Non-Hodgkin's Lymphoma of Kidney, Presenting as a Solid Mass: Case Report
Received: 18-Apr-2012 / Accepted Date: 16-Jul-2018 / Published Date: 18-Jul-2012 DOI: 10.4172/2161-0681.1000117
Abstract
Abstract
It is a common occurrence of bilateral renal involvement in high grade lymphomas. Primary renal lymphoma is a
rare event, it is a debated issue because of absence lymphoid tissue in normal kidney. Secondary renal involvement in
systemic lymphomas is generally present as multiple masses, but they may present as a solitary nodule.
This case was a 70-years old woman, and she had complaints of pain in right flank and abdomen for two months.
In laboratory examination in urology outpatient clinics she had prolonged bleeding time, high coagulation factors, low
thrombocytes, and no atypical cells in peripheric blood smear. In abdominopelvic computerized tomography it was
detected a mass in right kidney, and she underwent a right nephrectomy. Our case presented as a renal tumor, and it
was diagnosed as non-Hodgkin’s lymphoma, diffuse large B cell type.
Because of rarity of primary renal lymphoma and its debated origin we presented this case.
Introduction
Bilateral renal involvement is a common event in rapidly progressing hematological malignancies like high grade lymphomas and acute leukemias [1]. Widespread infiltration of the kidney is present in almost one-third of patients with lymphoma at autopsy. Primary Renal Lymphoma ( PRL) is a rather rare entity, because this organ is normally free of lympoid tissue [1,2]. PRL comprises only 0.7% of extranodal lymphomas [3]. PRL is commonly seen in middle-aged people [4], and in its etiology it is blamed acquired immune deficiencies and EBV infections [5]. Renal involvement with lymphoma occurs commonly with Non-Hodgkin’s Lymphoma (NHL). The majority of patients have intermediate or high grade lymphomas, most of them of B-cell origin [3].
Our case presented as a renal tumor. Because of rarity of primary renal lymphoma and its debated origin we presented this case.
Case
70 years-old woman applied to hospital because of pain in right flank and abdomen lasting for two months. In her medical history there were cholesistectomy performed 13 years ago, hypertension, and asthma. The laboratory findings in the beginning as follows: WBC= 4.26 k/ul (4.60-10.20), NE%=60.7 (37.0-80.0), LY%=20.8 (10.0-50.0), Hgb=13 g/dl (12.2-18.1), Hct=%36.1 (37.7-53.7), MCV=83.8 fl (80.0- 97.0), PLT=36 k/ul (142-424), PTR=15.2 (10.0-14.5), blood urea, kreatinin and electrolyte levels were normal. In urine it was negative protein, leukocyte and erythrocyte. She was asked for a hematological consultation, and in her peripheral blood smear it was detected pseudothrombocytopenia, and no atypical cells. She had prolonged bleeding time, high coagulation factors, low thrombocytes.
In Abdominopelvic Computerized Tomographical (CT) examination it was detected a hypervascular mass in lower pole of right kidney, measuring 127×97 mm, invasing the hilus, and perinephritic adipose tissue. Right renal artery was surrounded by lymph nodes in its middle part. Renal veins were patent. In aortocaval region it was seen a mass measuring 125×95×5 mm, possibly representing conglomerated lymph nodes. Spleen length was 15 cm, and larger than normal. Both adrenal glands and left kidney were normal. In positron emission tomography (PET) increased F-2-fluoro-2-deoxy-D-glucose (FDG) was detected in upper paratracheal, subcarineal, left hilar, right retrocrural, and right iliac lymph nodes.
