)(group1), the baseline weight and BMI were, respectively, before surgery 114 (±21kg) and 43(±8.0kg/m2), and after 10 years of RYGB were 83(±18 kg) and 31(±5.5kg/m2). (Figure 1)We evaluated 12 patients(group2), who did not answer our call, the baseline weight and BMI were, respectively, before surgery 122(±28kg) and 48(±10.0kg/m2), and after 180 days of RYGB were 92(±20 kg) and 36(±8.0kg/m2). These anthropometric measurements were not significantly different in these 2 groups.
The Excess Weight Loss (EWL) after 180 days and 10 years were, respectively, 54((±16.0%) and 44(±11.0%), therefore 100% of our patients did not have weight regain in this period.
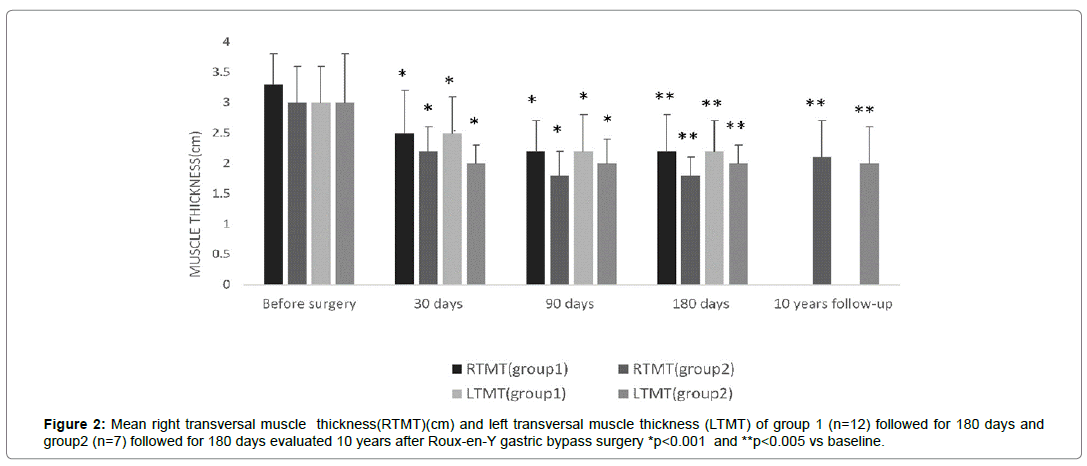
Considering group 1, the right and left muscle thickness in baseline were, respectively, 3.0 (±0.6 cm) and 3.0(±0.6 cm), after 10 years were 2.1(±0.6 cm) and 2.0 (±0,6 cm) (Table 1). In group2 the baseline right and left thickness were, respectively, 3.3(±0.5 cm) and 3.0(±0.6 cm), and after 180 days of RYGB were, respectively, 2.2(±0.6 cm) and 2.2(±0.5 cm) (Figure 2). We did not find any difference between neither right nor left muscle thickness in both groups.
The right and left SAT thickness were, respectively, 2.0(±0.5 cm) and 1.6(±0.6 cm), at baseline and after 10 years 0.9(±0.5cm) and 0,5(±0.2 cm).We evaluated 12 patients, who did not answer our call, either (Table 1).
| TIME | RTMT±SD(cm) | LTMT±SD(cm) | RTFT±SD(cm) | LTFT±SD(cm) |
|---|---|---|---|---|
| Before surgery(N=19) | 3.1 ± 0.6 | 3.0 ± 0.7 | 2.0 ± 0.5 | 2.0 ± 0.7 |
| 30 days(N=19) | 2.4 ± 0.7* | 2.3 ± 0.5* | 2.0 ± 0.7 | 2.0 ± 0.7 |
| 90 days(N=19) | 2.0 ± 0.5* | 2.2 ± 0.5* | 1.6 ± 0.6 | 1.6 ± 0.6 |
| 180 days(N=19) | 2.1 ± 0.5* | 2.1 ± 0.45* | 1.3 ± 0.6* | 1.3 ± 0.7** |
| 10 years follow up(N=07) | 2.1 ± 0.6* | 2.0 ± 0.6* | 1.1 ± 0.6* | 0.5 ± 0.2** |
Table 1: Mean ± standard deviation of muscle and fat thigh thickness evaluated by ultrasound before and after bariatric surgery.
The reduction of muscle and SAT thickness and weight 10 years after bariatric surgery was significant compared to the baseline. However, in relation to 180 days after surgery were not significant after 10 years. There was a positive but not significant correlation between right and left muscle thickness and weight, respectively (rp=0,6 and 0,5). There was not this correlation between right and left SAT thickness and weight. We did not find a correlation between age and muscle thickness after 10 years.
Discussion
This study describes muscle and SAT thickness, weight, BMI and diabetic condition change across 10 years after bariatric surgery. Reduction of weight, BMI and, muscle and SAT thickness remained significant after 10 years follow-up. Besides that, in clinical practice we observed maintenance of diabetic remission and weight loss in this period.
US has lower cost, higher spatial resolution, real-time evaluation, ability to compare to the contralateral site, and it is also a non-invasive, portable, safe and easy to use imaging method [2,16-18]. Although it is reproducible, accurate and validate method for obese and bariatric surgery patients, there are few studies to evaluate body composition by US in this area [2,12].
The preservation of muscle mass has been considered a critical factor for the maintenance of long-term weight loss [19]. Our result of muscle loss after bariatric surgery has already been demonstrated in previous studies[1,8,10,11,19]. Our patients had lost muscle mass significantly since the first month after surgery, however there was not a significant difference 180 days and 10 years after surgery. They were ten years older; they had preserved muscle mass and they had sustained weight loss for 10 years. Therefore, considering the fact that muscle plays an important role in weight loss maintenance, our findings came to demonstrated it.
We found a reduction of SAT thickness that has been sustained for ten years. Mizrahi at al demonstrated this reduction evaluated by US in a short period of time after RYGB [12]. Unfortunately, there was not long-term follow-up studies about this issue.
In our study, the US evaluation was performed by one expert radiologist, who made the same evaluation 10 years before.The use of US to measure muscle and SAT thickness US allows direct measure of muscle mass.
In this study, 86 % of our patients had T2DM before RYGB. All of them (100%) have sustained T2DM remission and weight loss for ten years. Studies have demonstrated that patients had T2DM remission until 2 years after RYGB[6,20]. However, after 6 and 10 years of RYGB, respectively 35% and 50% of relapse occurred different from our finding [4,6]. It could be explained to 100% of our patients did not have weight regain after 10 years of RYGB, according to SOS study demonstrated 10-30% of weight loss maintenance it is essential to sustain T2DM remission in this period [6].
Although this study has several strengths, including a validated and practical method to evaluate muscle and SAT thickness with repeated measures extending 10 years after bariatric surgery, there are some limitations. First, our sample is small, even though we evaluated 42% of our patients after 10 years.Second, we did not measure physical activity or protein intake in these participants; both of which could have affected the time course of changes in muscle and fat thickness after surgery. Third, US is an accurate method to evaluate visceral fat, despite the fact that we did not use it.
Conclusion
After 10 years of surgery a significant reduction in quadriceps SAT and muscle thickness, evaluated by US, was observed.
References
- Davidson LE, Yu W, Goodpaster BH, DeLany JP, Widen E, et al. (2018) Fat-free mass and skeletal muscle mass five years after bariatric surgery. Physiol Behav 26: 1130-1136.
- Pereira AZ, Marchini JS, Carneiro G, Arasaki CH, Zanella MT (2012) Lean and fat mass loss in obese patients before and after Roux-en-Y gastric bypass: A new application for ultrasound technique. Obes Surg 22:597-601.
- Schiavon CA, Bersch-Ferreira AC, Santucci EV, Oliveira JD, Torreglosa CR, et al. (2018) Effects of bariatric surgery in obese patients with hypertension the GATEWAY randomized trial (gastric bypass to treat obese patients with steady hypertension). Circulation 137:1132-1142.
- Maggard-Gibbons MA, Maglione M, Livhits M, Ewing B, Maher AR, et al. (2013) Bariatric surgery for weight loss and glycemic control in nonmorbidly obese adults with diabetes a systematic review. JAMA - J Am Med Assoc 309: 2250-2261.