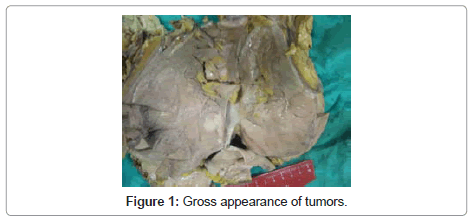
She underwent a right nephrectomy. In gross examination it was seen a kidney measuring 24×11.5×10.5 cm, and no adrenal gland . After cut-sectioning tumor was seen in lower pole, invasing perirenal adipose tissue and reaching to Gerota’s fascia, pushing pelvis renalis, measuring 12.5×10×10 cm, appearing as a fleshy mass (Figure 1). In addition to nephrectomy specimen, lymph nodes were separetely sent, measuring largest one being 6×4×3 cm; their cut sections revealed solid, gray structure, and focal hemorrhage.
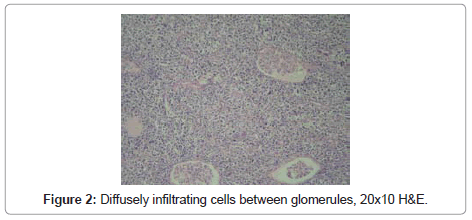
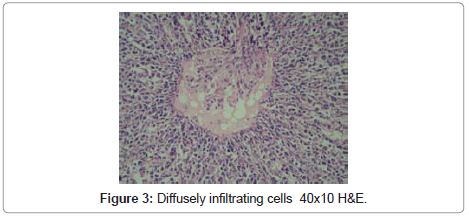
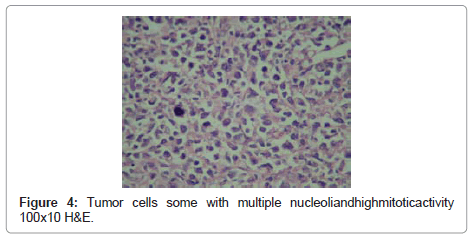
In microscopical examination, tumor was detected as diffusely infiltrating cells between glomerules and tubules, and having no organization. Tumor cells had vesiculated, sometimes hyperchromatic nuclei, some with multiple nucleoli, and high mitotic activity (Figure 2-4). Tumor invaded perirenal adipose tissue. There was no tumor in ureter and renal vein. In sections of lymph nodes tumor cells were detected having similar morphology. Nonneoplastic kidney revealed no discernible pathology.
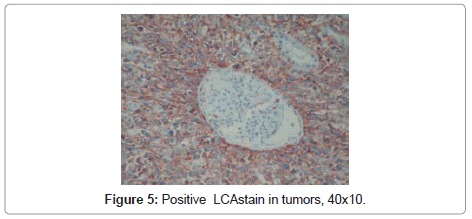
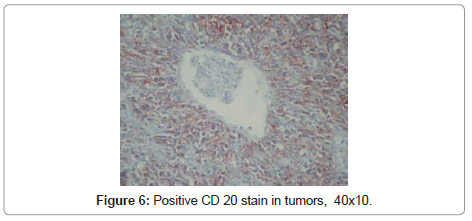
In differential diagnosis renal cell carcinoma, angiomyolipoma, synovial sarcoma, vascular tumors, smooth muscle tumors, malignant fibrous histiocytoma were considered. In immunohistochemical examination it was positive for vimentin, leukocyte common antigen (LCA), CD 20 (Figure 5,6) and CD 43, and negative for pan cytokeratin, epitelial membran Ag (EMA), HMB 45, Melan A, S 100, smooth muscle actin (SMA), desmin, CD 34, CD 99, bcl2, CD 68, CD 30 and CD 3. Case was reported as non-Hodgkin’s lymphoma, diffuse large B cell type (NHLDLBCs) based on morphological and immunohistochemical findings.
Our case was accepted as secondary renal involvement of systemic lymphoma. She was given four cycles of CHOP protocol, she developed a neutropenic fever, and treatment was cancelled. She died four months after operation. An autopsy was not performed because her relatives denied to give a permission for autopsy.
Discussion
NHLDLBC comprises 25-30% of adult non-Hodgkin’s lymphomas, commonly seen in 7th decade and males are more prevalent [6]. Secondary renal lymphomas are more common 30 times than primary lymphomas [7]. In autopsy series secondary renal involvement in systemic lymphomas is reported up to 30-60% of patients [8]. This percentage is reported as 3-15% in CT, performed for lymphoma staging [8,9]. The discrepancy between CTs and autopsies is explained rarity of biopsy and nephrectomies in renal lymphomal involvement [9]. PRL is a rather rare entity and it is a debated issue because of absence lymphoid tissue in normal kidney [2]. It was proposed that lymphatics in renal capsule may be origin of lesions, or chronic inflammation may cause to lymphomas [5]. In present case there was no chronic pyelonephritis in remaining nonneoplastic kidney.
Kidneys are generally involved in high grade lymphomas, presenting with nonspesific symptoms, diameter of lesions ranges between 1 and 20 cm [8]. Our case was 12.5 cm in diameter. In CT exams renal lymphomas generally presents as bilateral multiple masses, less often as solitary lesion with retroperitoneal invasion. Present case was a solitary lesion, but there were also perirenal adipose tissue and Gerotal invasion. In literature it was reported diffuse, large conglomerated adenopathies, but no vascular invasion [8]. We also did not find any vascular invasion.
Some reservations are proposed to make a PRL diagnosis [5]: 1. Presence of a renal mass, 2. Absence of lymph node invasion and other visceral invasion at the time of diagnosis, 3. Absence of myelosuppresion and absence of a leukemic blood picture. However some cases reported as PRL without second or third condition [2,4,9].
Yasunaga et al. [5] reported an eight-case PRL series, six of being NHLDLBC, none of cases presented lymphadenopathy or hepatosplenomegaly at the time of diagnosis. Mean survival time was six months, in autopsies only one case was limited to kidney, others with extrarenal visceral invasion. In our case in CT exam in aortocaval region it was seen a mass measuring 12, 5x9, 5x5 cm, possibly representing conglomerated lymph nodes. Spleen length was 15 cm, and larger than normal. Both adrenal gland and left kidney were normal. In Positron Emission Tomography (PET) increased FDG was detected in upper paratracheal, subcarineal, left hilar, right retrocrural, and right iliac lymph nodes. Our case was accepted as secondary renal involvement of systemic lymphoma.
In the literature it was reported that PRLs may simulate renal carcinomas both radiologically and pathologically [10]; it may present as a solitary mass in 10-20% of cases [11], and perirenal invasion in 10% of cases. In our case because of tumor’s presence as a solitary mass renal carcinoma was included in differential diagnosis; angiomyolipoma, synovial sarcoma, and smooth muscle tumor because of localization and perirenal adipose invasion. In additon to morphological findings, positivity of LCA and CD20 directed to correct diagnosis of lymphoma.
In Airaghi’s article [12] in a patient with cold agglutinin disease and hypercoagulation it was reported lymphoma in kidney and adrenal gland. At the time of diagnosis there were no mediastinal and paraaortic lymph nodes, but after diagnosis bone and lymph node involvement were detected in PET-CT exams. Case was accepted as PRL.
Pinggera et al. [2] reported a solitary renal mass invading Gerota’s fascia, without blood abnormalities. In this case in mediastin and retroperitoneum there were lymph nodes with borderline size. This case was accepted as possible PRL.
Alonso et al. [9] reported three cases with solitary masses, one paraaortic, one retrocaval conglomerated lymph nodes, and one patient with invasion of renal vein and perirenal adipose tissue. All cases were accepted as PRL, NHLDLBC.
It was said that it must be determined no neoplastic proliferation using bone marrow biopsies,or bone scintigraphy and periperal blood smears in order to give a PRL diagnosis. Most patient are at stage 4, and their prognoses are bad [4]. There are some debate on whether it is a primary event or origin of a rapidly progressing sysyemic disease. In studies it was said that either extrarenal disease couldn’t definetely diagnosed or absence of enough postmortem studies [9]. It was also stressed that PRL is highly aggressive and rapidly invades systemic lymphatic tissue.