- Koliaki C, Liatis S, Roux CW, Kokkinos A, le Roux CW, et al. (2017) The role of bariatric surgery to treat diabetes: current challenges and perspectives. BMC Endocr Disord 17: 50.
- Sjöström L (2013) Review of the key results from the Swedish Obese Subjects (SOS) trial - a prospective controlled intervention study of bariatric surgery. J Intern Med 273: 219-234.
- Moizé V, Andreu A, RodrÃguez L, Flores L, Ibarzabal A, et al. (2012) Protein intake and lean tissue mass retention following bariatric surgery. Clin Nutr 32: 550-555.
- Pereira AZ, Marchini JS, Carneiro G, Arasaki CH, Zanella MT (2012) Lean and fat mass loss in obese patients before and after Roux-en-Y gastric bypass: A new application for ultrasound technique. Obes Surg 22: 597-601.
- Stegen S, Derave W, Calders P (2011) Physical fitness in morbidly obese patients : Effect of gastric bypass surgery and exercise training 2011: 61-70.
- Alba DL, Wu L, Cawthon PM, Mulligan K, Lang T, et al. (2018) Changes in lean mass, absolute and relative muscle strength, and physical performance after gastric bypass surgery. J Clin Endocrinol Metab. 104: 711-720.
- Vaurs C, Diméglio C, Charras L, Anduze Y, Chalret M, et al. (2015) Determinants of changes in muscle mass after bariatric surgery. Diabetes Metab 41: 416-421.
- Mizrahi I, Beglaibter N, Simanovsky N, Lioubashevsky N, Mazeh H, et al. (2015) Ultrasound Evaluation of Visceral and Subcutaneous Fat Reduction in Morbidly Obese Subjects Undergoing Laparoscopic Gastric Banding, Sleeve Gastrectomy, and Roux-en-Y Gastric Bypass: A Prospective Comparison Study. Obes Surg 25: 959-966.
- Da L (1994) Screening for nutritional status in the elderly. Prim Care 21: 55-67.
- Umeda LM, Pereira AZ, Carneiro G, Arasaki CH, Zanella MT (2013) Postprandial Adiponectin Levels Are Associated with Improvements in Postprandial Triglycerides after Roux-en-Y Gastric Bypass in Type 2 Diabetic Patients. Metab Syndr Relat Disord 2013: 1-6.
- Mcnee M, Levine B (2015) Sonography of muscle : Normal findings and spectrum of abnormalities. Curr Radiol Rep 3: 1-9.
- Heymsfield SB, Gonzalez MC, Lu J, Jia G, Zheng J (2015) Skeletal muscle mass and quality: evolution of modern measurement concepts in the context of sarcopenia. Proc Nutr Soc 74: 355-366.
- Guglielmi CG (2016) Body composition in clinical practice. Eur J Radiol 85: 1461-1468.
- Azagury DE, Ris F, Pichard C, Volonté F, Karsegard L, et al. (2015) Does perioperative nutrition and oral carbohydrate load sustainably preserve muscle mass after bariatric surgery? A randomized control trial. Surg Obes Relat Dis 11: 920-926.
- Sjöström L, Gummesson A, Sjöström CD, Narbro K, Peltonen M, et al. (2009) Effects of bariatric surgery on cancer incidence in obese patients in Sweden (Swedish Obese Subjects Study): A prospective, controlled intervention trial. Lancet Oncol 10:653-662.
Citation: Pereira ZA, Arasaki CH, Umeda LM, Zanella MT (2020) 10 Years Follow-Up after Bariatric Surgery: Body Composition, Weight and Diabetes. J Obes Weight Loss Ther 10: 416. DOI: 10.4172/2165-7904.1000416
Copyright: © 2020 Pereira ZA, et al. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.
Share This Article
Recommended Journals
Open Access Journals
Article Tools
Article Usage
- Total views: 2177
- [From(publication date): 0-2020 - Apr 04, 2025]
- Breakdown by view type
- HTML page views: 1427
- PDF downloads: 750