In short there were no concordance between researchers [2,9]. Some studies stresses absence of lymph node involvement and leukemic blood picture to make a PRL diagnosis [4,5,12]. But in other studies, although concurrent lymph node involvement alongside with a solitary renal mass, is accepted PRL. In addition they insisted either extrenal disease is not full fledged or absence of postmortem investigations and they said that PRL is a rapidly progressive disease (From renal to lymph node), so that it is not possible to determine whether its primary or secondary in the very beginning of the disease. Primary or not both can make solid or bilateral involvement, moreover their treatment is similar [13].
Our case, despite the absence of leukemic blood picture, was regarded as systemic involvement because of presence of lymph nodes.
Conclusion
In conclusion renal lymphoma may present as a solitary mass whether primary or not, and it must be kept in mind in the differential diagnosis of renal tumors.
References
- Monfared A, Orangpoor RO, Fakheri TF, Falahatkar S (2009) Acute renal failure and bilateral kidney infiltration as the first presentation of non-Hodgkin lymphoma. Iran J Kidney Dis 3: 50-53.
- Pinggera GM, Peschel R, Buttazzoni A, Mitterberger M, Friedrich A, et al. (2009) A possible case of primary renal lymphoma: a case report. Cases J 2: 6233.
- Qui L, Unger PD, Dillon RW, Strauchen JA (2006) Low-grade mucosa-associated lymphoid tissue lymphoma involving the kidney: report of 3 cases and review of the literature. Arch Pathol Lab Med 130: 86-89.
- Olusanya AA, Huff G, Adeleye O, Faulkner M, Burnette R, et al. (2003) Primary renal non-Hodgkins lymphoma presenting with acute renal failure. J Natl Med Assoc 95: 220-224.
- Yasunaga Y, Hoshida Y, Hashimoto M, Miki T, Okuyama A, et al. (1997) Malignant lymphoma of the kidney. J Surg Oncol 64: 207-211.
- Swerdlow SH, Campo E, Haris NL, Jaffe ES, Pileri SA, et al. (2008) World Health Organization Classification of tumours of haematopoietic and lymphoid tissues, fourth edition. Lyon, IARC Press 233-237.
- Eble JN, Sauter G, Epstein JI, Sesterhenn IA (2004) World Health Organization Classification of tumours . Pathology and Genetics of Tumours of the Urinary System and Male Genital Organs. Lyon IARCPress 2004: 85-86.
- Urban BA, Fishman EK (2000) Renal lymphoma: CT patterns with emphasis on helical CT. Radiographics 20: 197-212.
- O’Sullivan AW, Lee G, Fitzgerald E, O’Sullivan GC (2003) Bilateral primary renal lymphoma. Ir J Med Sci 172: 44-45.
- Omer HA, Hussein MR (2007) Primary renal lymphoma. Nephrology 12: 314-315.
- Francualdo Barreto, Marcos F Dall Oglio , Miguel Srougi (2006) Renal lymphoma. a typical presentation of a renal tumor. Int Braz J Urol 32: 190-192.
- Airaghi L, Greco I, Carrabba M, Barcella M, Baldini IM, et al. (2006) Unusal presentation of large B cell lymphoma: a case report and review of literature. Clin Lab Haem 28: 338-342.
- Vázquez Alonso F, Sánchez Ramos C, Vicente Prados FJ, Pascual Geler M, Ruiz Carazo E, et al. (2009) Primary renal lymphoma: report of three new cases and literature review. Arch Esp Urol 62: 461-465.
Citation: Celik A, Yildiz Y, Özekinci S, Mizrak B (2012) Non-Hodgkin’s Lymphoma of Kidney, Presenting as a Solid Mass: Case Report. J Clin Exp Pathol 2:117. DOI: 10.4172/2161-0681.1000117
Copyright: © 2012 Celik A, et al. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.
Share This Article
Recommended Journals
Open Access Journals
Article Tools
Article Usage
- Total views: 21622
- [From(publication date): 7-2012 - Dec 19, 2024]
- Breakdown by view type
- HTML page views: 17056
- PDF downloads: 4566